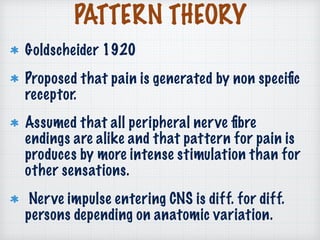
The document presents a comprehensive overview of pain in dentistry, covering its definitions, historical theories, and neurophysiological aspects. It discusses various etiological classifications of orofacial pain, including dental and non-dental origins, as well as diagnostic approaches to evaluate pain characteristics. Additionally, it outlines treatment methods, both pharmacological and non-pharmacological, for managing acute and chronic orofacial pain.