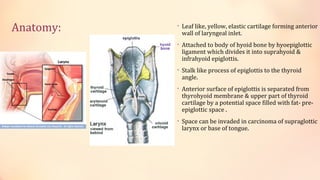
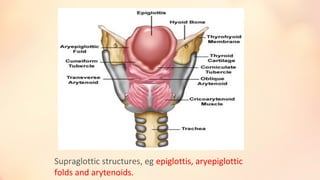
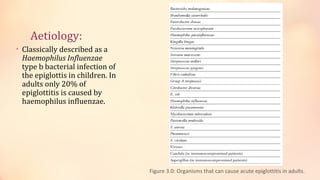
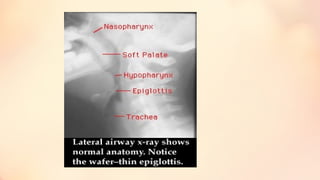
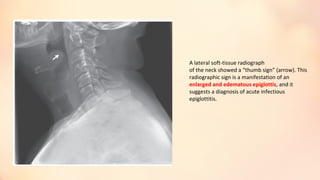
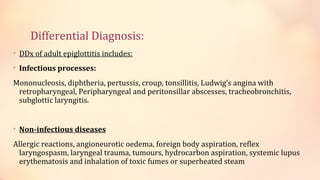
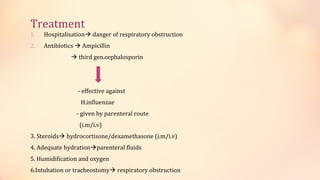
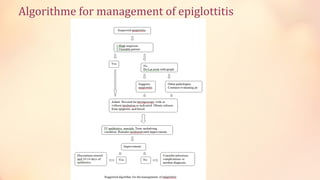
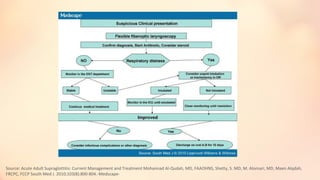
The document summarizes acute epiglottitis, an inflammatory condition of the supraglottic structures including the epiglottis, aryepiglottic folds, and arytenoids that can cause airway obstruction. It describes the anatomy of the epiglottis, causes including H. influenzae infection, symptoms of sore throat and difficulty swallowing, signs of fever and swelling of the epiglottis, diagnosis through examination and imaging, complications of spread of infection, treatment with antibiotics, steroids, and intubation if needed, and good prognosis with timely treatment but risk of sudden airway obstruction.