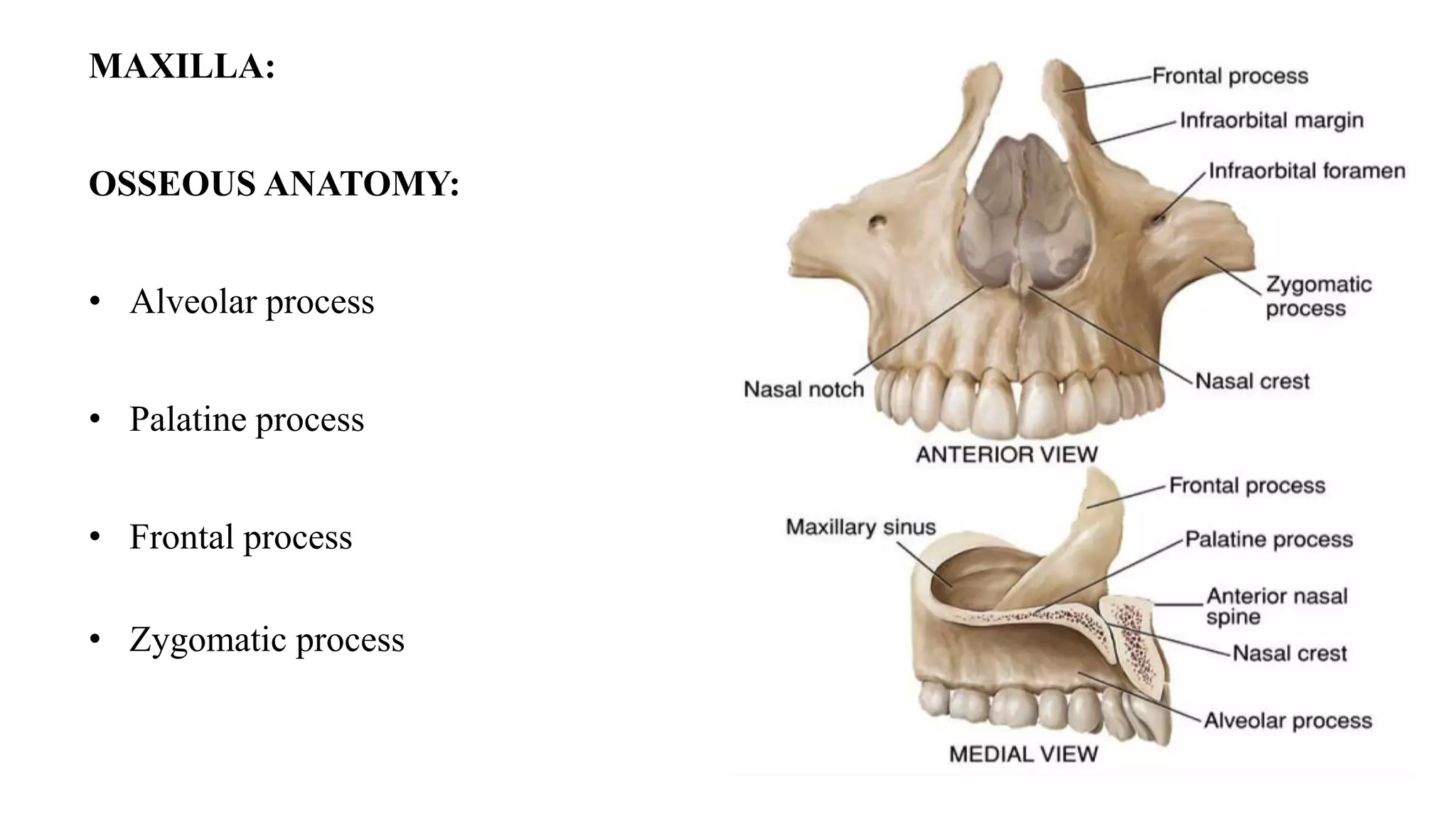
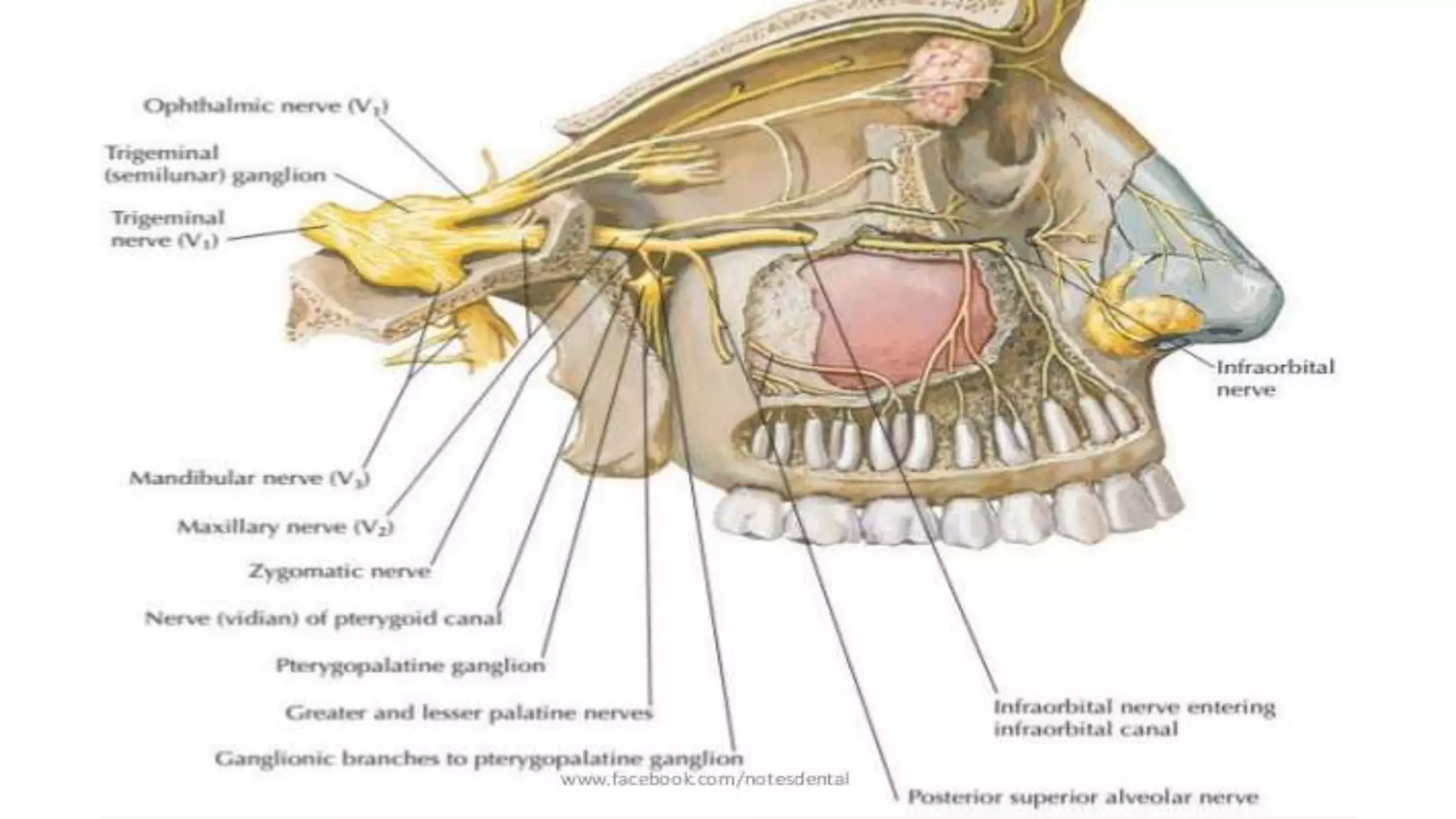
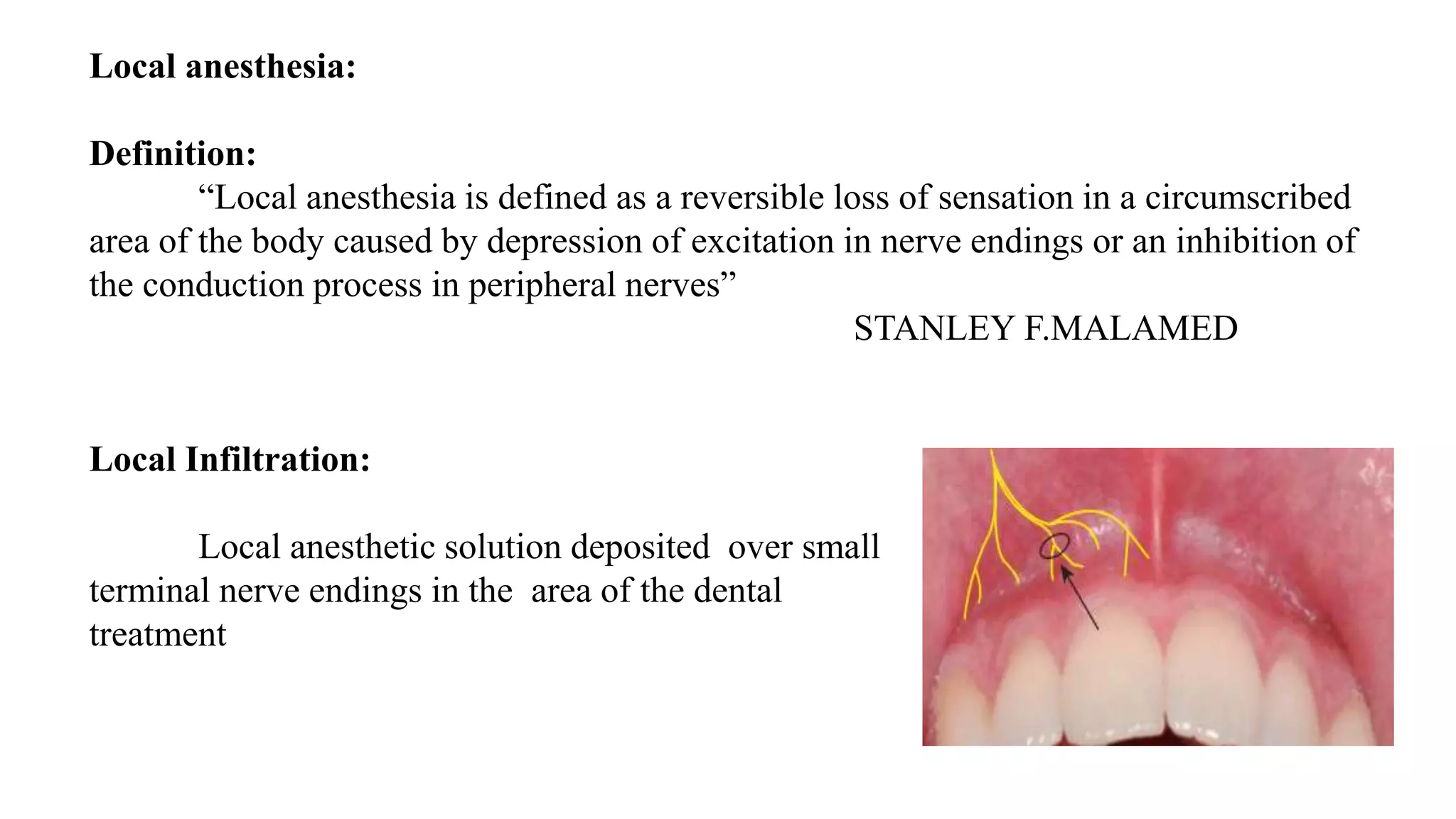
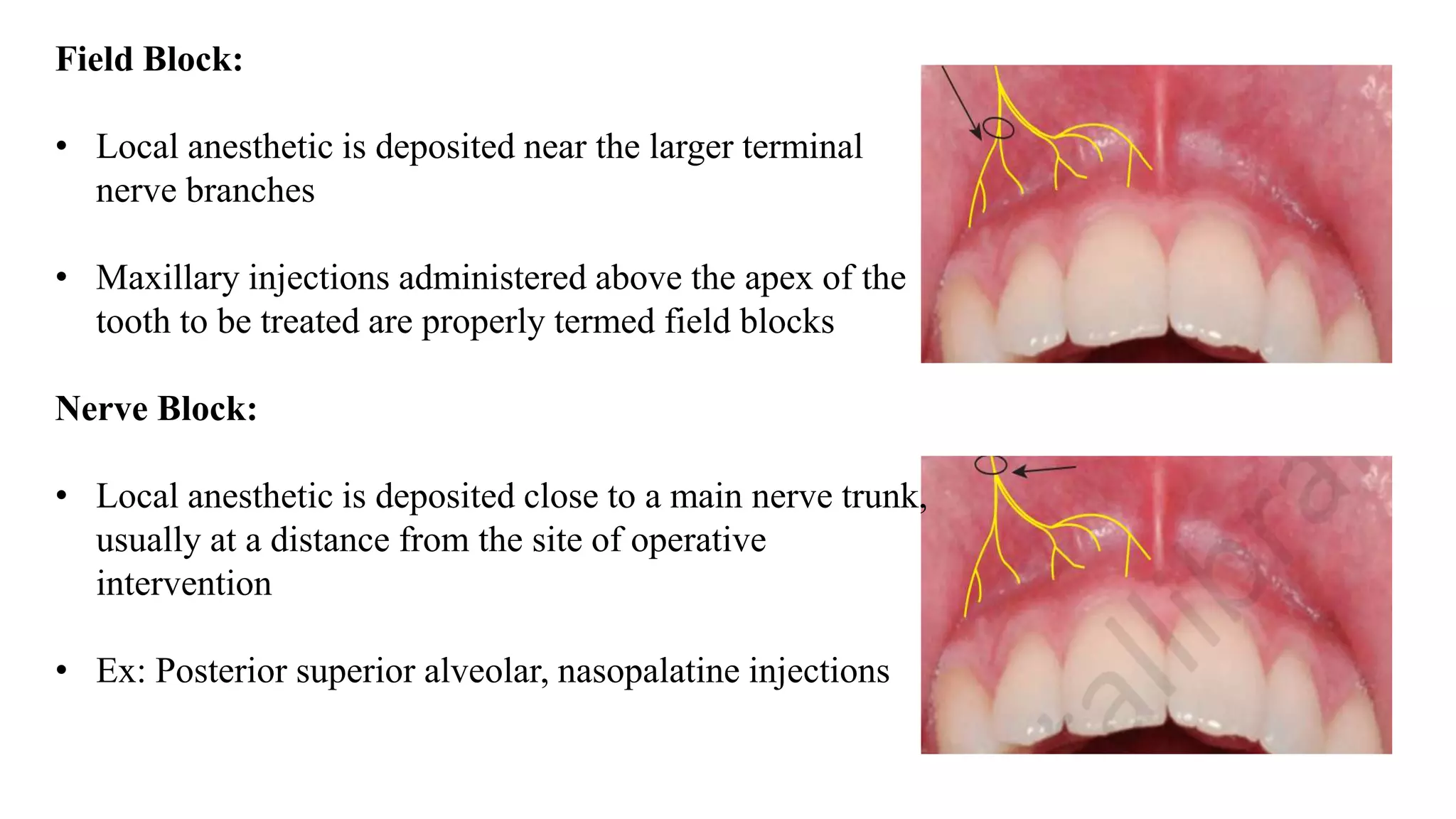
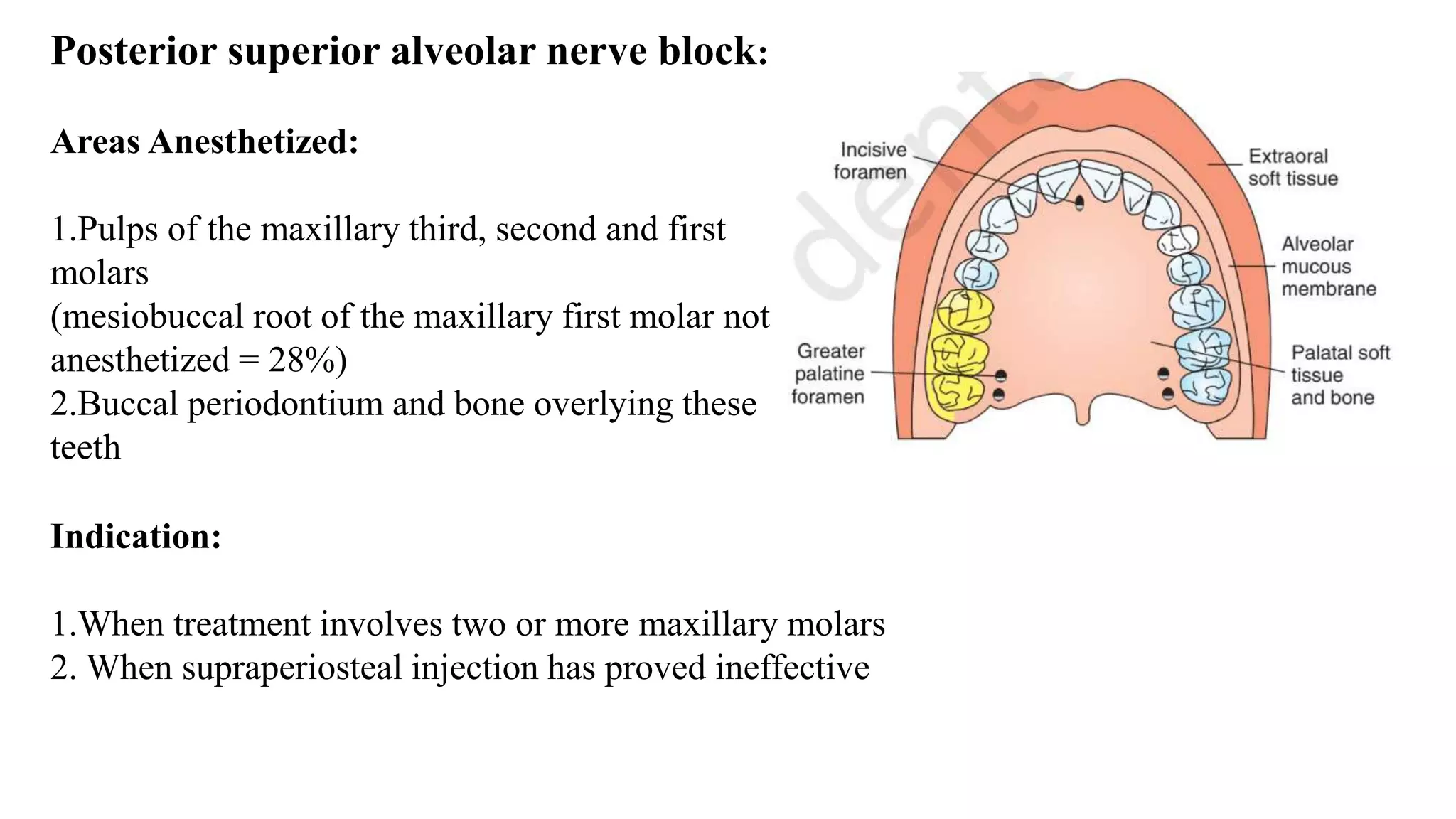
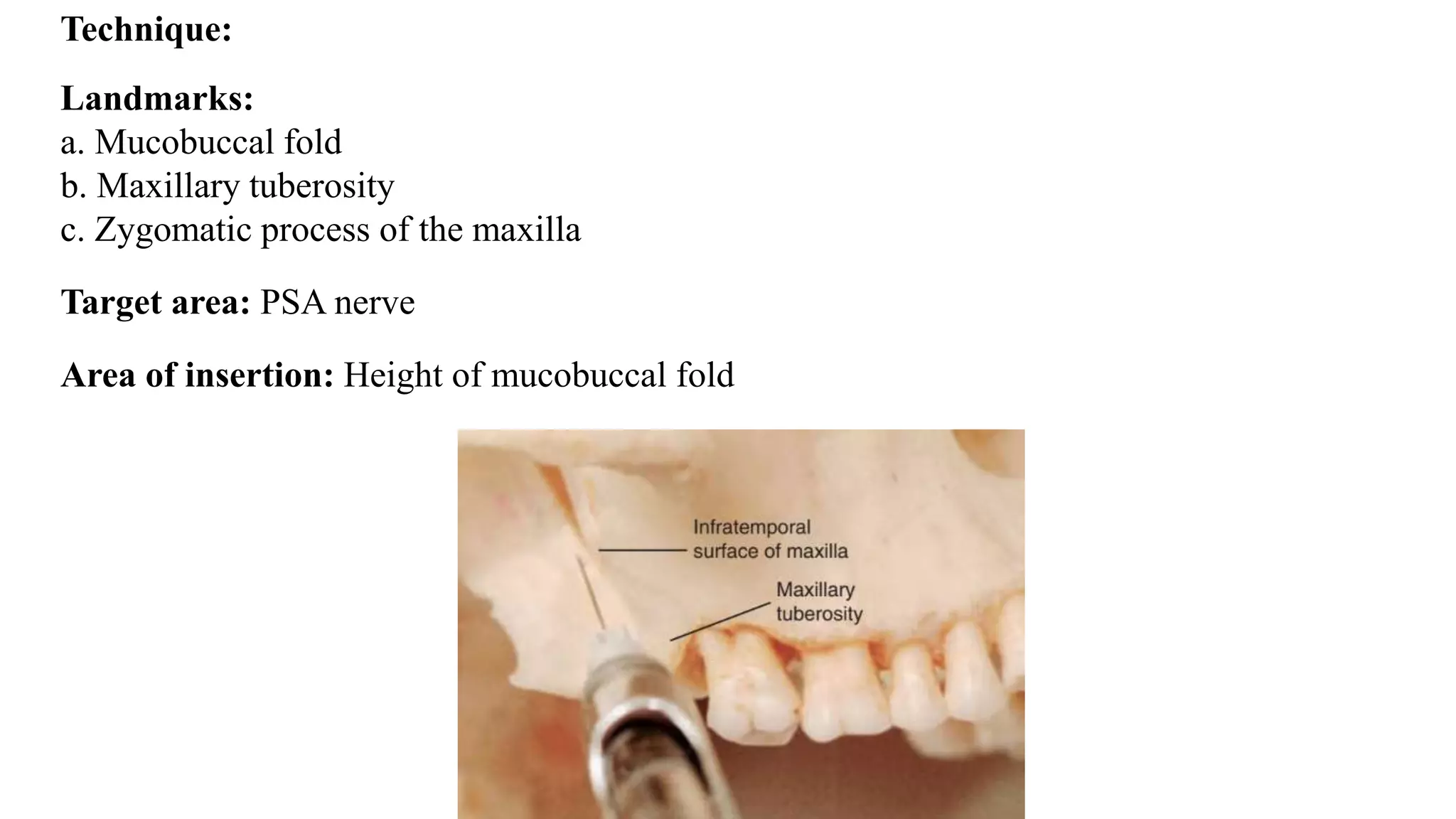
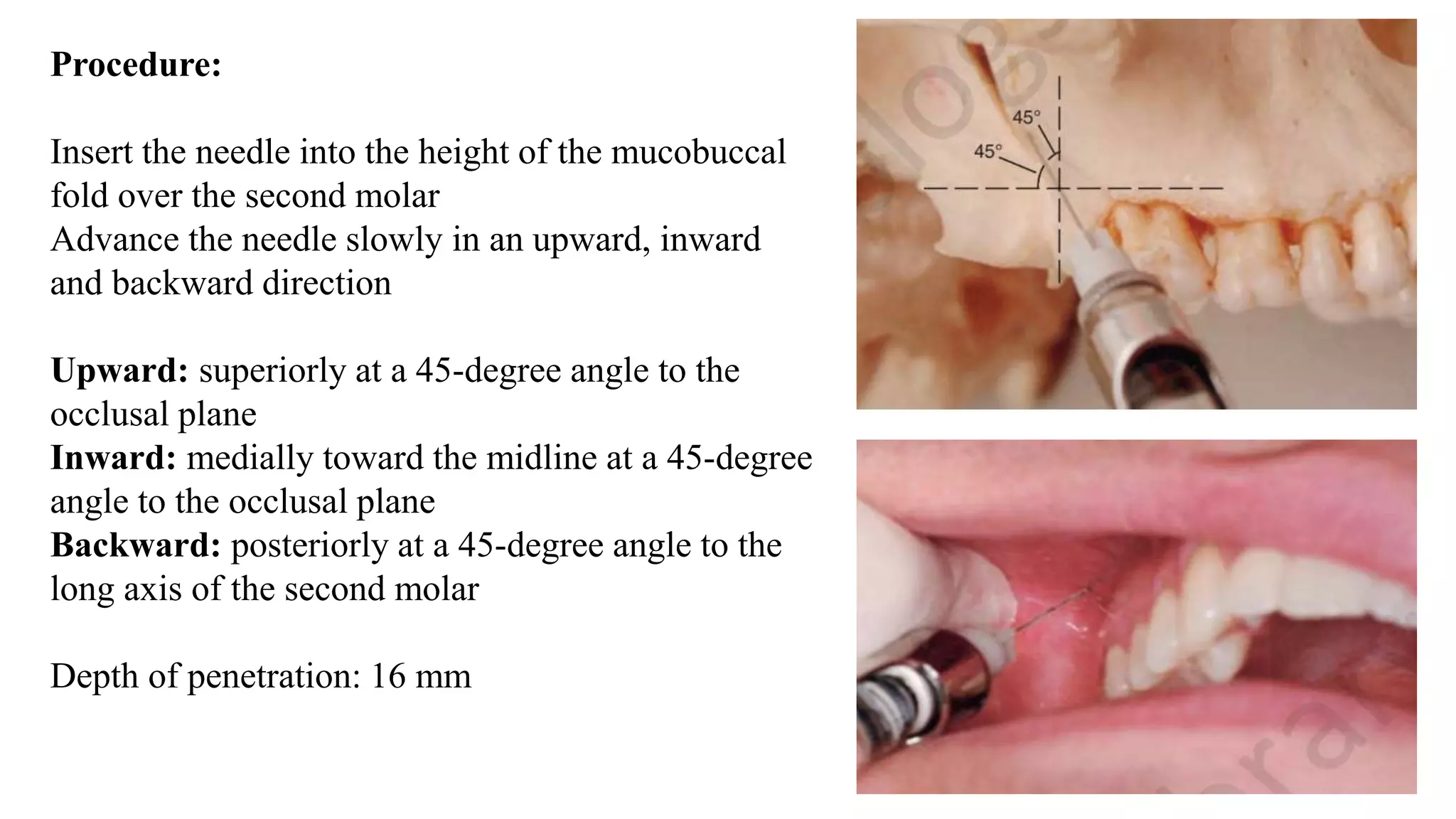
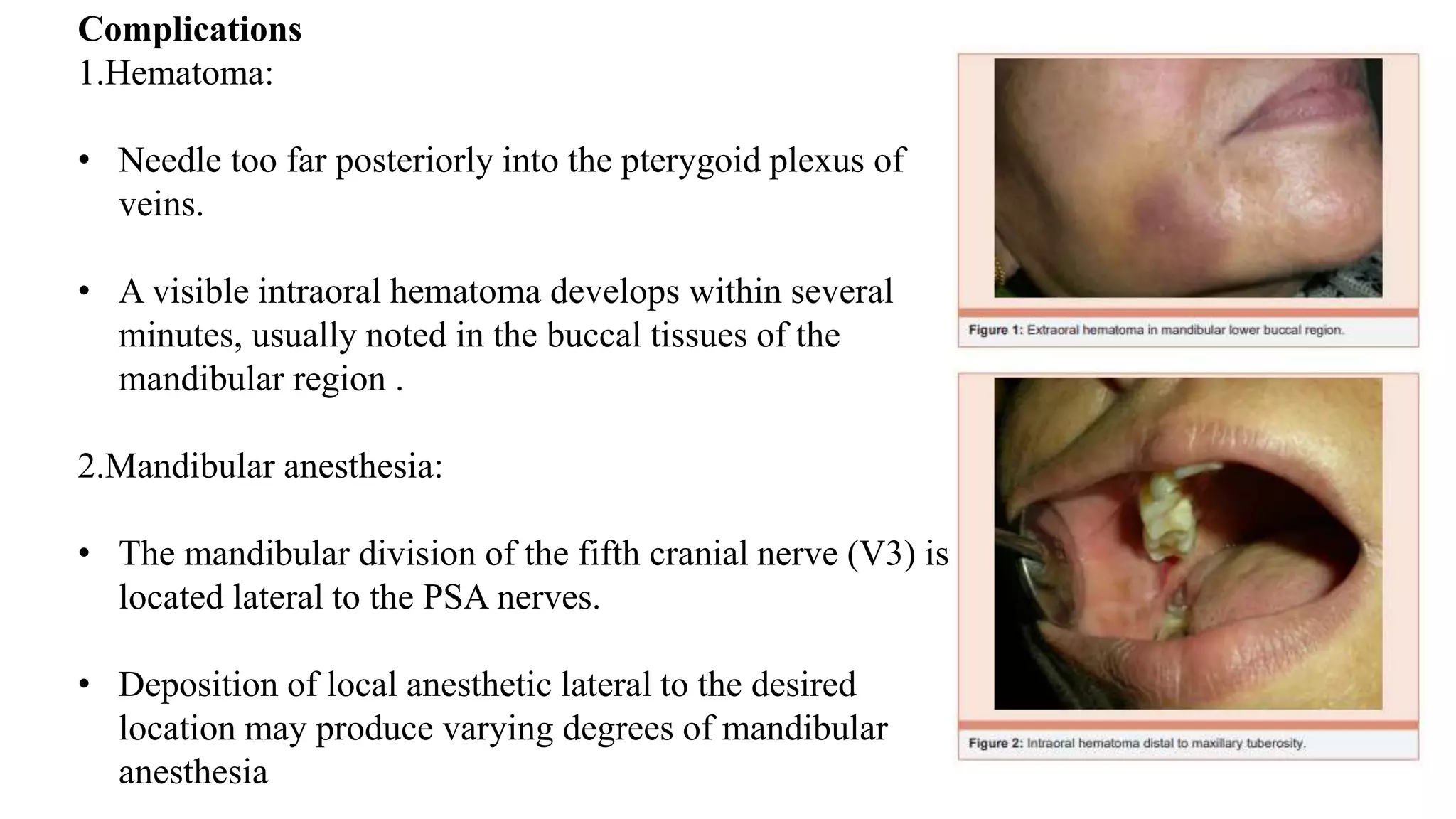
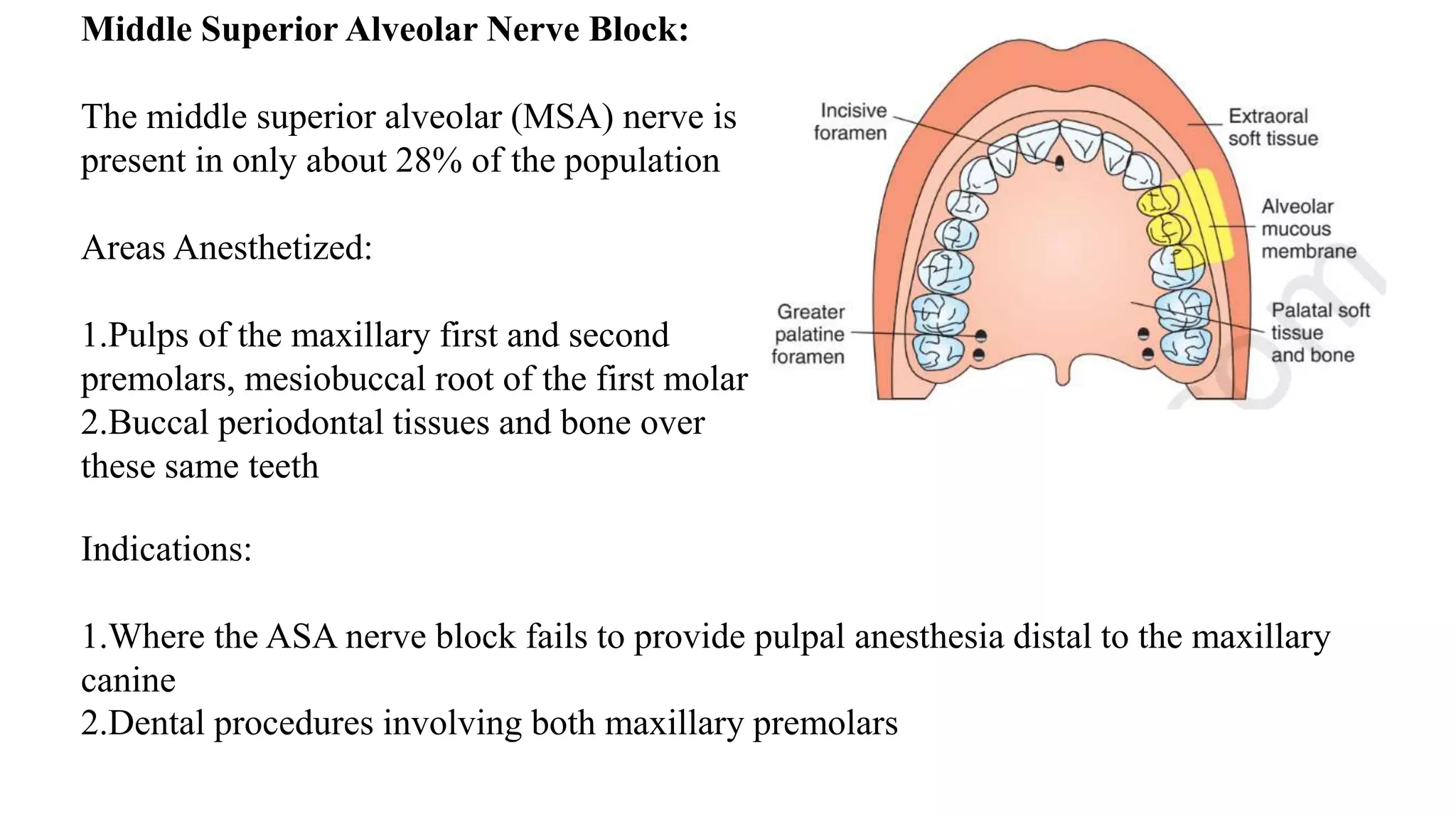
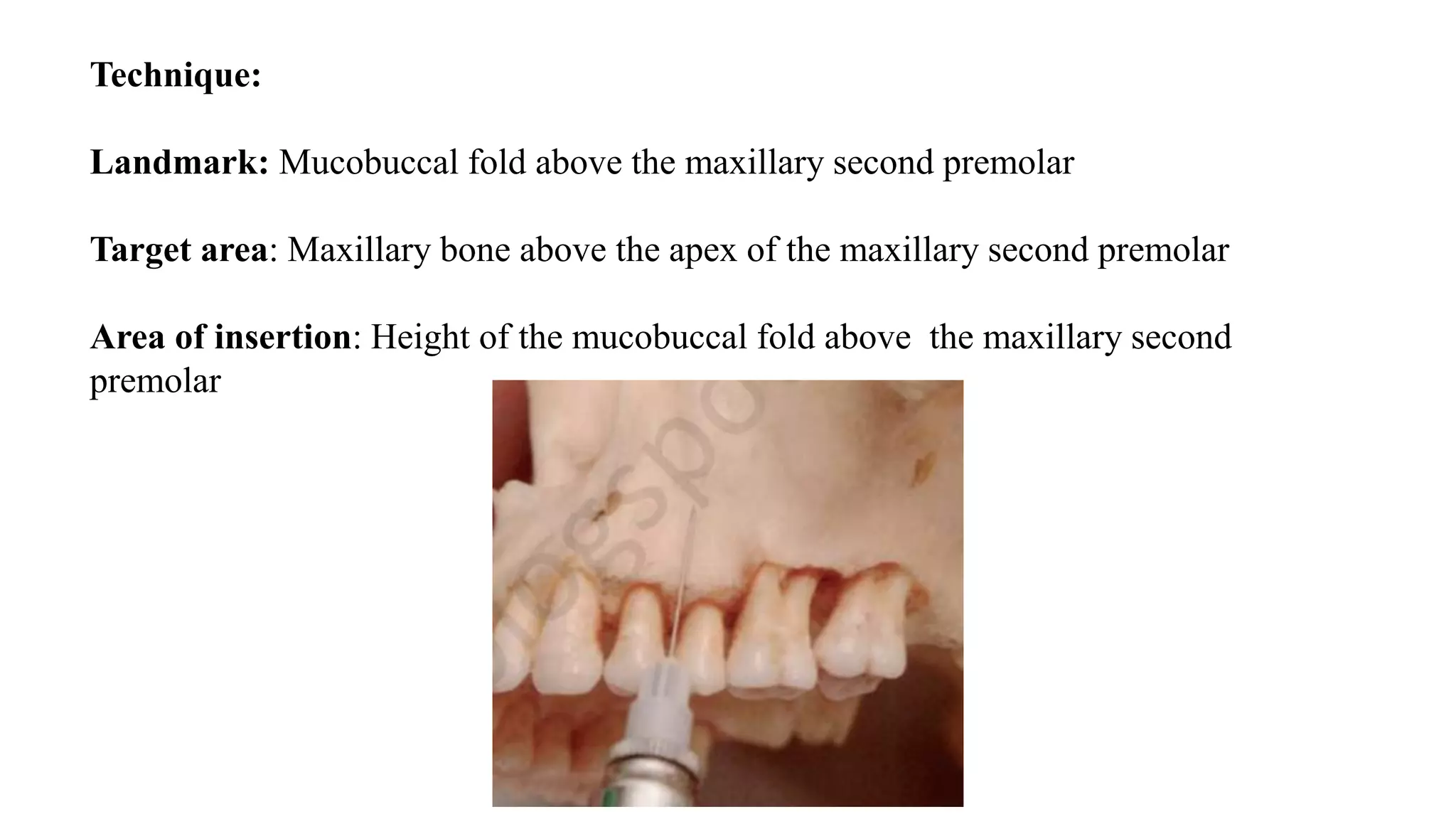
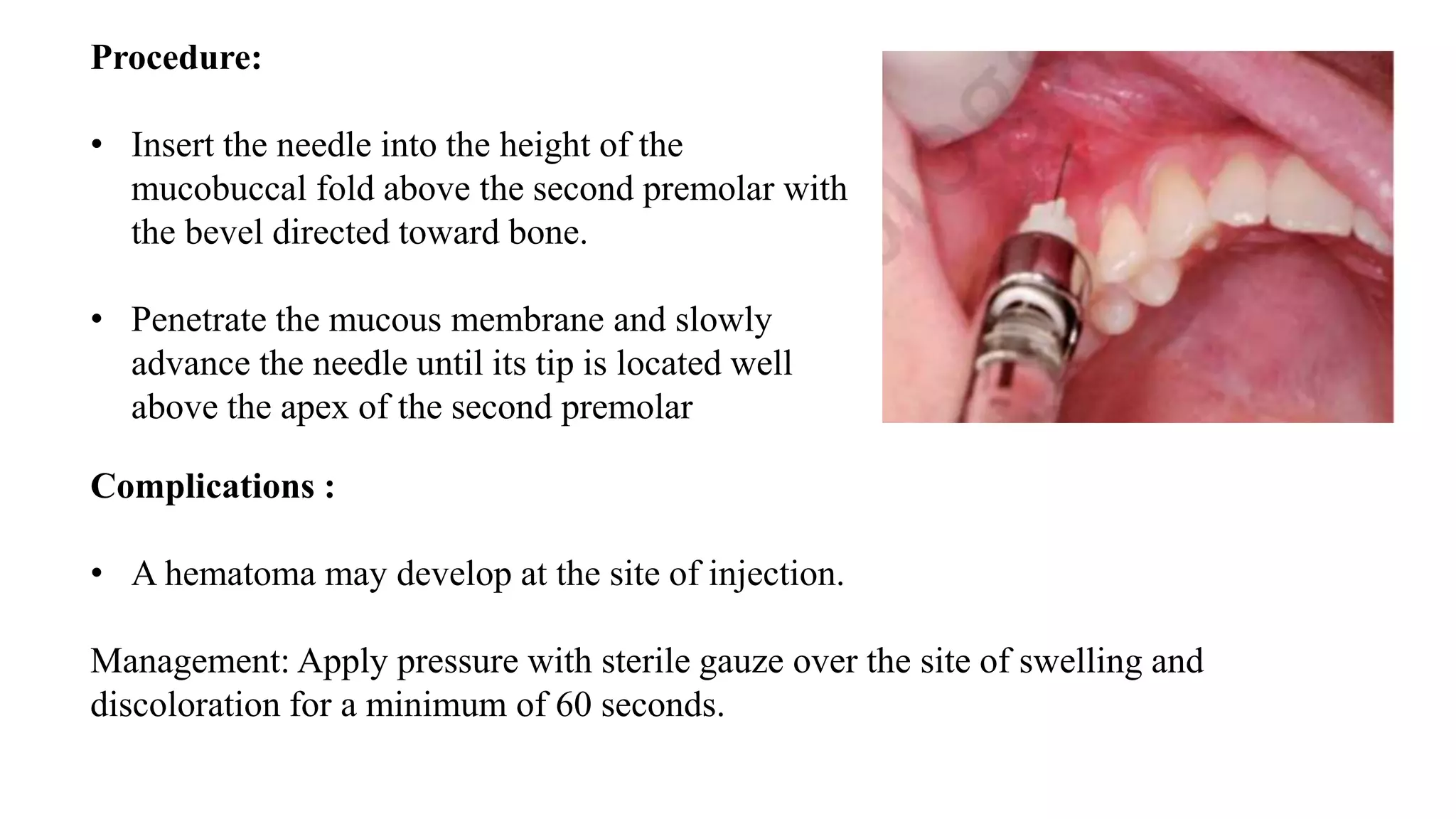
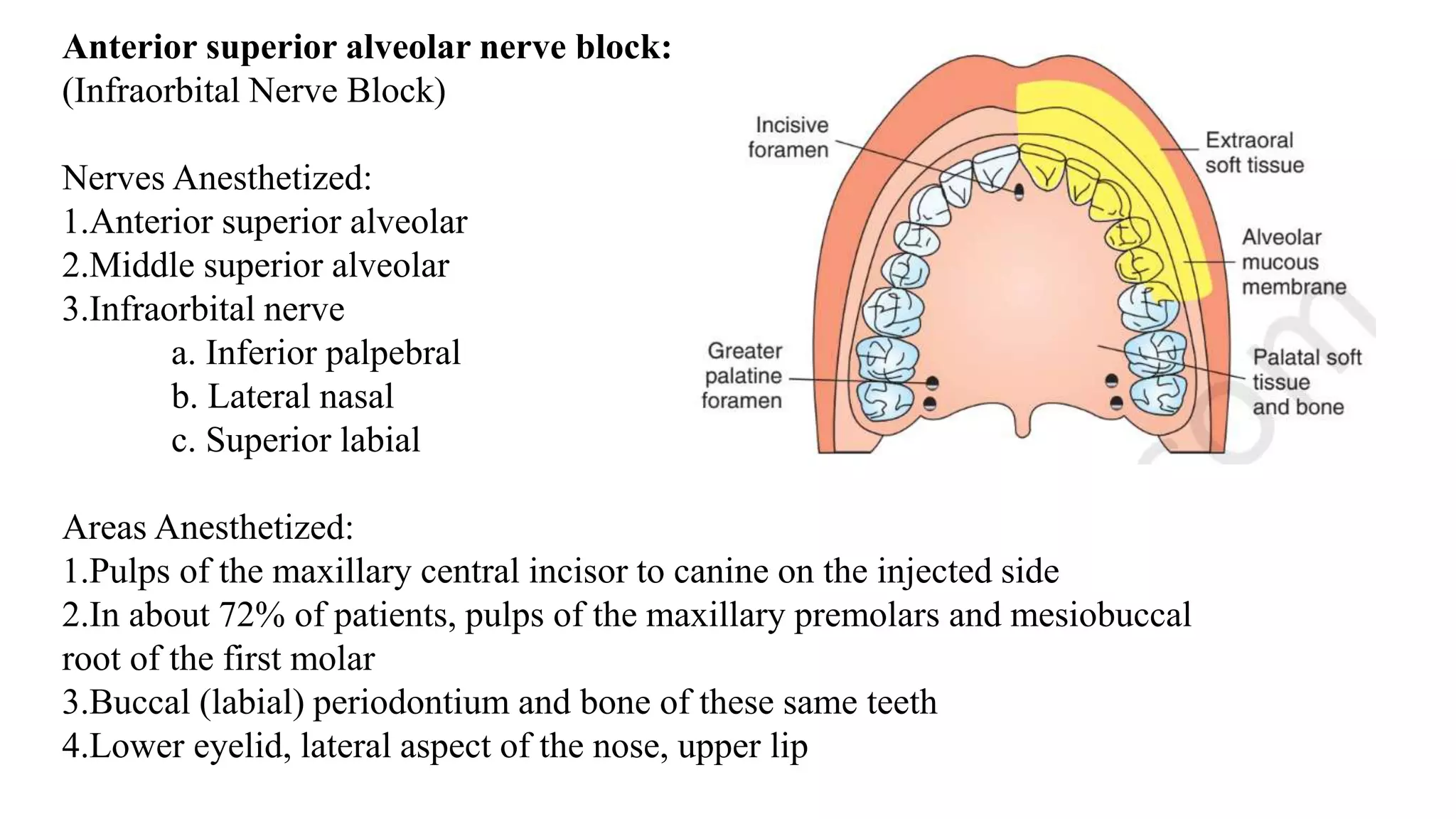
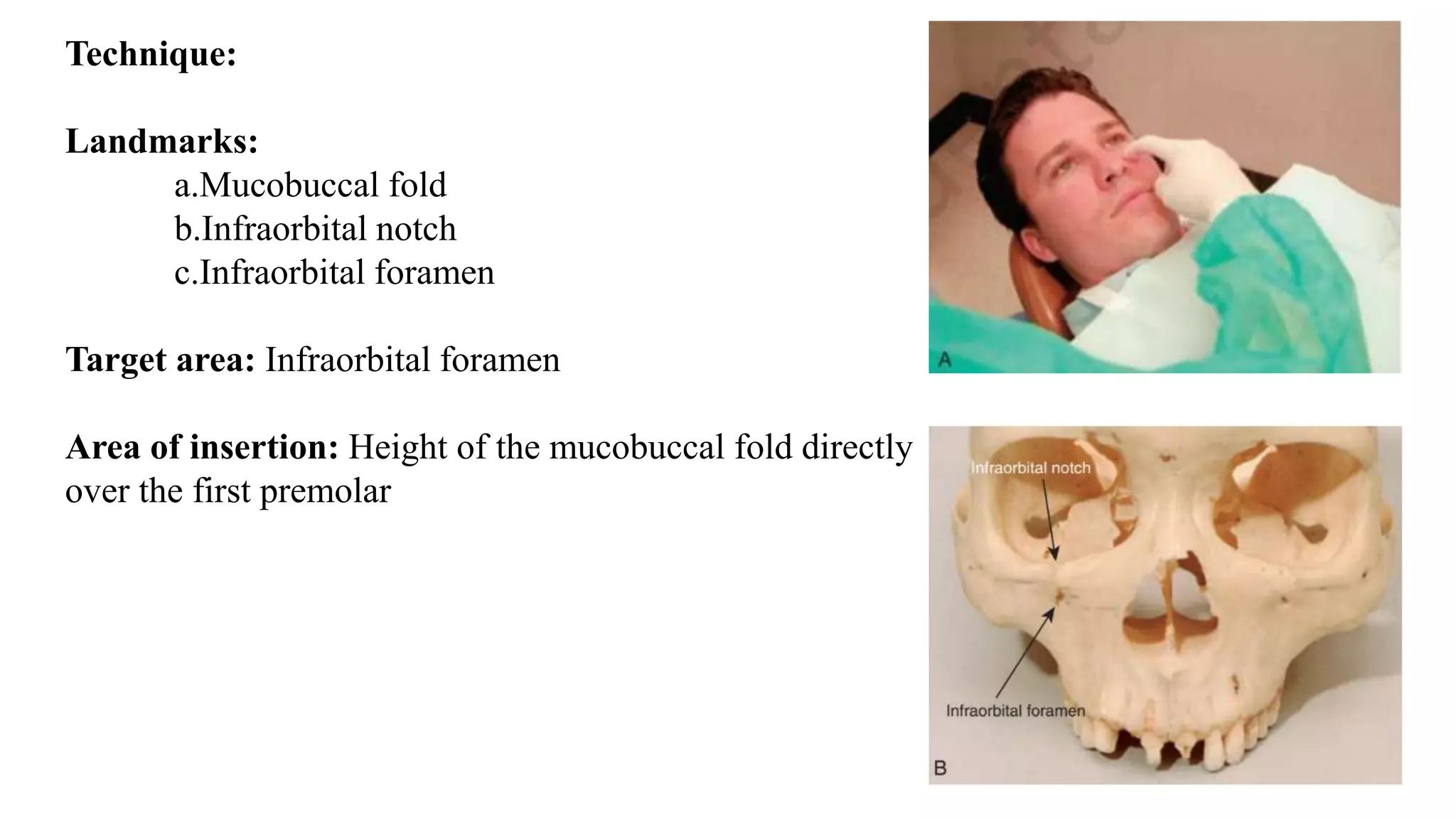
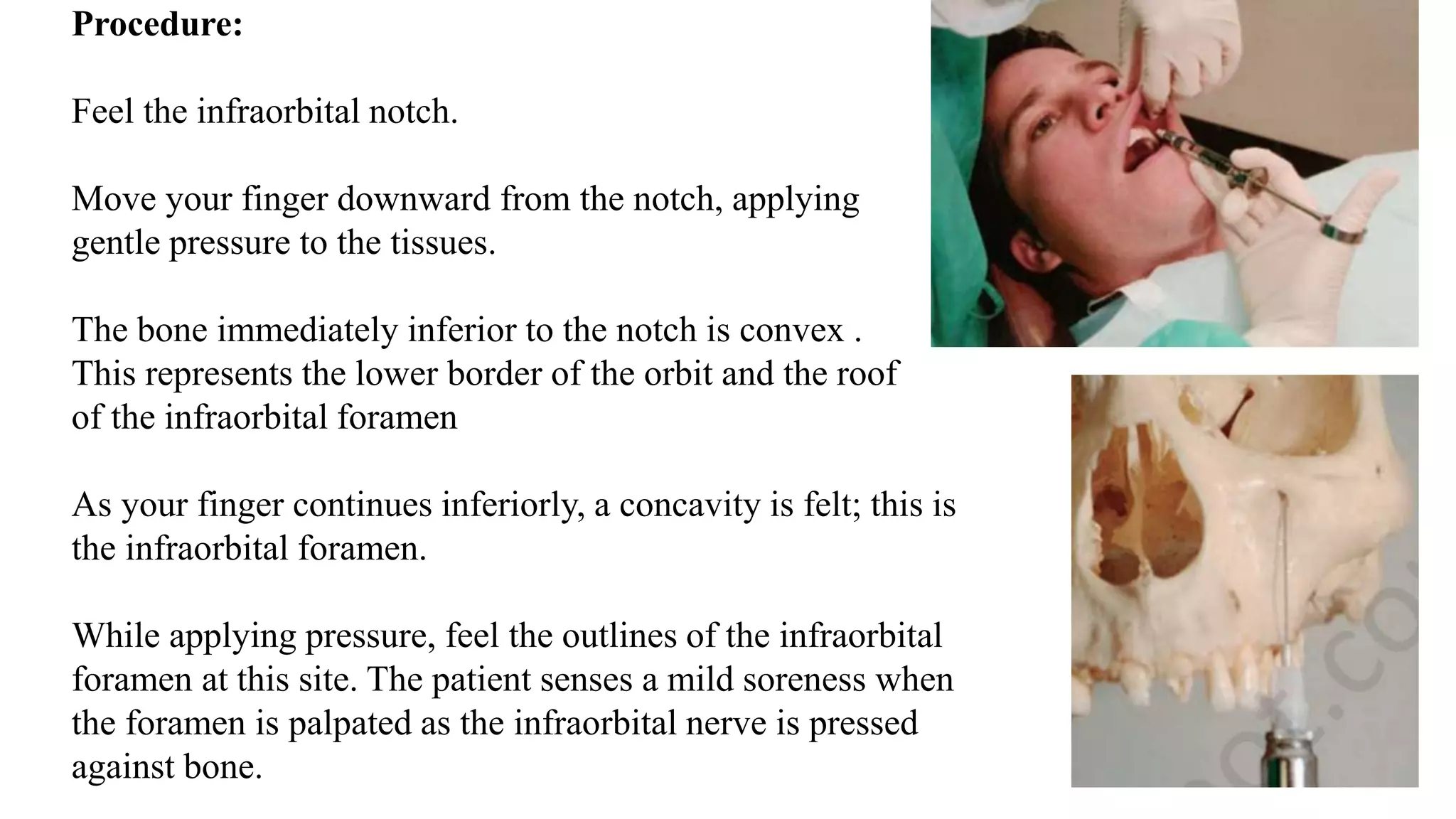
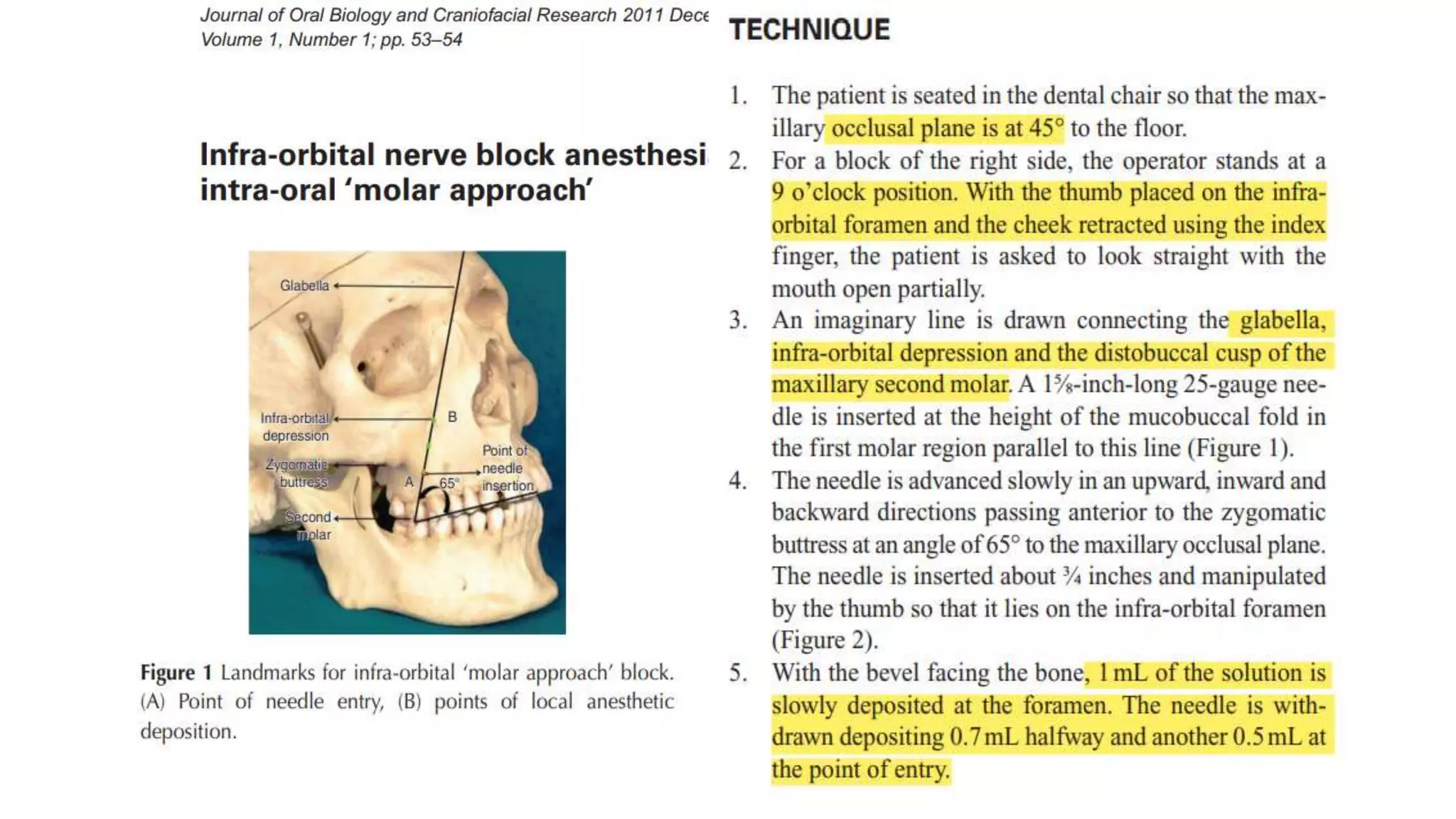
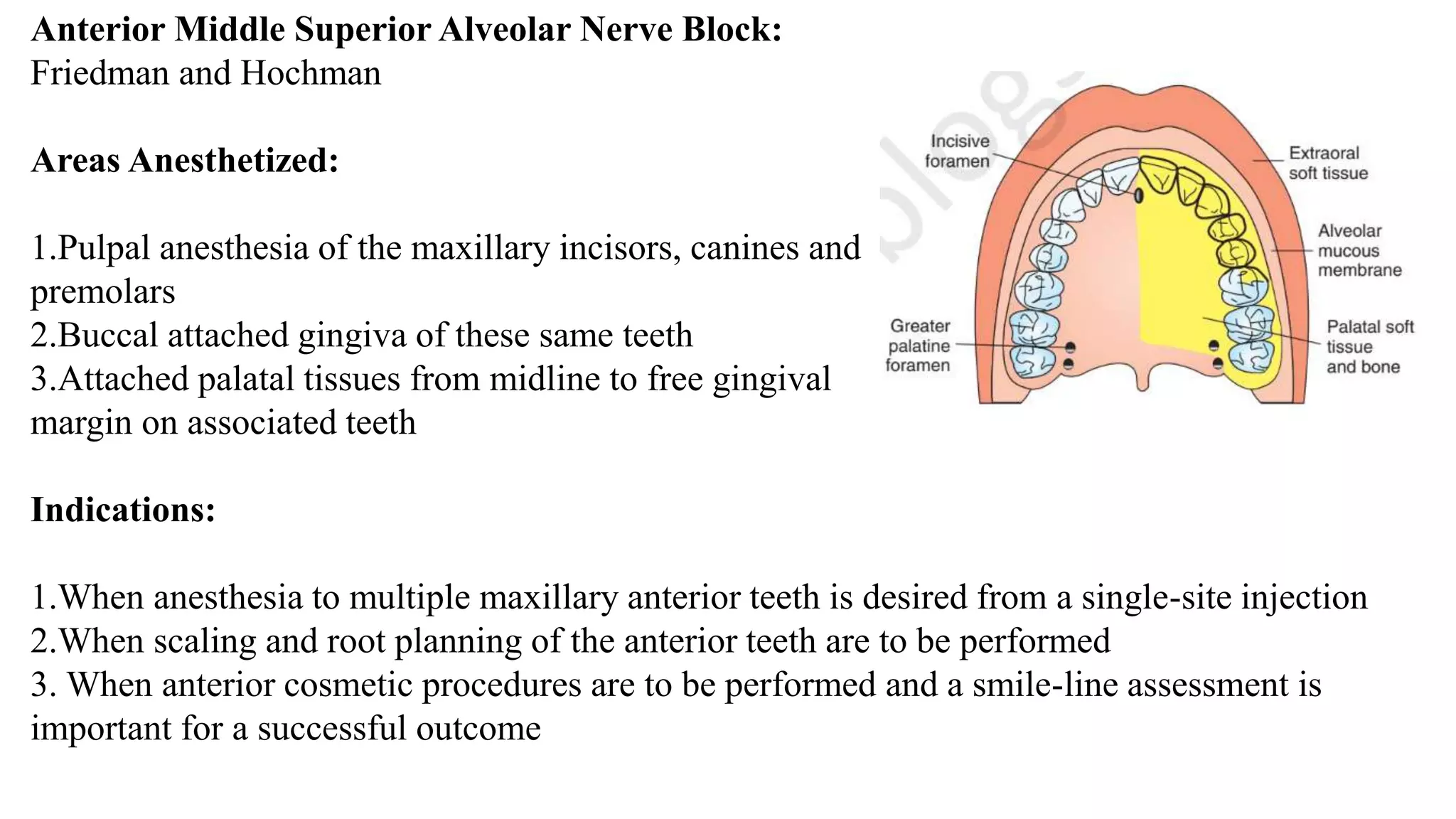
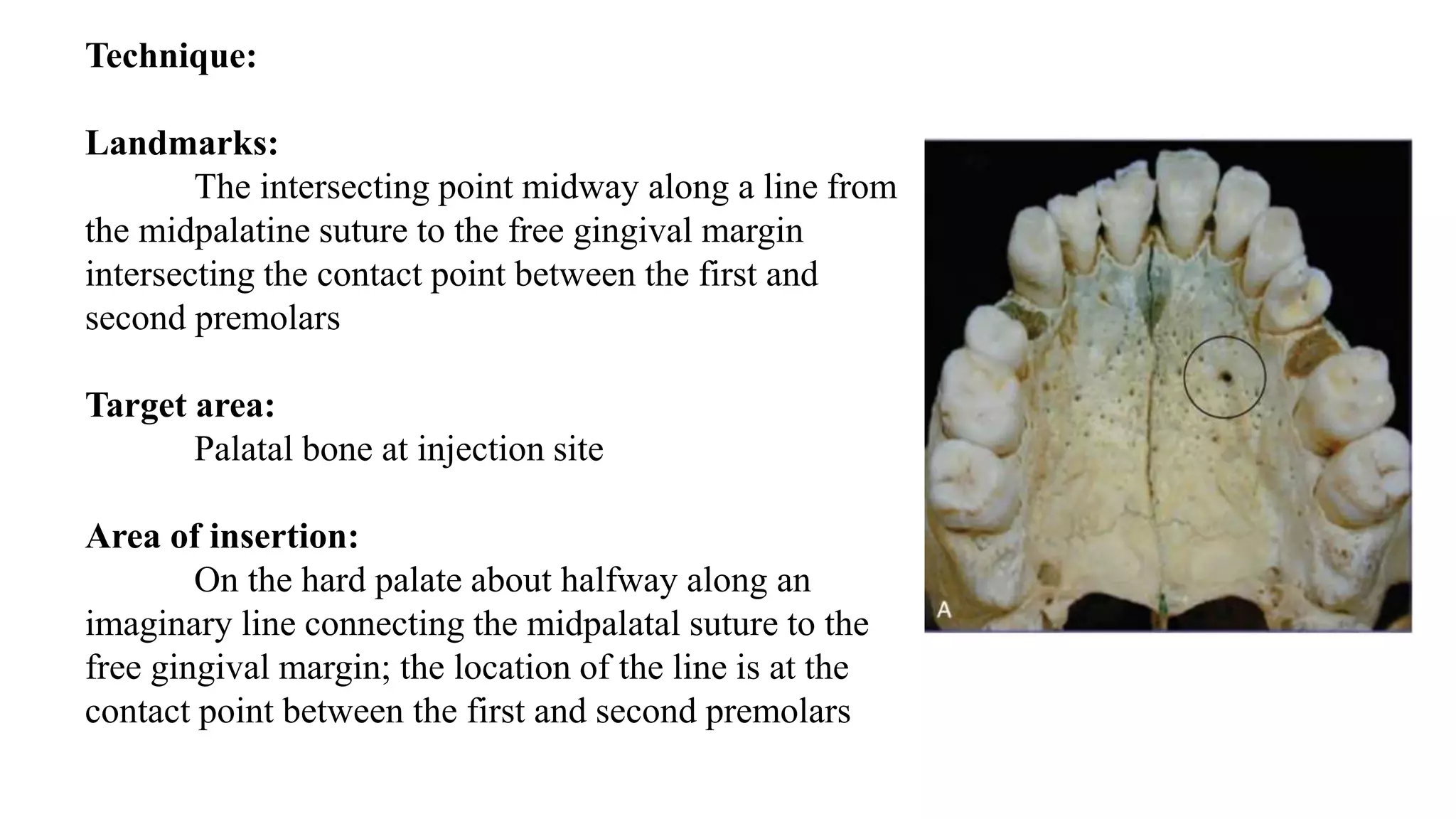
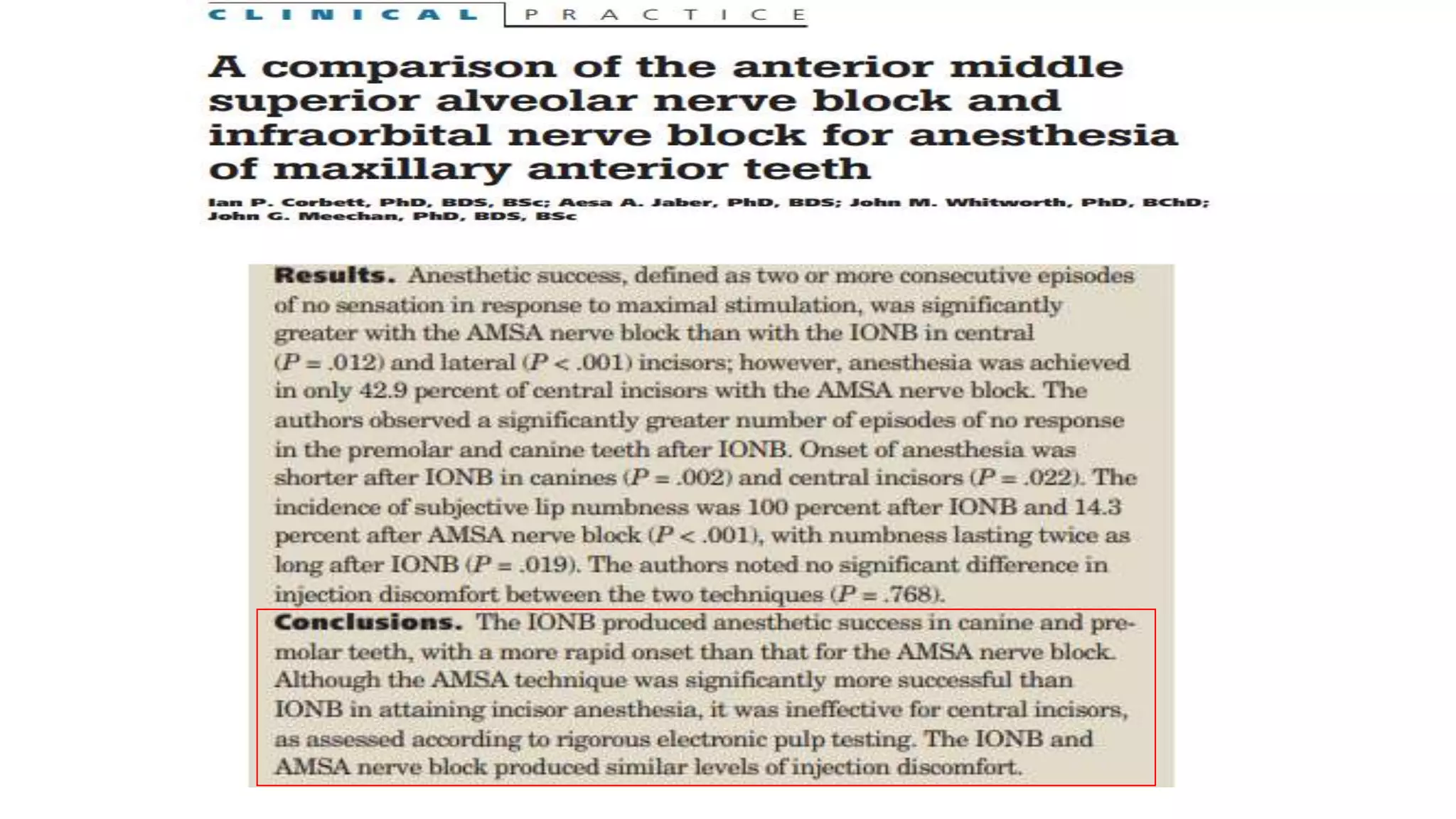
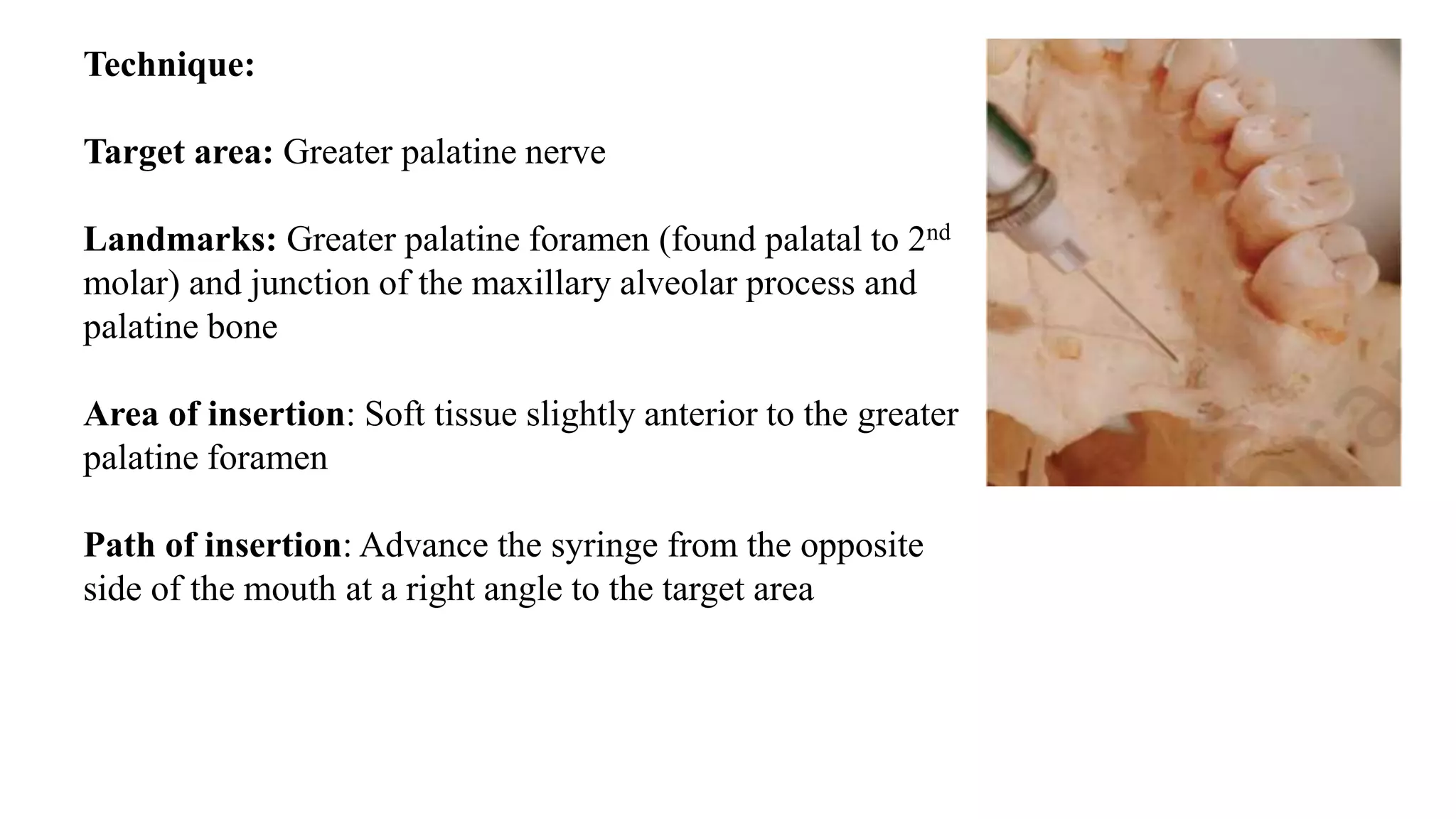
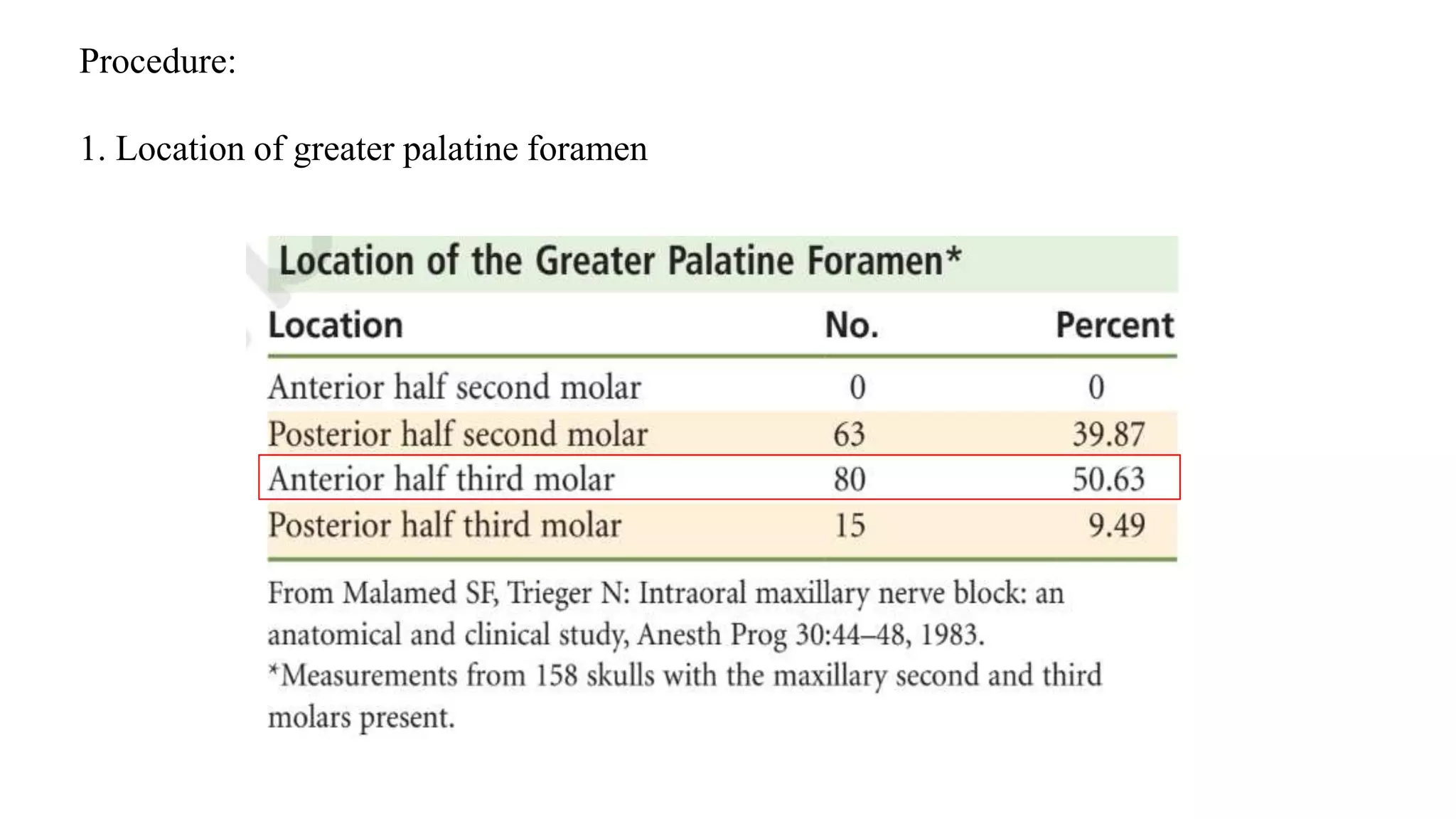
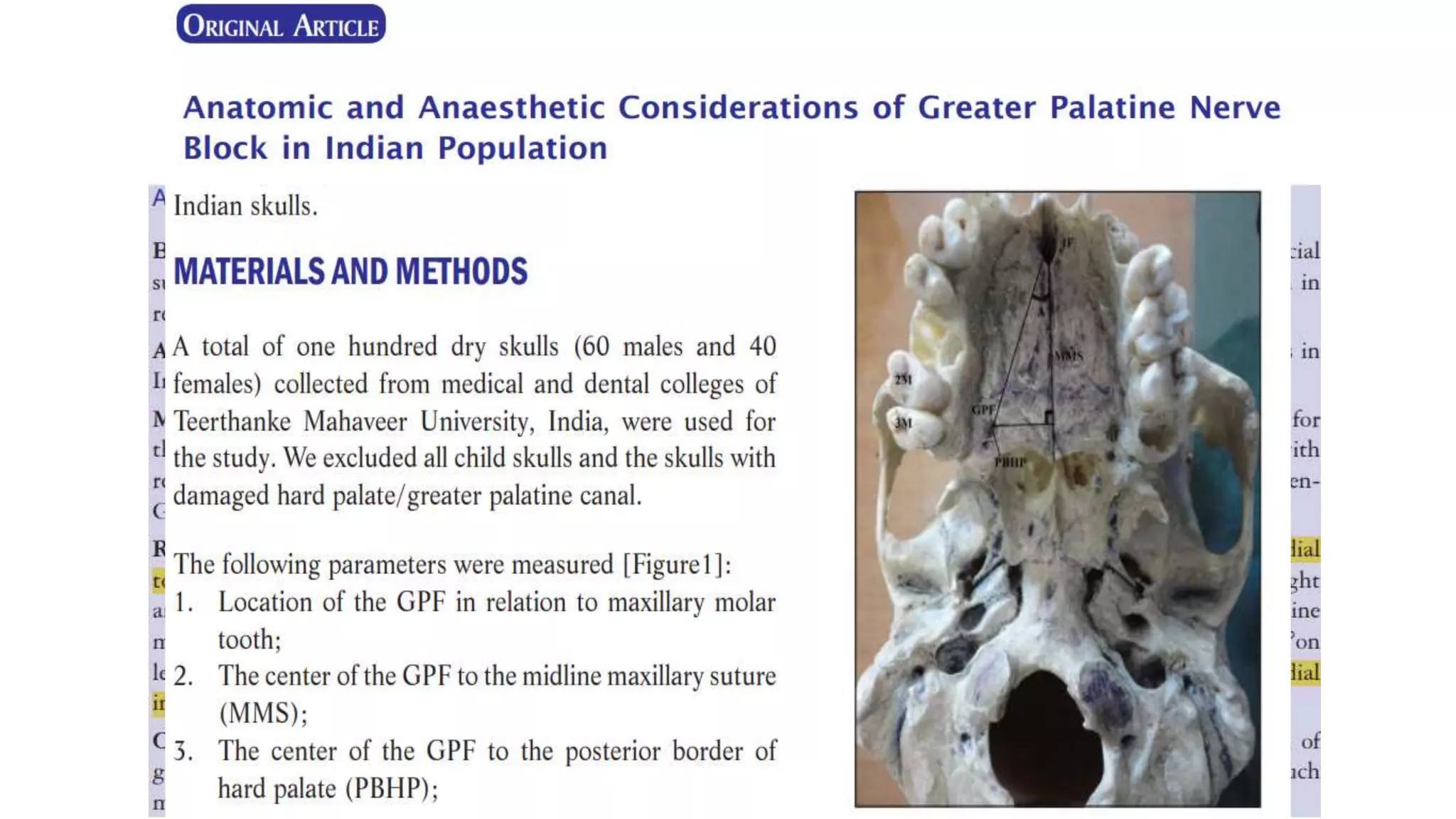
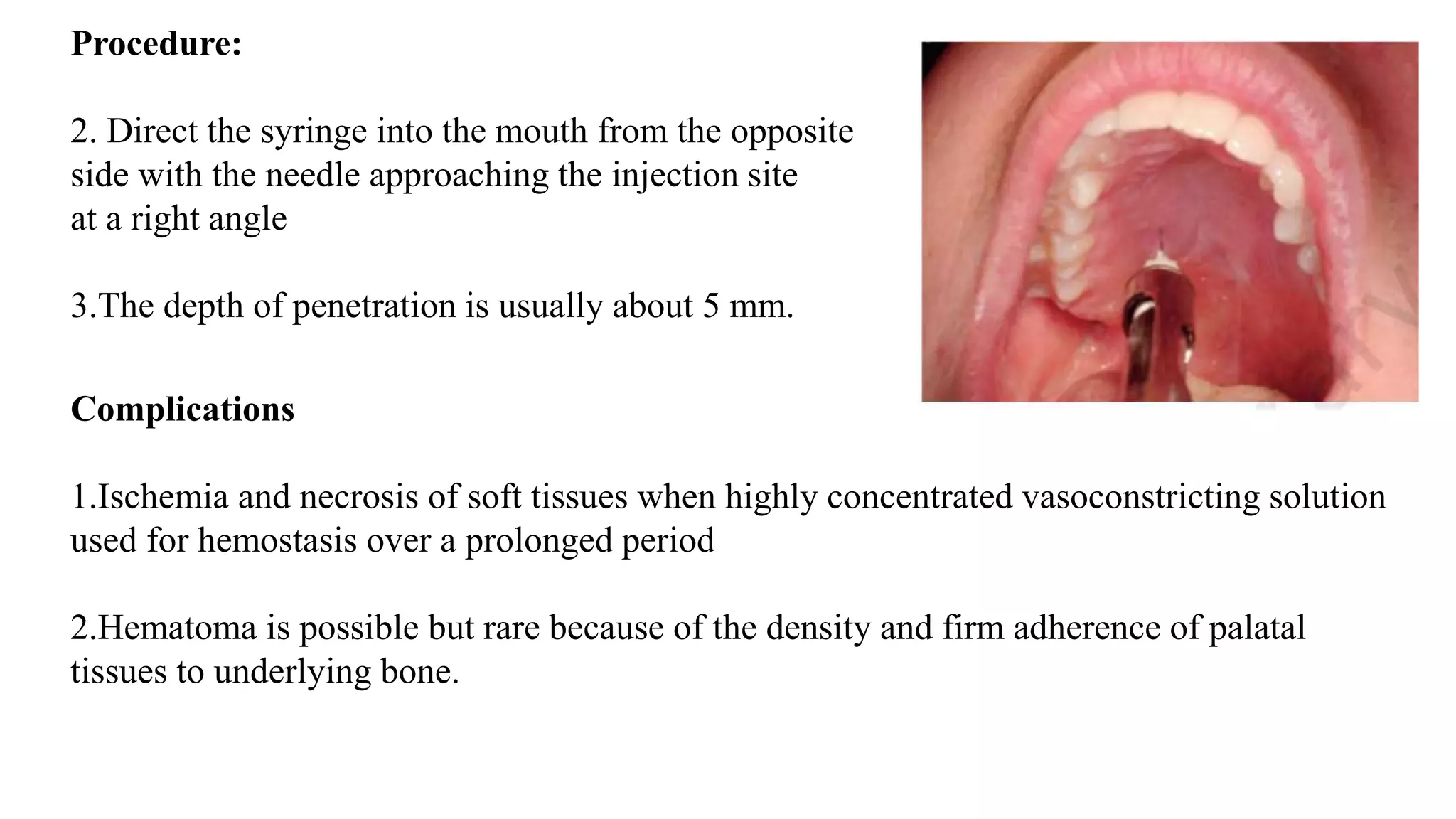
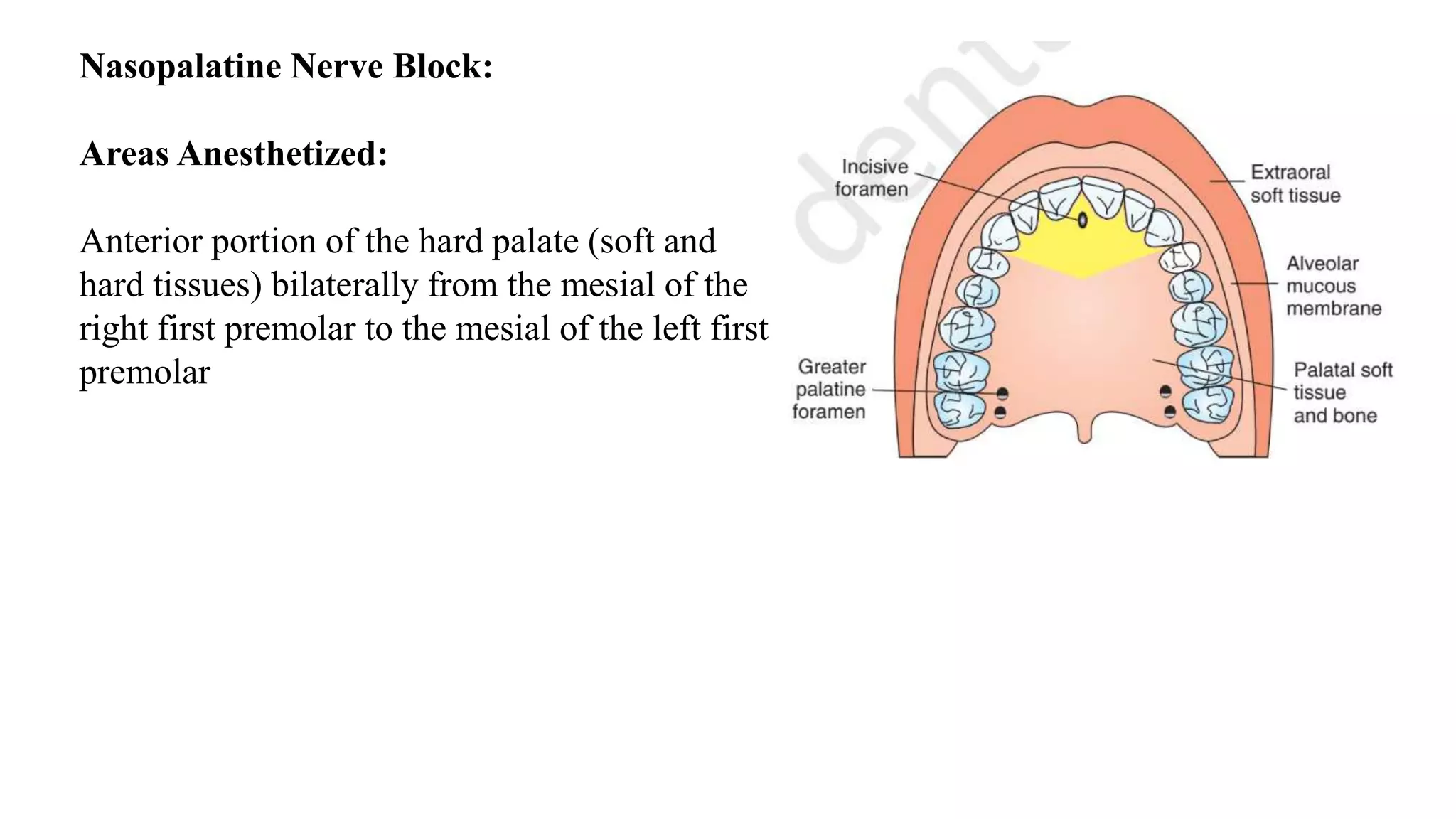
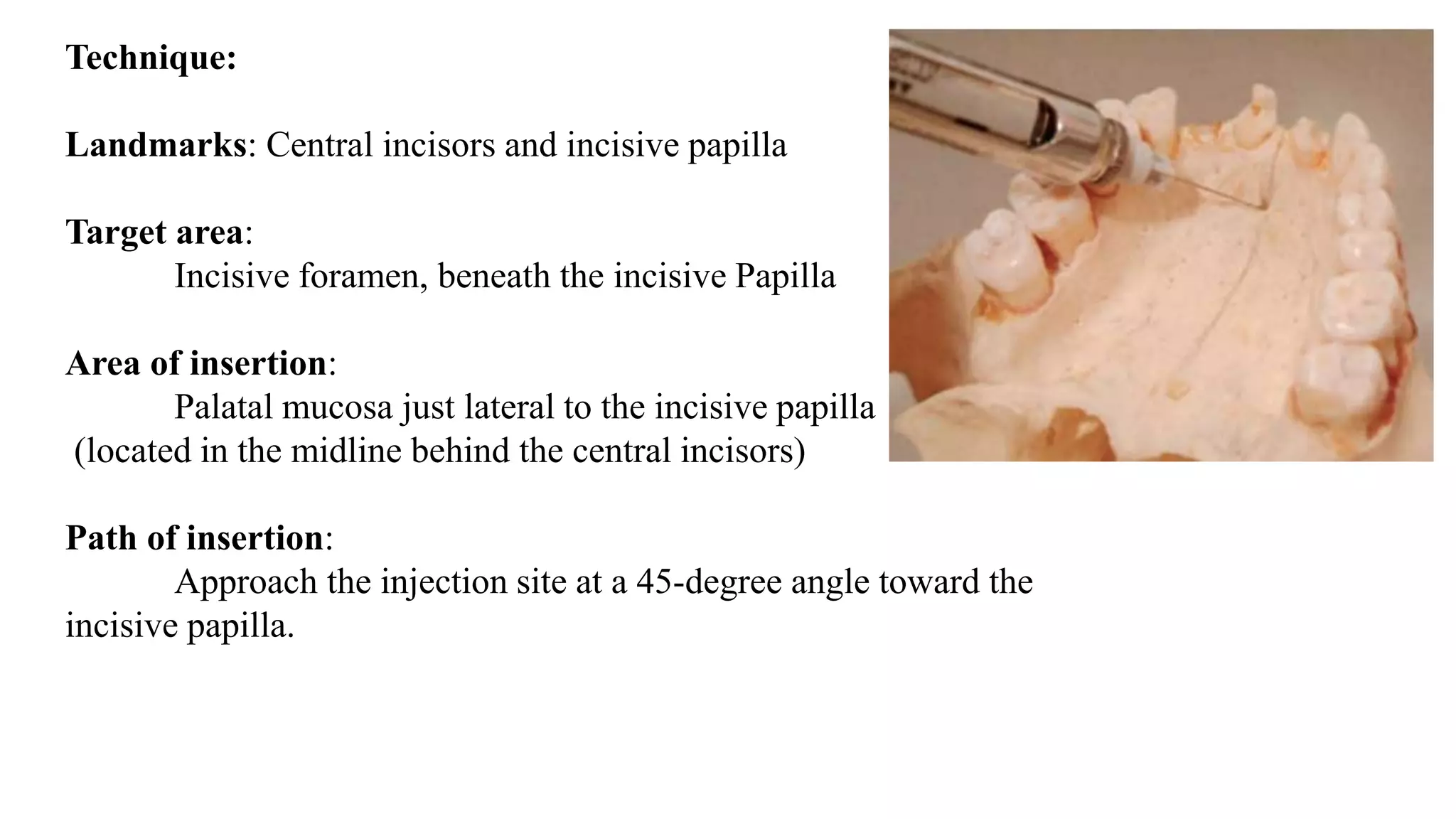
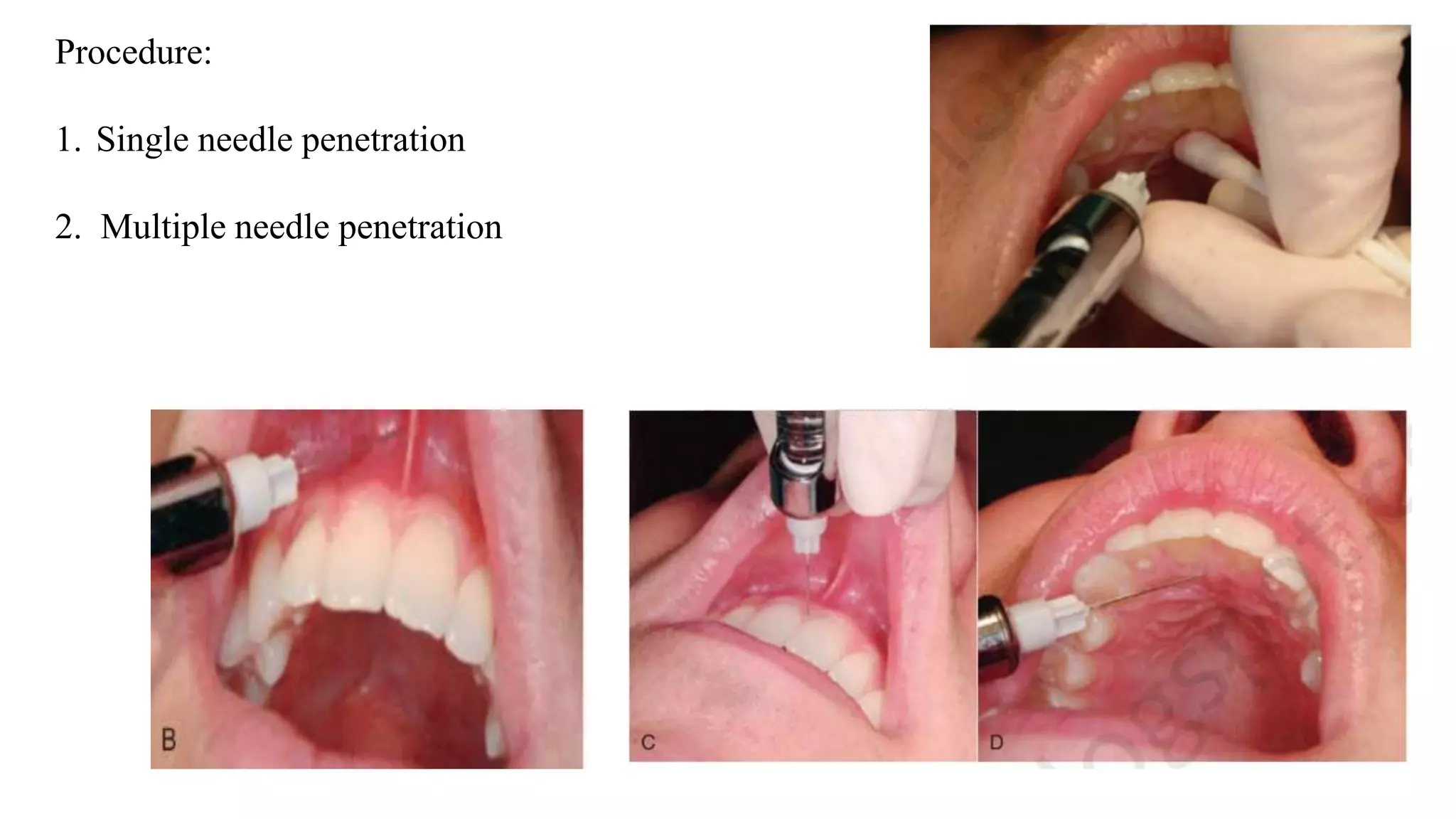
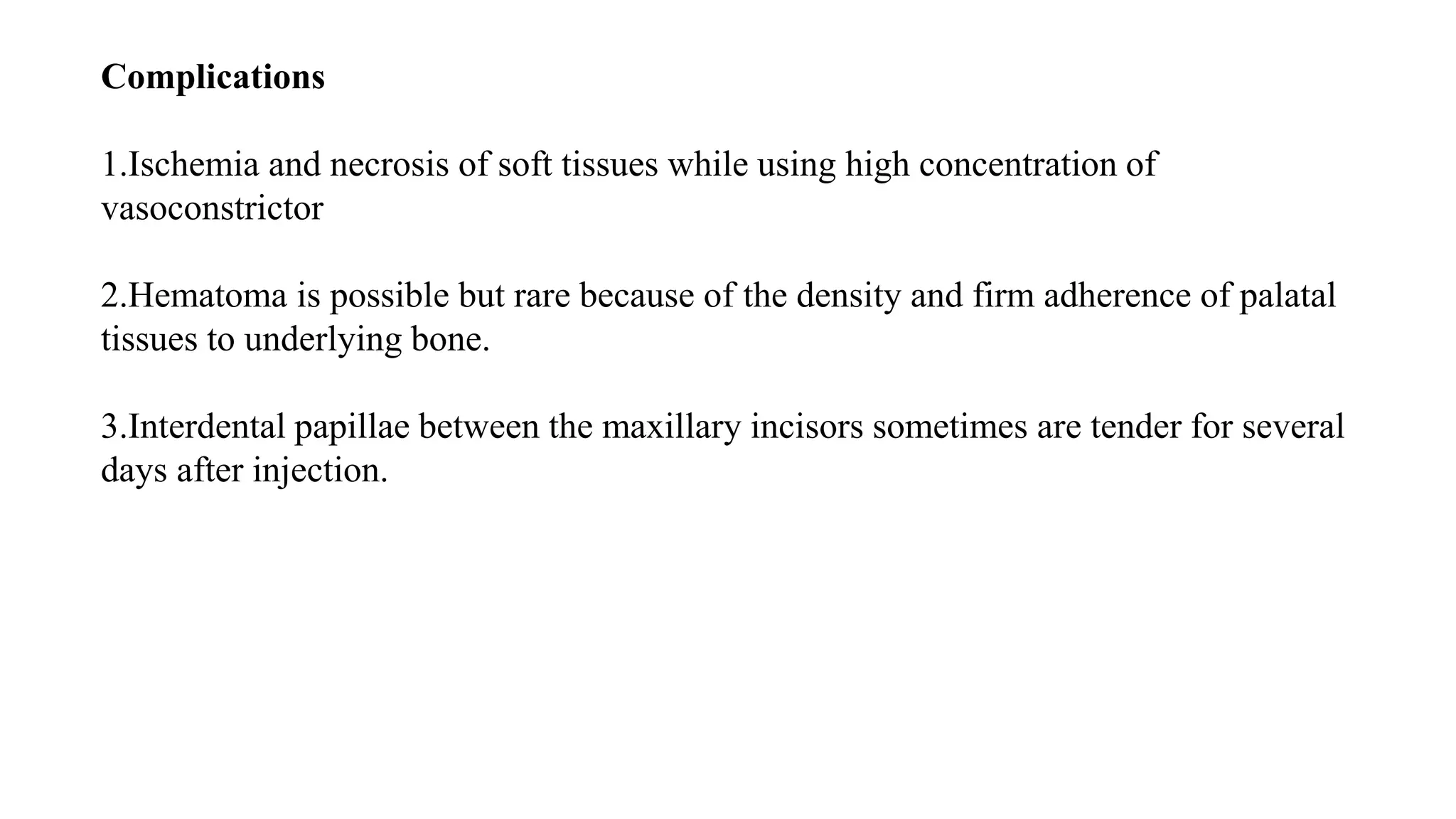
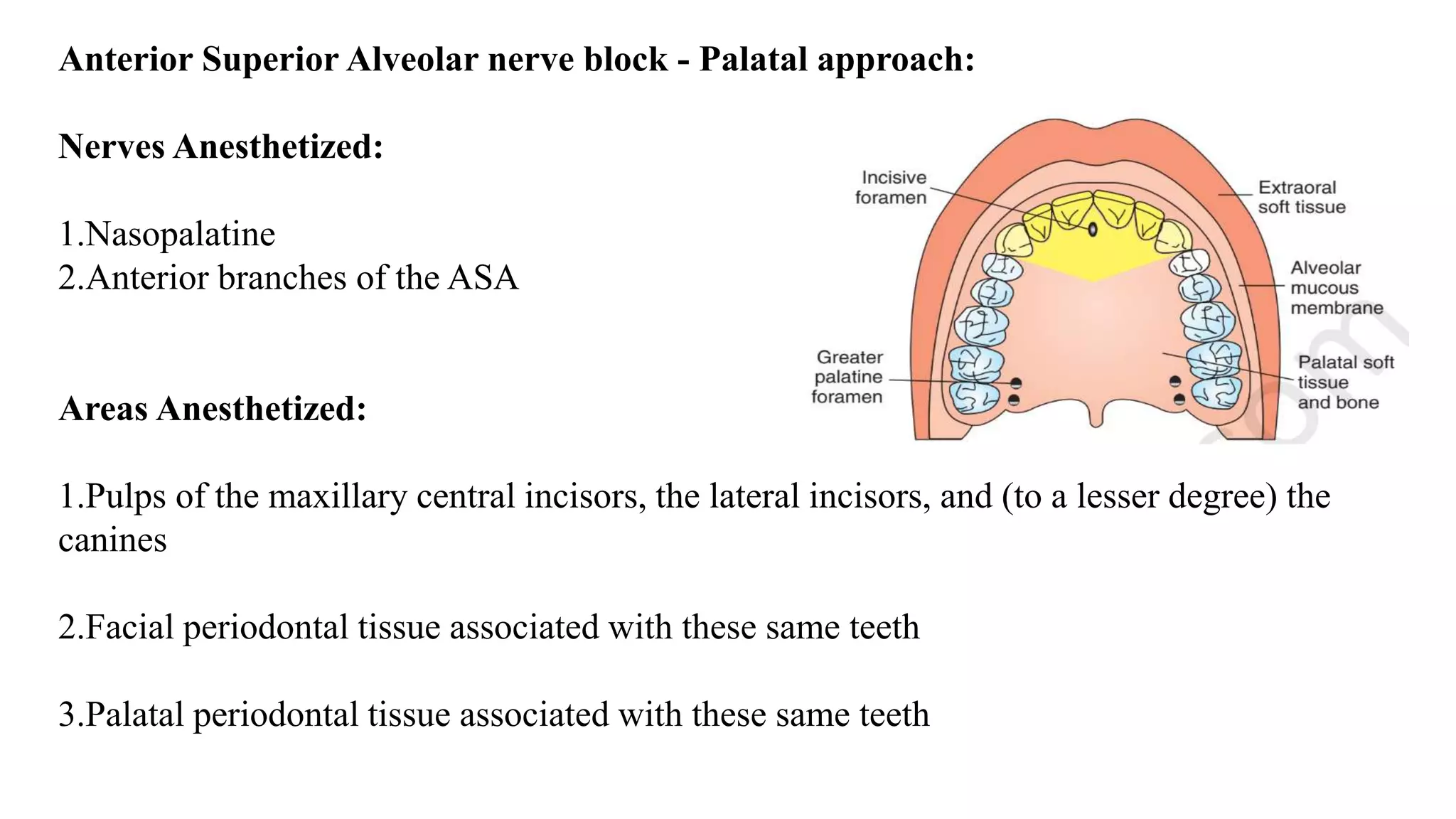
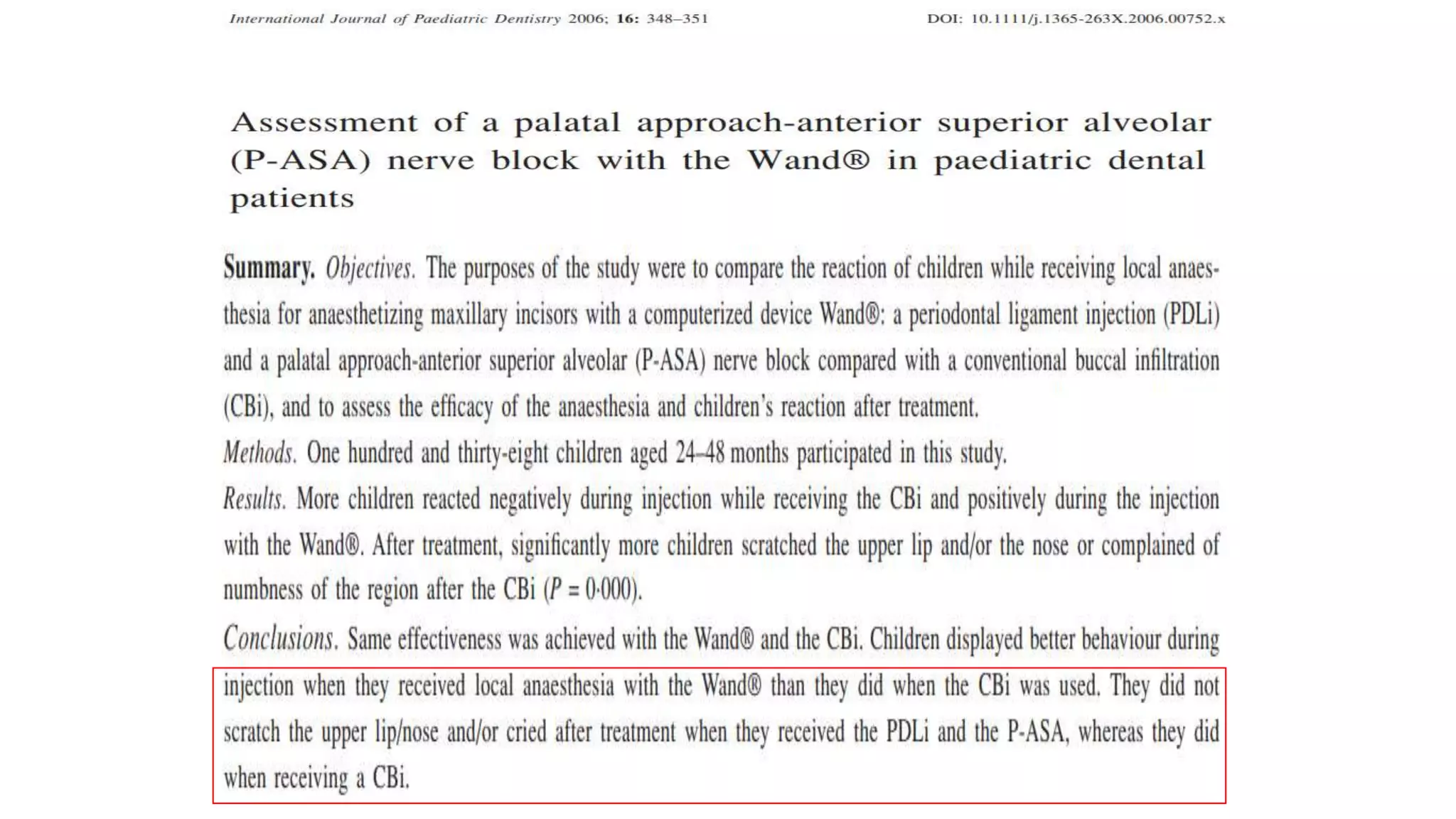
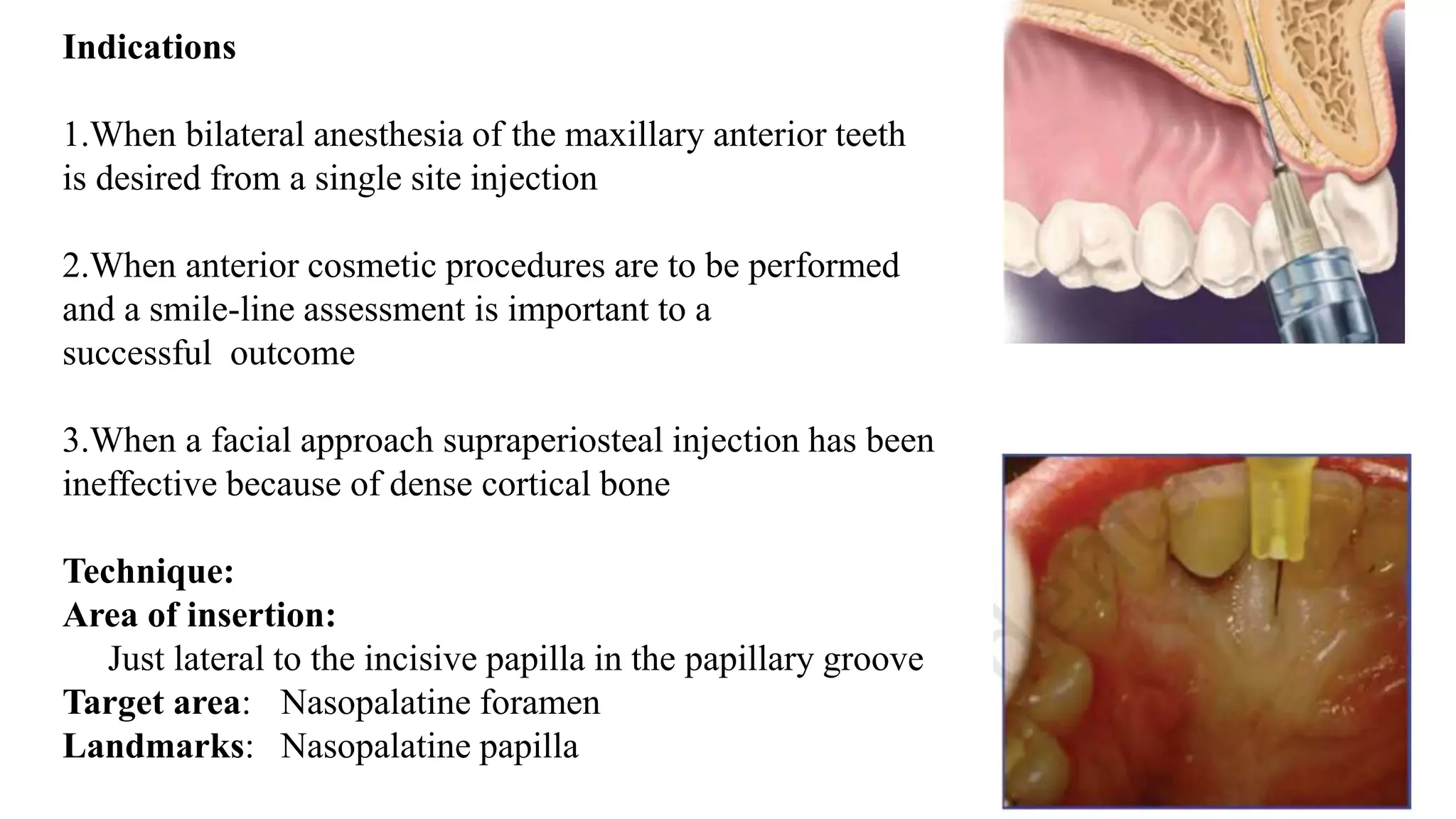
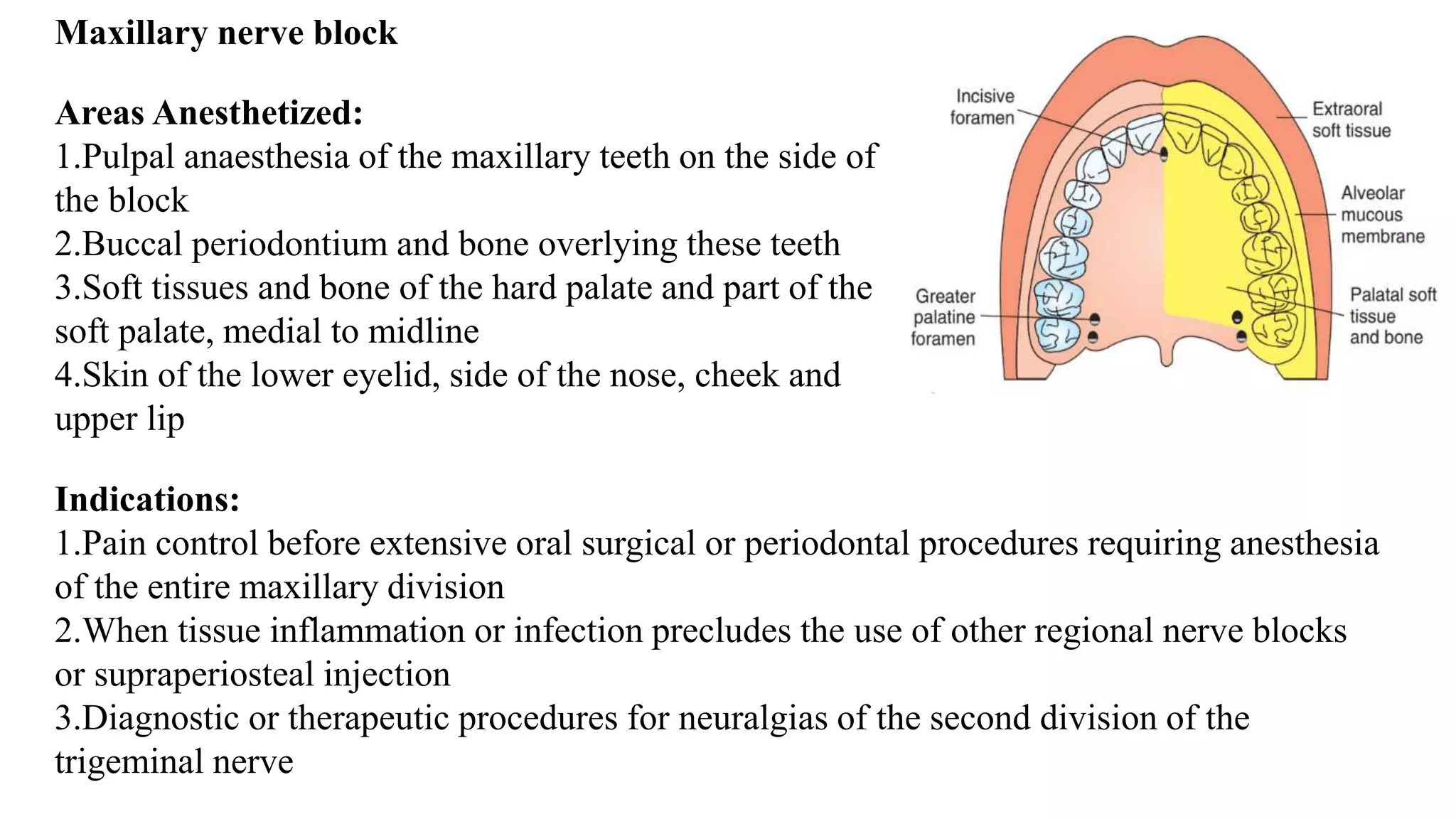
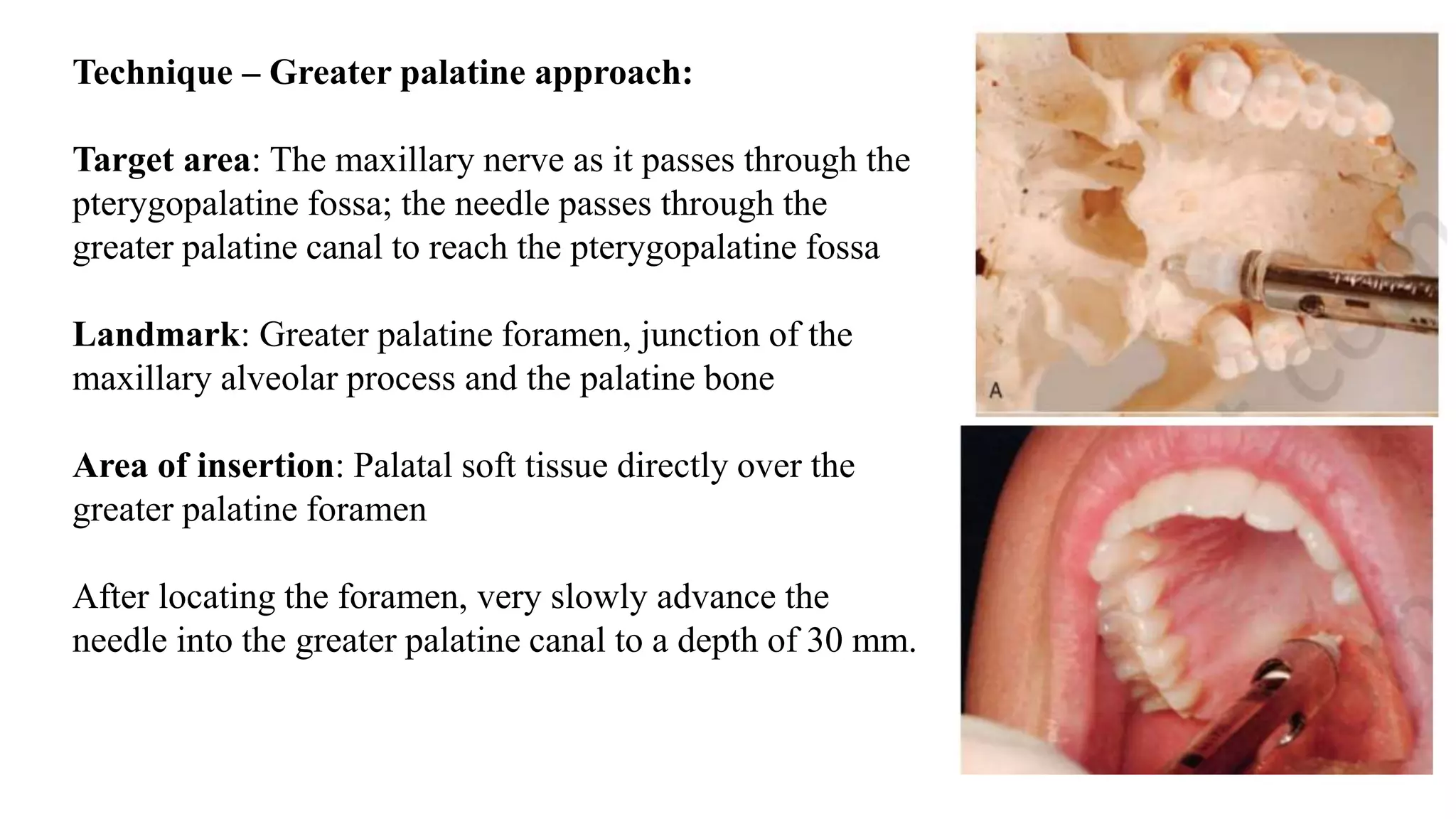
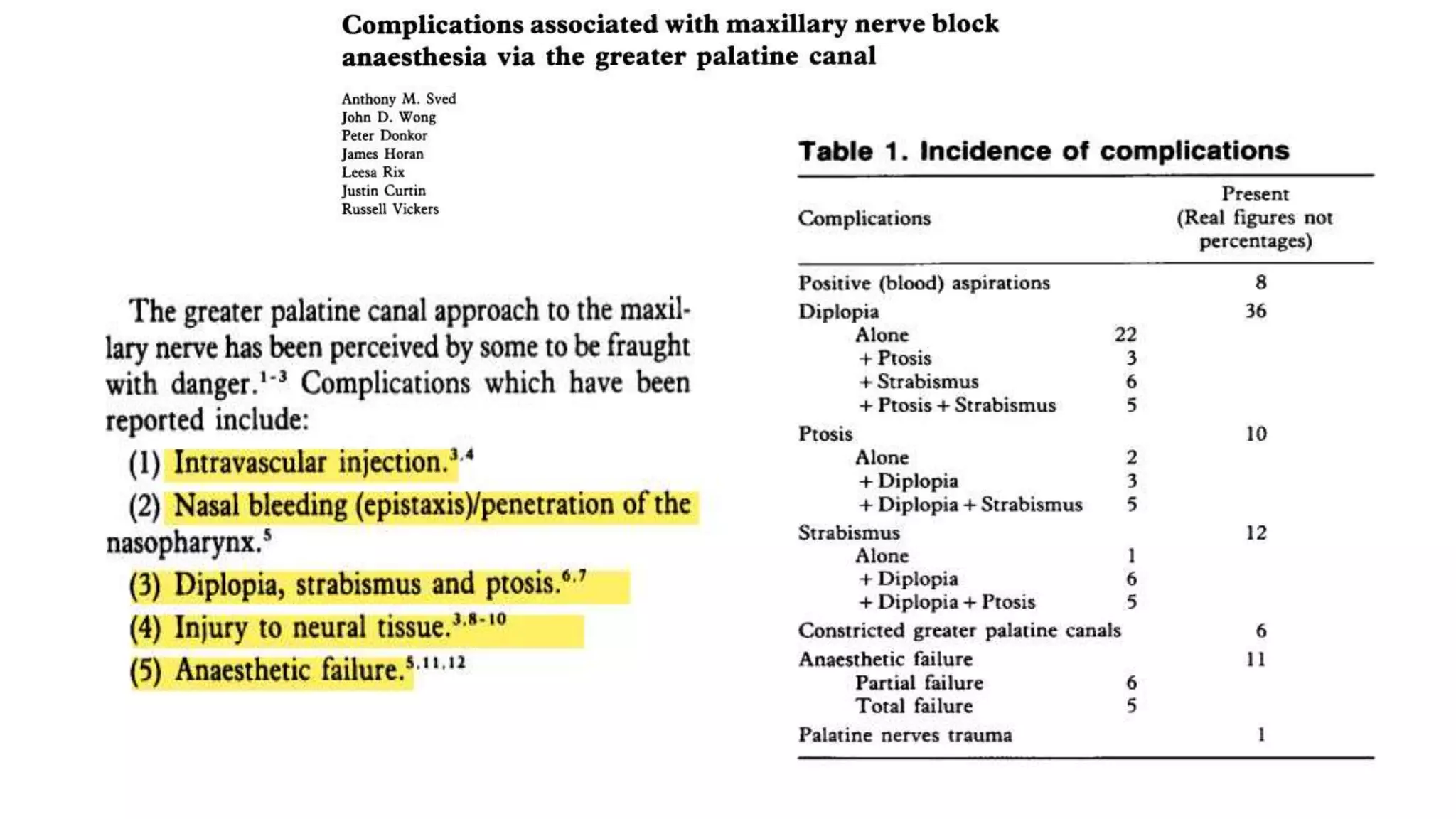
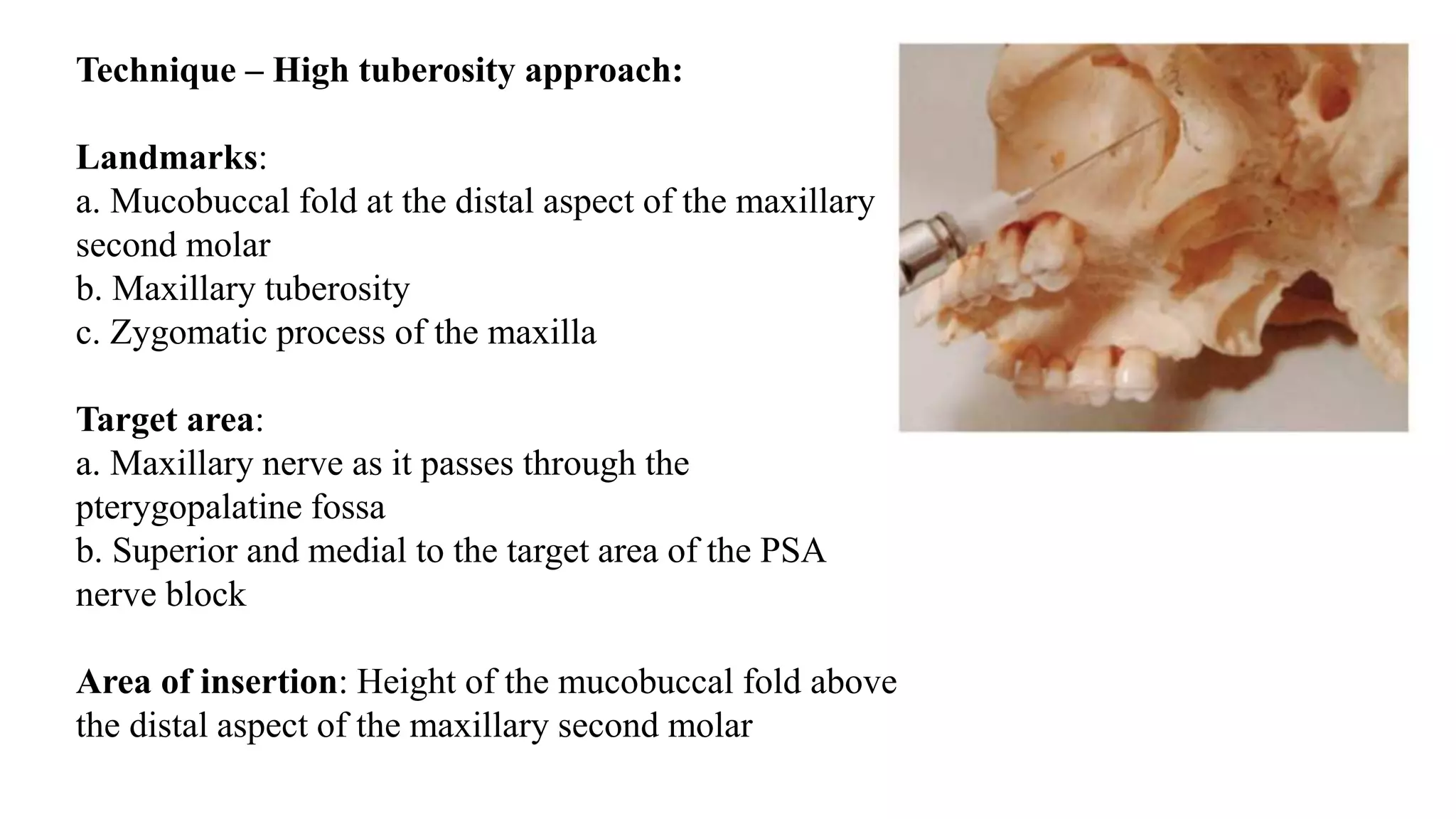
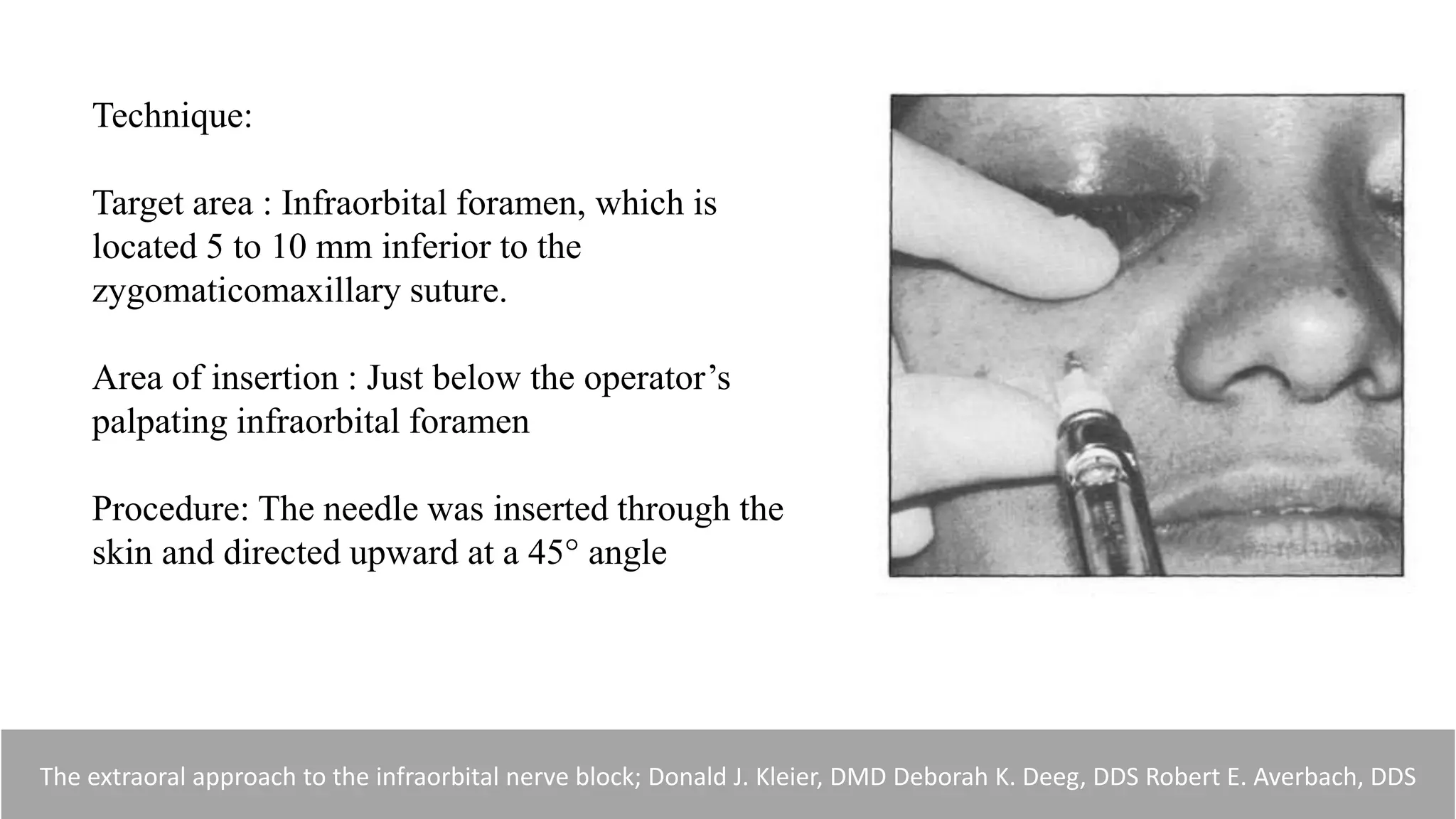
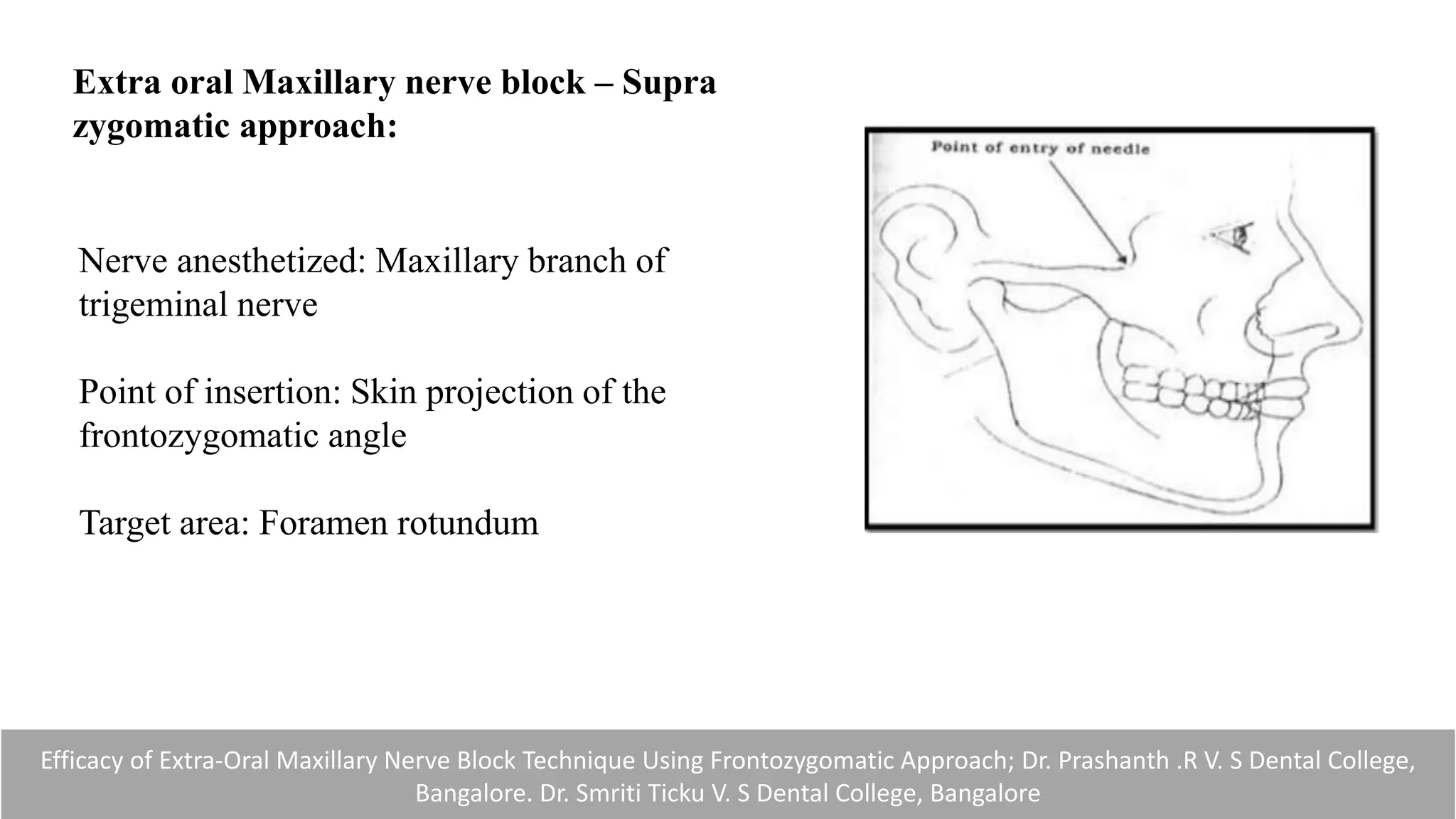
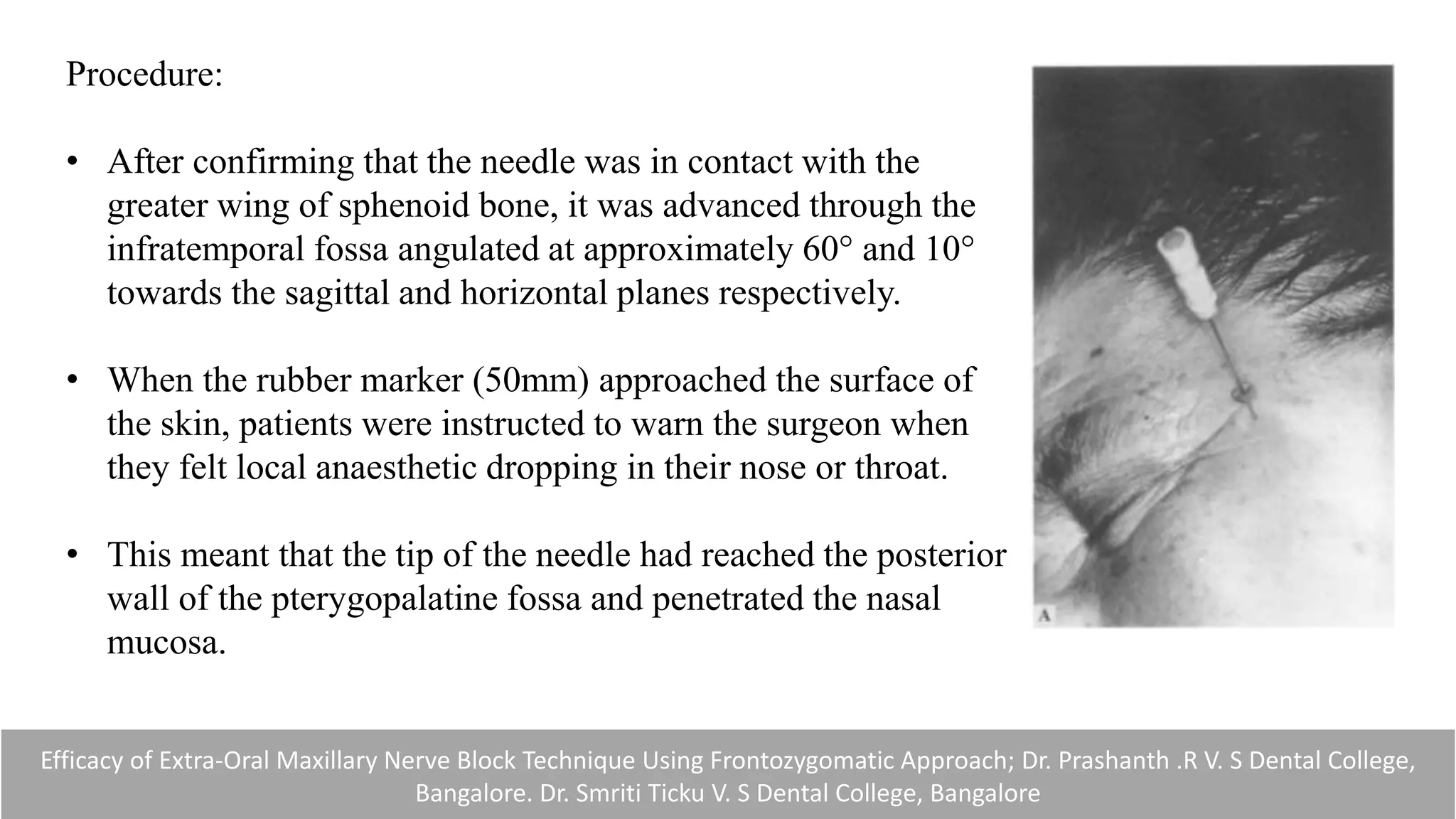
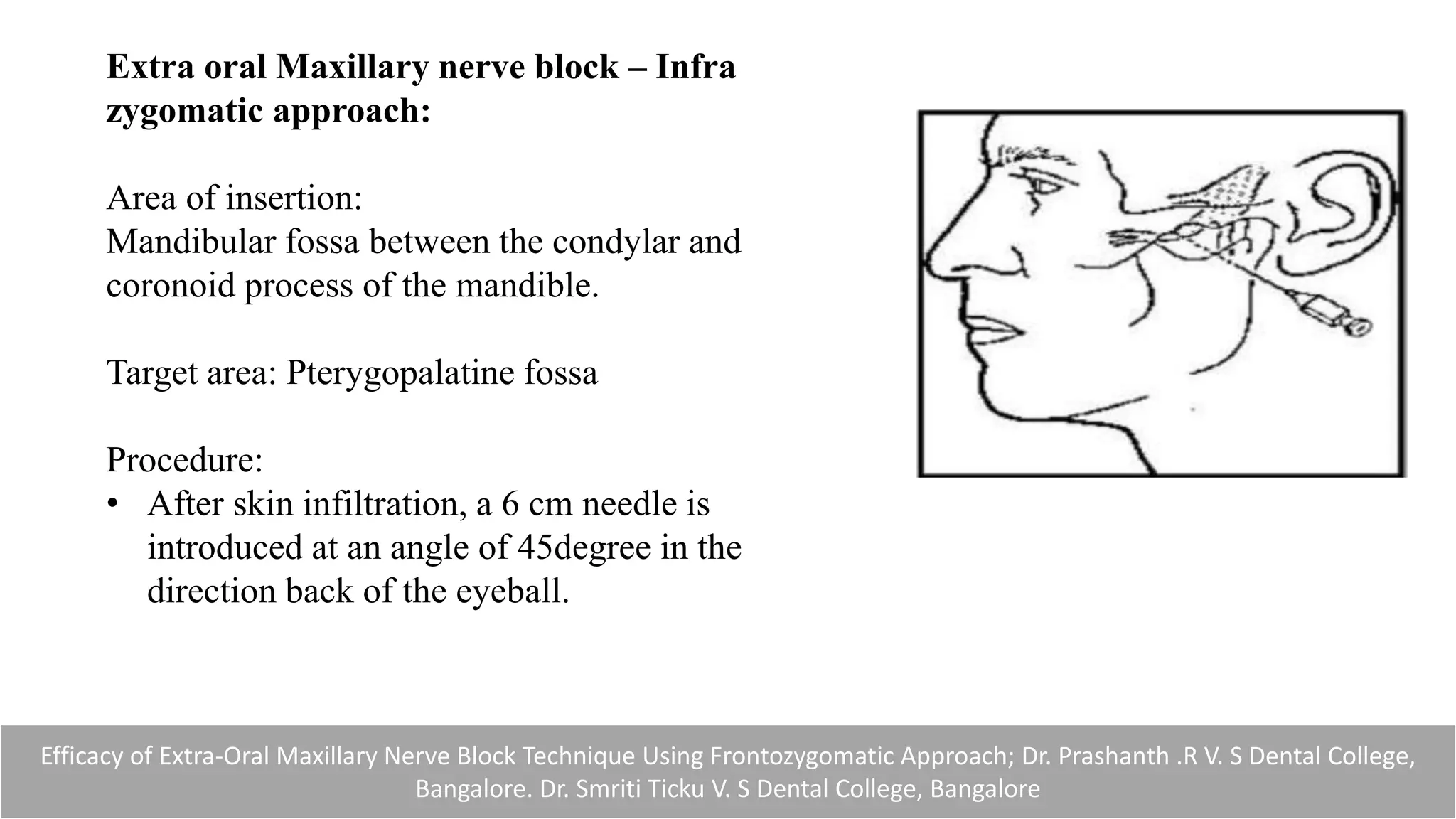
This document provides a comprehensive overview of maxillary nerve blocks, including anatomical details, local anesthesia techniques, and specific nerve block procedures. It outlines indications, techniques, complications, and management for various intra-oral and extra-oral techniques used in dental anesthesia. The document serves as a guide for dentists on effective pain management during dental procedures involving the maxillary region.