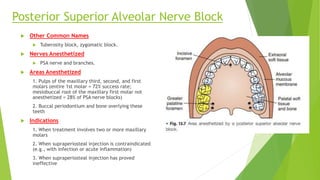
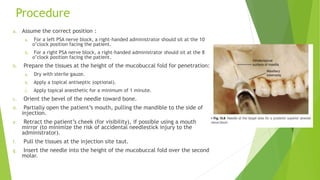
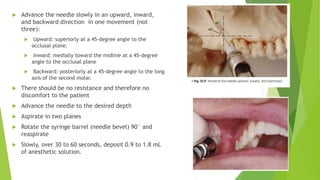
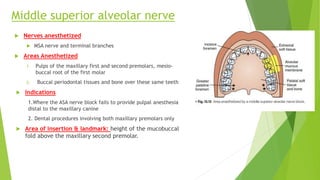
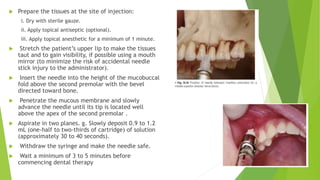
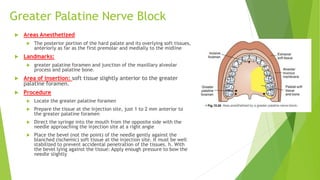
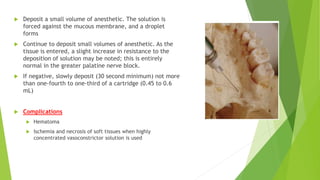
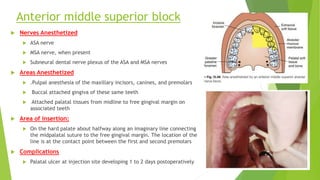
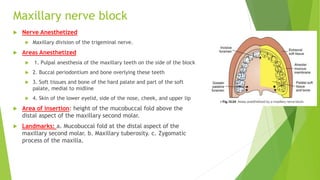
This document describes various techniques for injecting the maxilla to provide anesthesia for dental procedures. It discusses the posterior superior alveolar nerve block, middle superior alveolar nerve block, anterior superior alveolar nerve block, greater palatine nerve block, nasopalatine block, anterior middle superior block, and maxillary nerve block. For each technique, it provides the nerves anesthetized, areas anesthetized, landmarks, procedures, signs and symptoms, and potential complications. The goal is to select the appropriate injection based on the nature of the planned dental treatment.