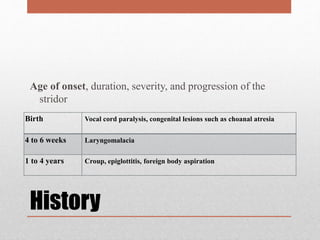
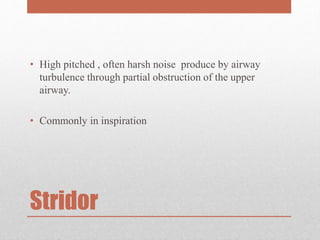
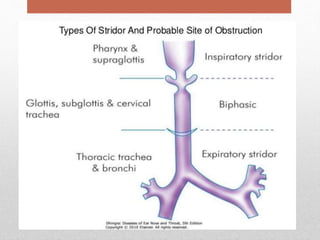
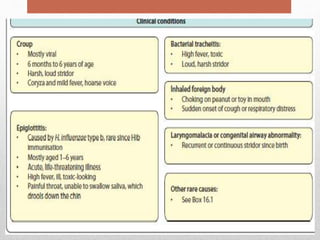
1. A 2-year-old child presented with stridor and was diagnosed with laryngomalacia based on age of onset and examination findings.
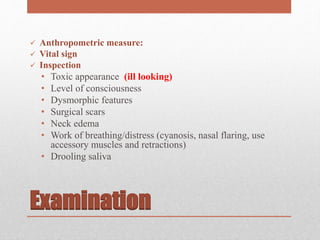
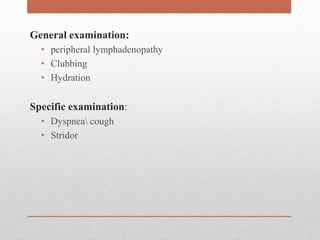
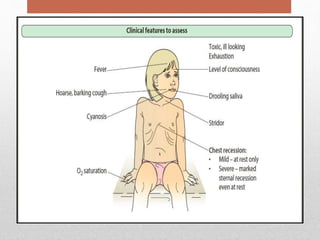
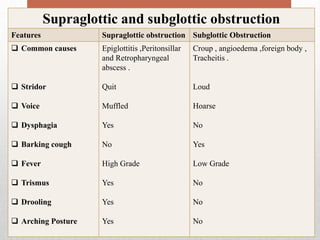
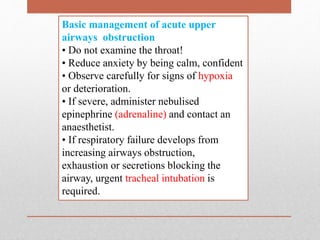
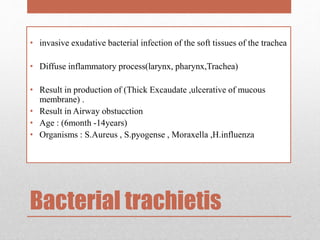
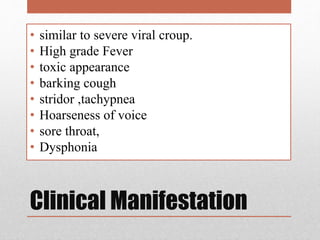
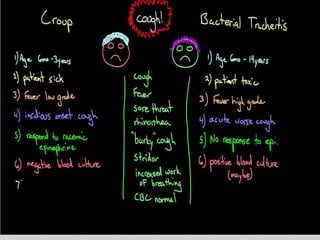
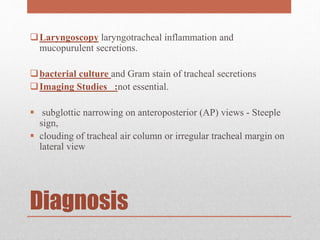
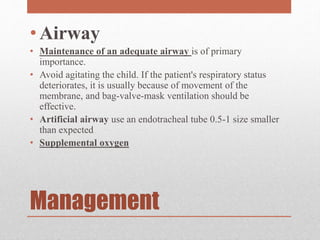
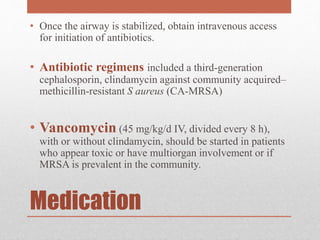
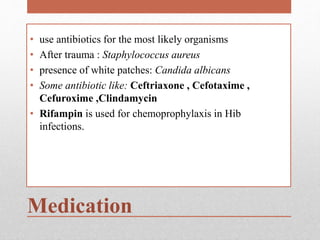
2. Bacterial tracheitis causes upper airway obstruction in children aged 6 months to 14 years and is characterized by high fever, toxic appearance, and barking cough. It requires antibiotics and airway management.
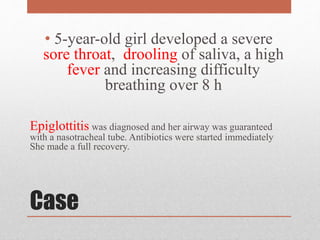
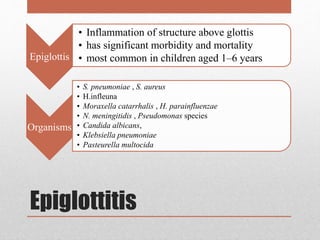
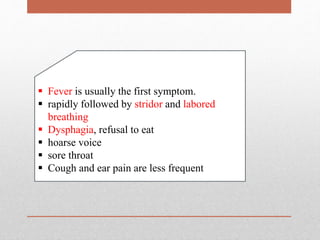
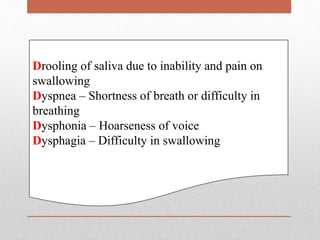
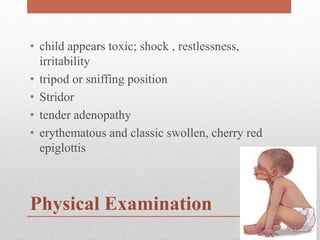
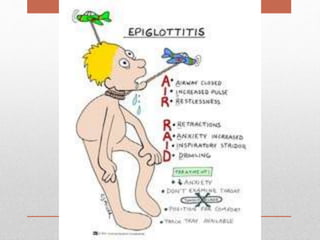
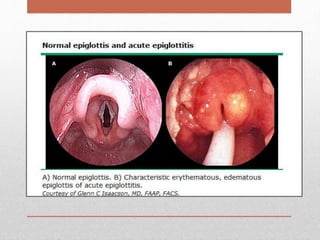
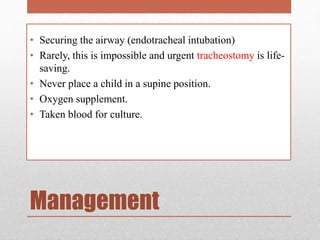
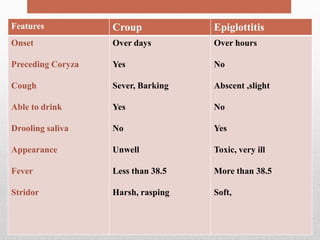
3. Epiglottitis is a medical emergency that causes sudden upper airway obstruction in young children. It presents with fever, drooling, dysphagia, and a toxic appearance, and requires securing the airway with intubation.