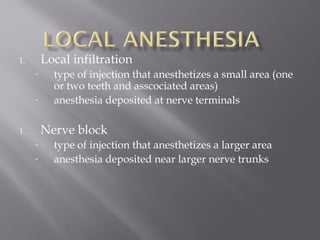
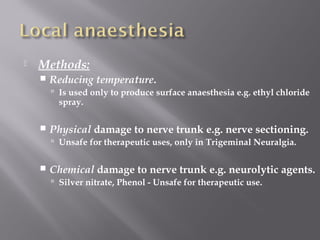
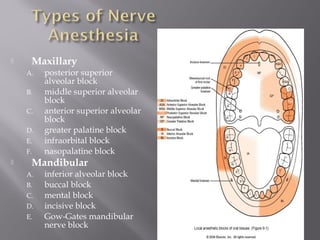
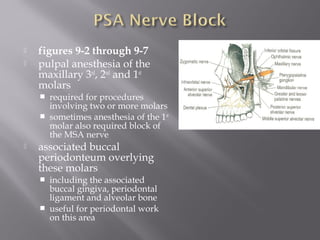
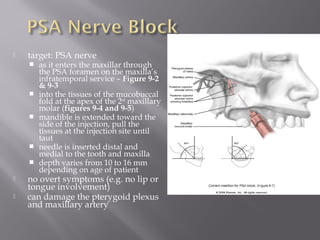
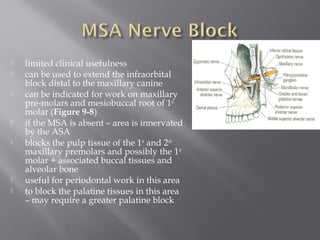
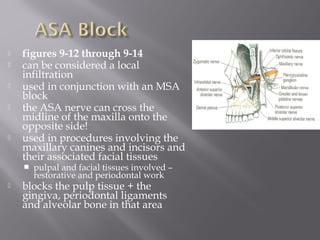
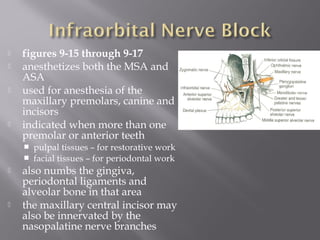
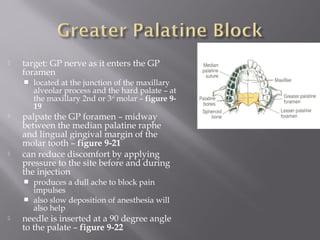
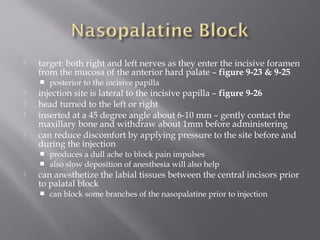
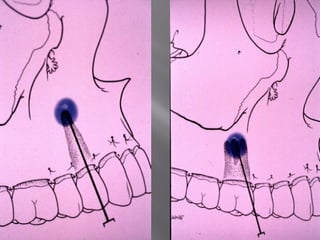
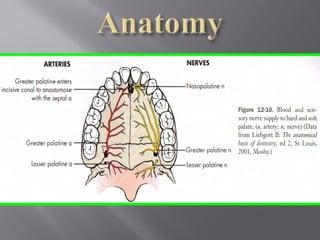
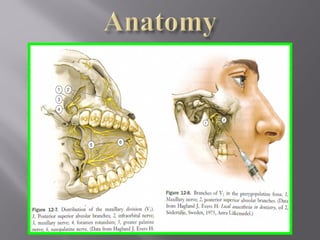
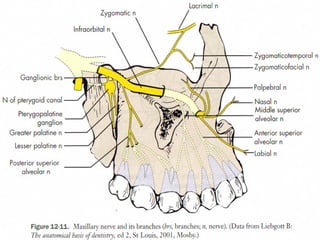
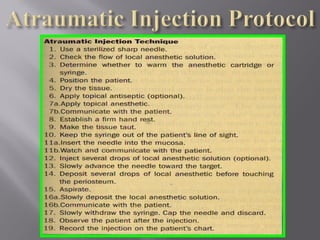
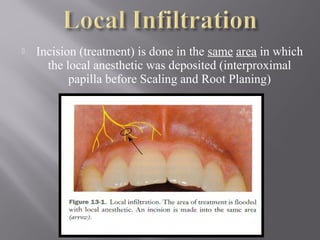
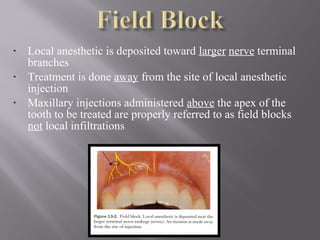
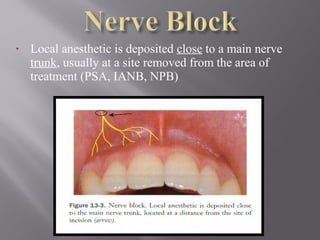
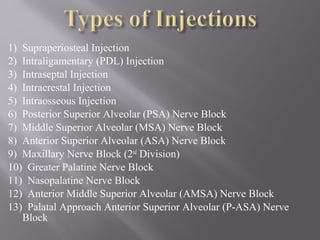
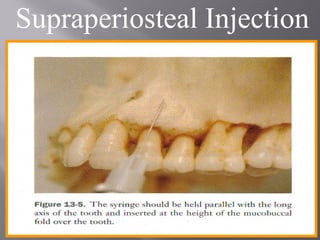
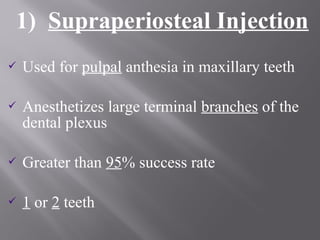
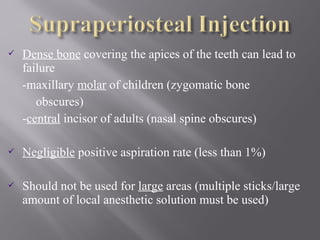
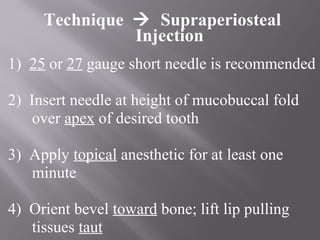
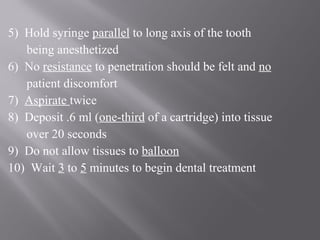
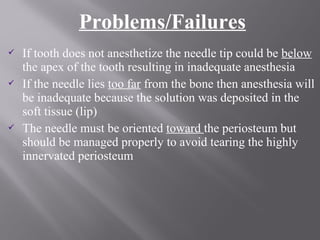
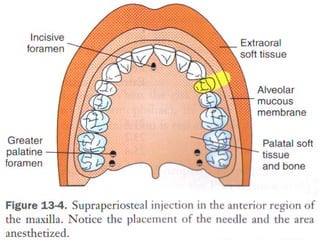
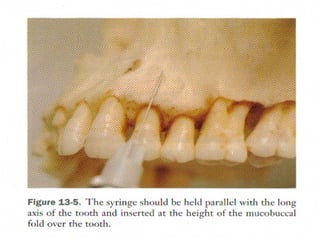
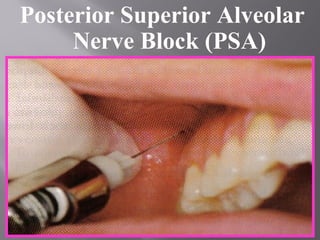
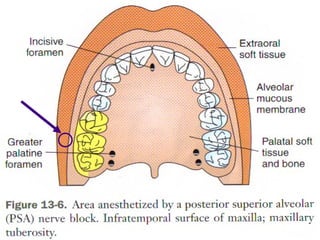
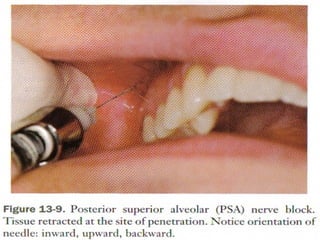
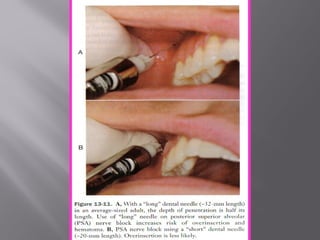
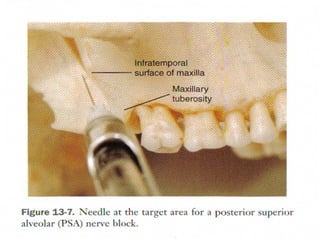
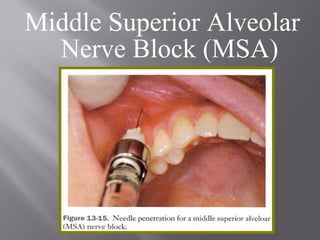
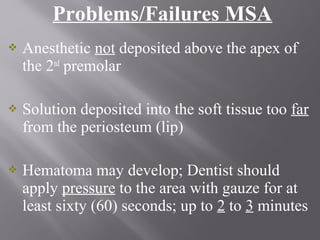
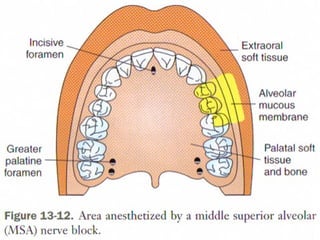
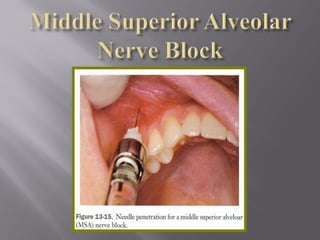
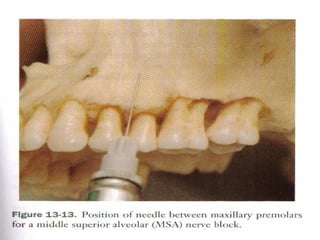
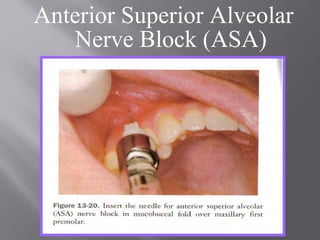
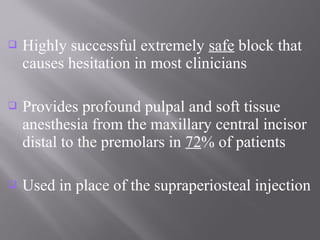
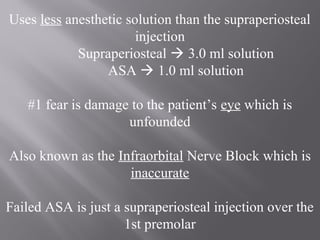
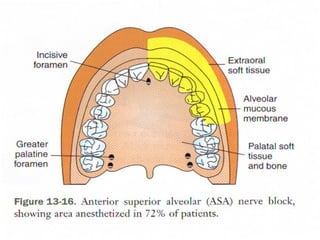
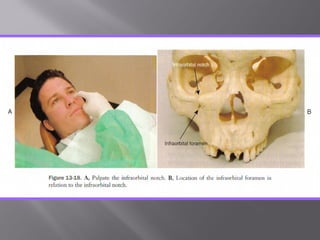
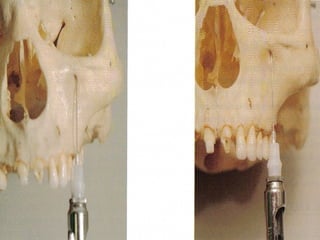
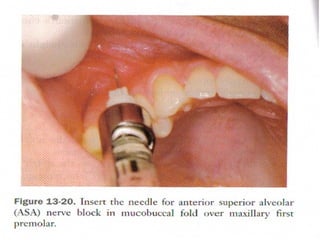
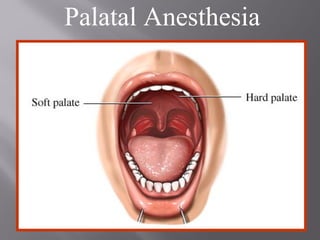
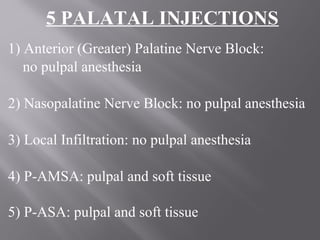
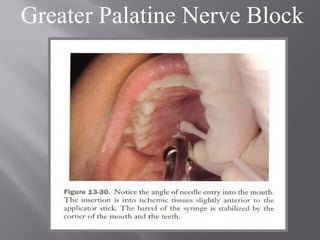
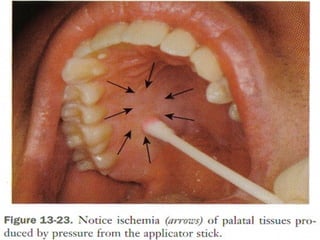
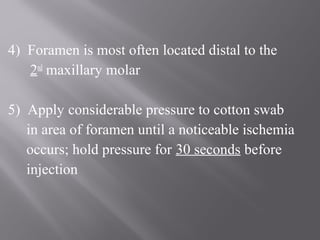
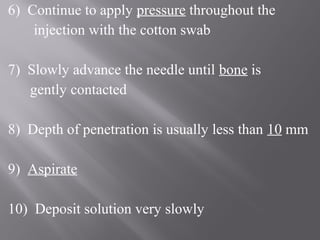
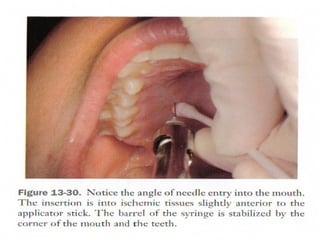
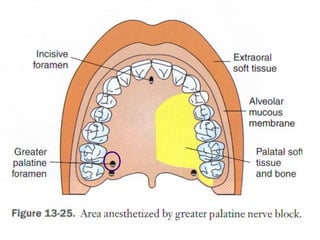
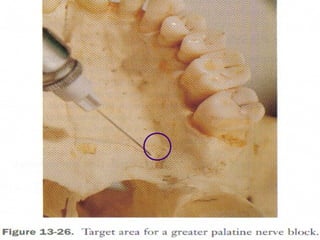
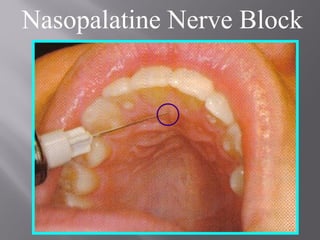
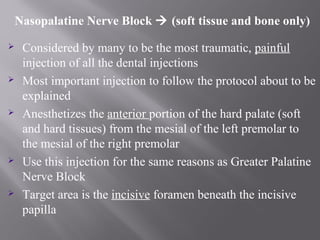
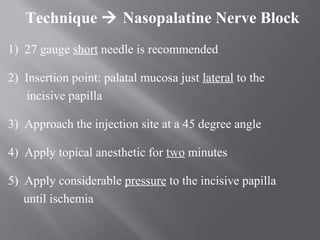
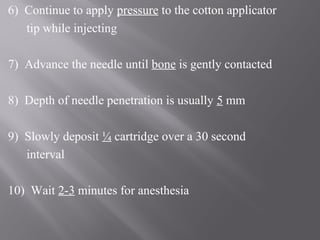
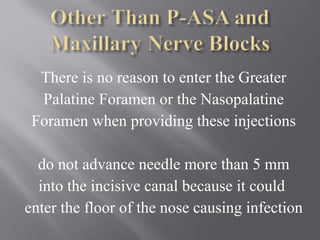
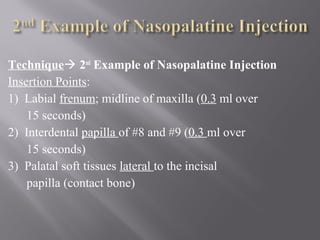
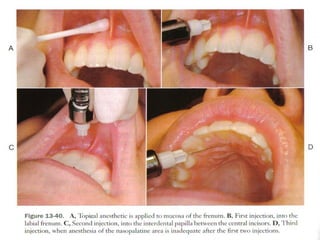
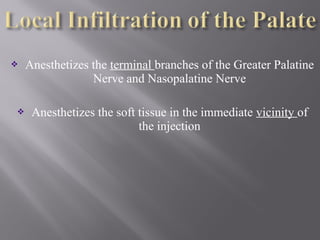
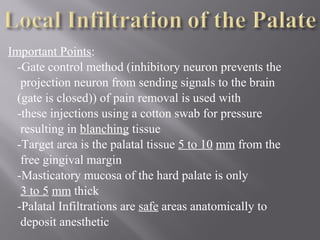
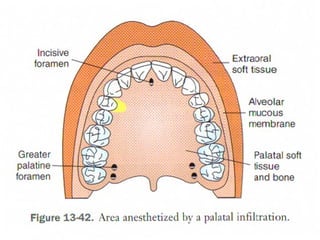
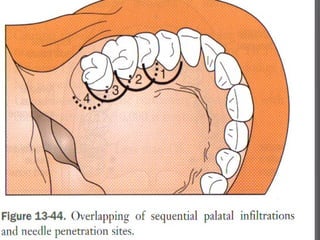
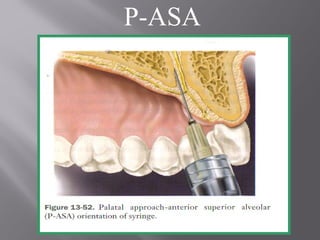
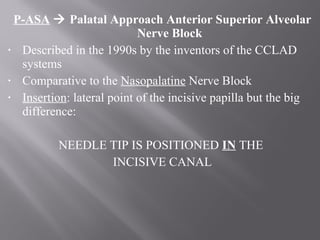
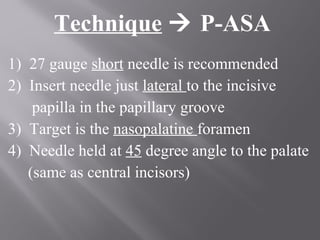
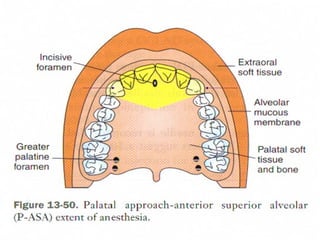
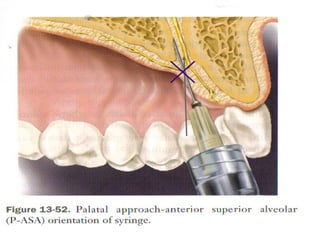
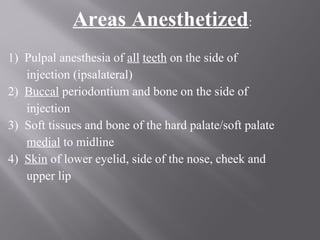
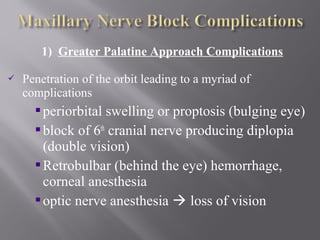
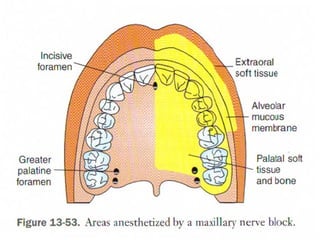
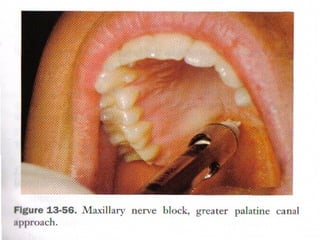
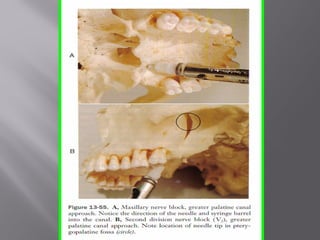
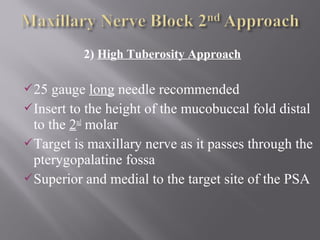
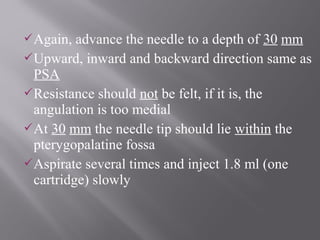
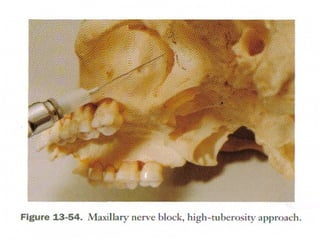
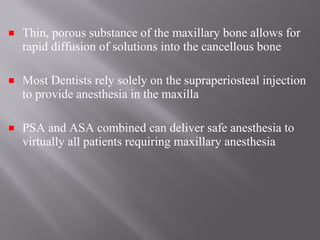
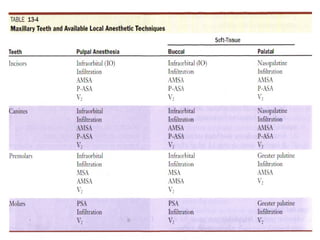
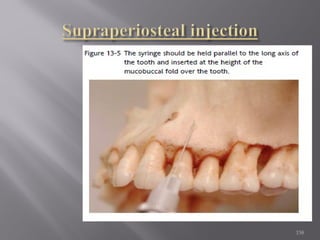
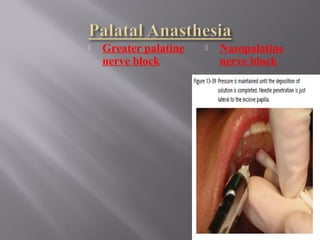
The document discusses various types of dental injections including local infiltration, nerve blocks, and field blocks. It provides details on specific injections for the maxilla, such as the posterior superior alveolar nerve block, which is used to anesthetize the maxillary first, second, and third molars. The document describes injection techniques, target areas, and expected outcomes for different maxillary injections.