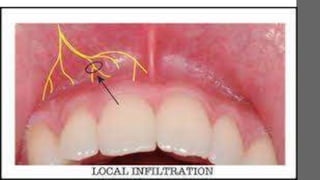
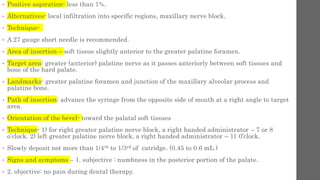
This document discusses various techniques for local anesthesia in dentistry. It describes different nerve blocks for anesthetizing specific regions of the maxilla and mandible, including the posterior superior alveolar nerve block, middle superior alveolar nerve block, and anterior superior alveolar (infraorbital) nerve block. It also covers maxillary injection techniques such as supraperiosteal injections and palatal anesthesia techniques like the greater palatine nerve block.