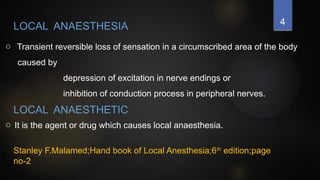
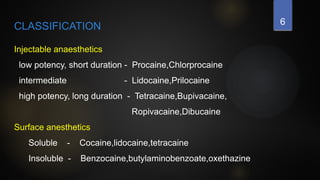
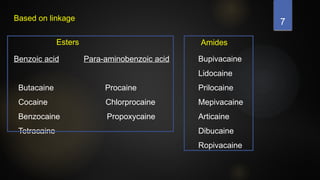
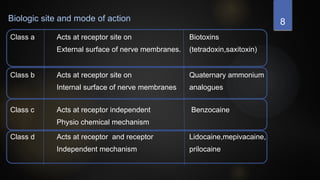
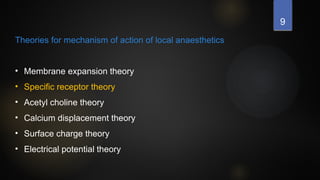
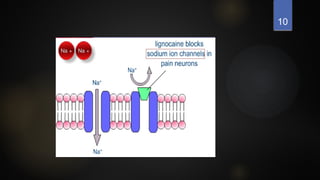
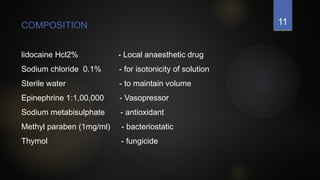
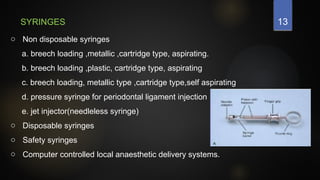
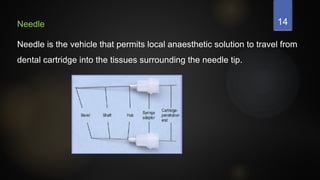
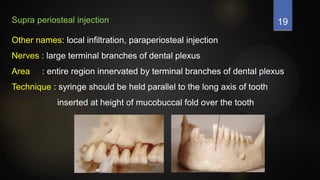
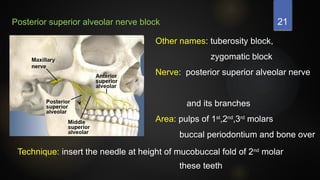
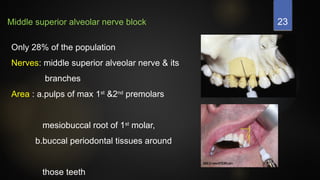
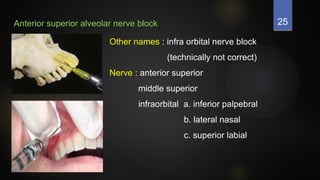
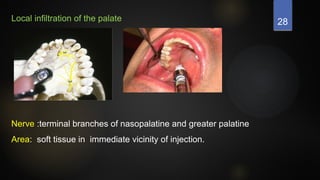
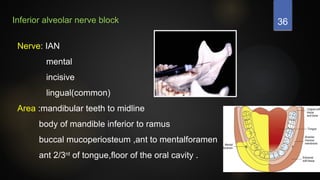
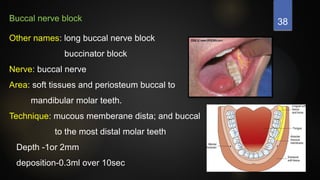
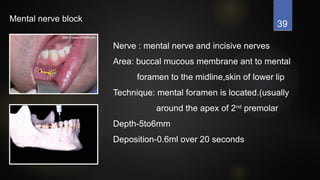
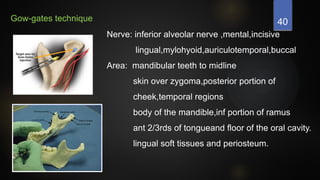
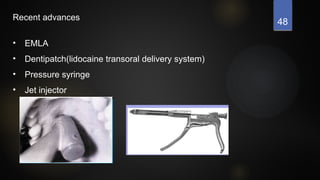
The document provides a comprehensive overview of local anaesthesia, including its definitions, classifications, mechanisms of action, techniques, and potential complications. It delineates various local anaesthetic agents, their compositions, and offers procedural guidelines for administering local anaesthesia in maxillary and mandibular regions. Additionally, it discusses complications that may arise from local anaesthetic use and recent advances in the field.