1. Antiplatelet drugs work by inhibiting platelet aggregation which is essential for forming blood clots. They are used to prevent thrombus formation in certain pathological conditions.
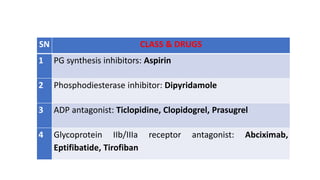
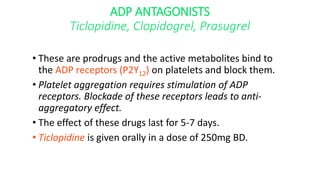
2. There are several classes of antiplatelet drugs including aspirin, clopidogrel, abciximab which work via different mechanisms such as inhibiting thromboxane A2, blocking ADP receptors, or inhibiting the glycoprotein IIb/IIIa receptor.
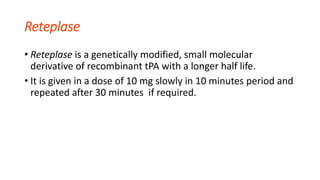
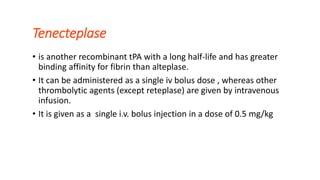
3. Fibrinolytics like streptokinase, alteplase work by activating plasminogen to plasmin to break down fibrin clots and are indicated for pulmonary embolism, myocardial infarction, and ischemic stroke. The major risks are bleeding complications.