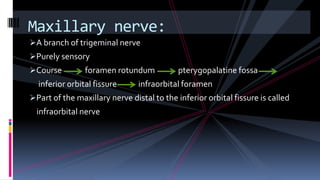
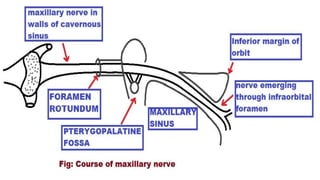
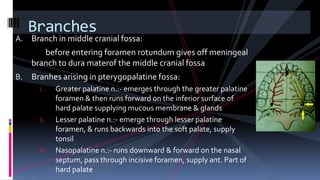
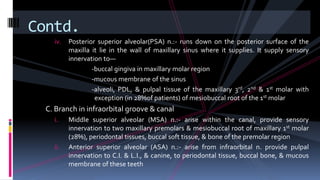
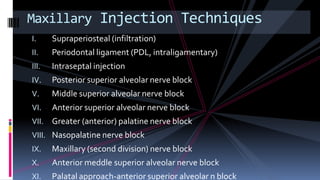
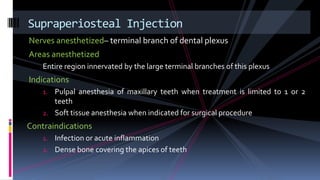
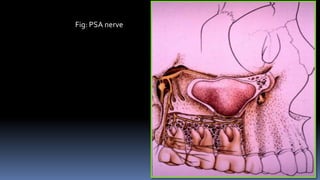
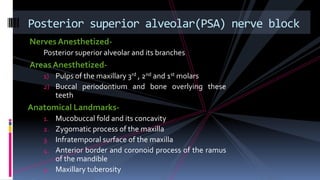
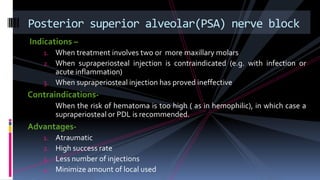
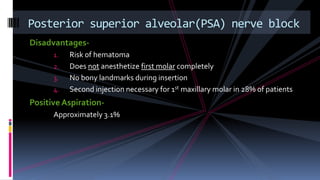
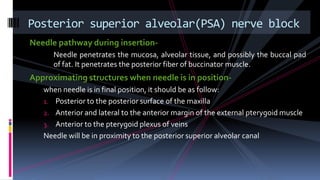
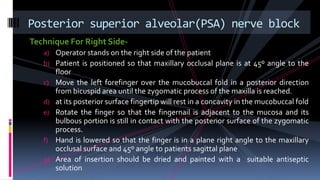
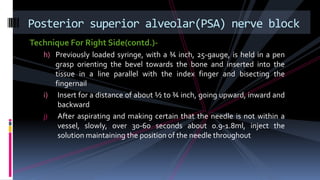
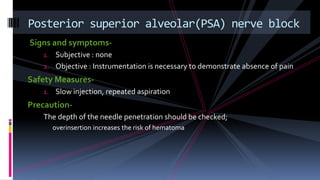
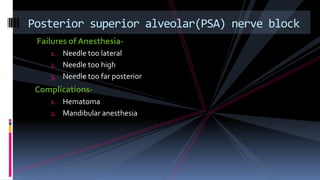
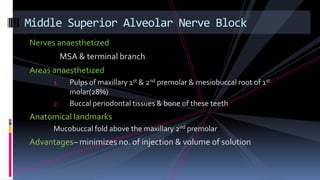
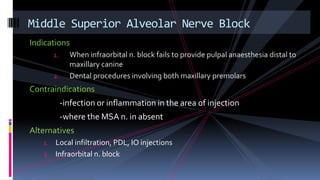
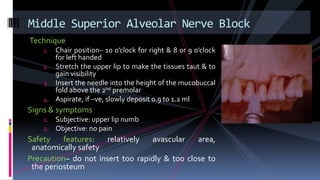
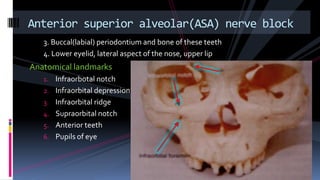
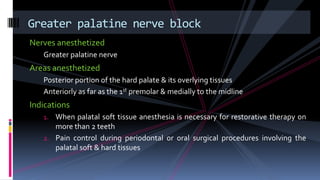
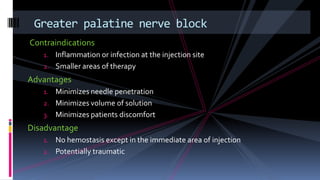
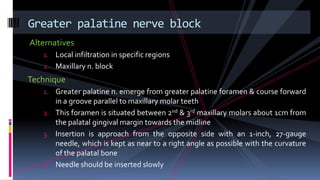
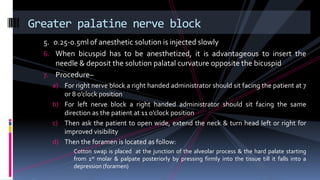
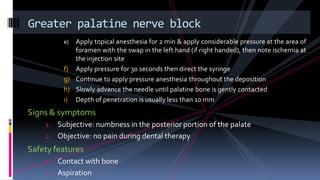
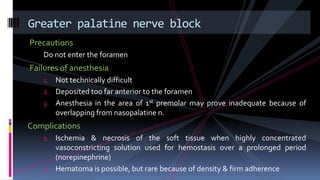
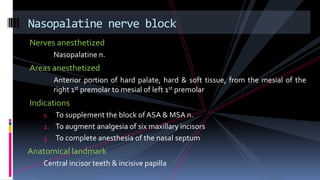
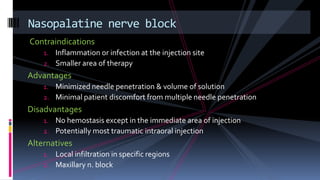
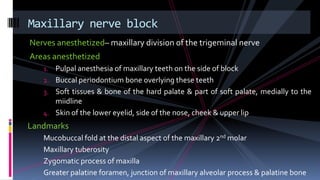
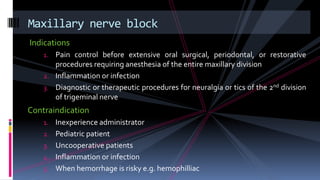
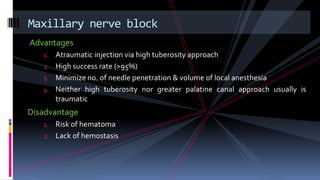
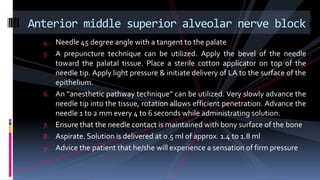
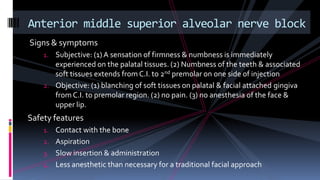
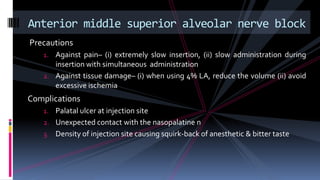
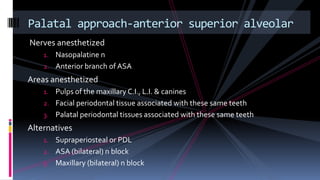
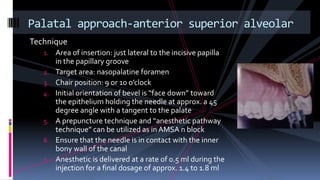
This document provides information on maxillary anesthesia techniques. It discusses the anatomy of the maxillary nerve and its branches that innervate the maxilla. Several injection techniques are described including posterior superior alveolar nerve block, middle superior alveolar nerve block, anterior superior alveolar nerve block, and greater palatine nerve block. Each technique lists the nerves anesthetized, areas anesthetized, indications, contraindications, and steps for administration. Complications and alternatives are also noted for some techniques.