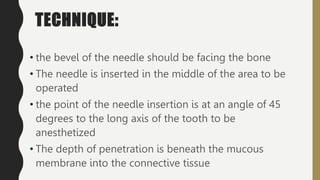
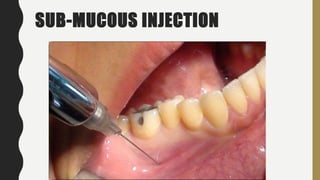
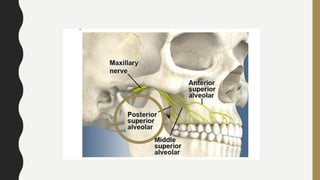
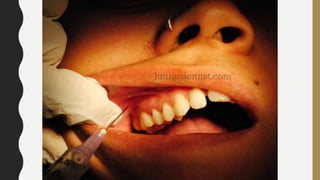
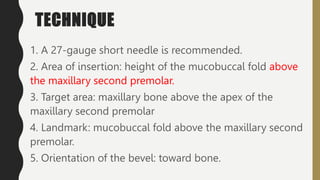
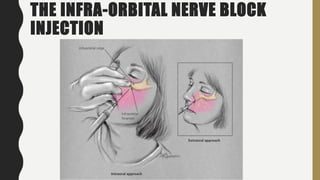
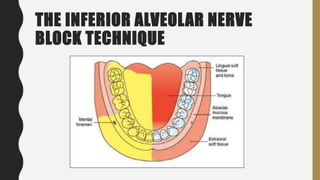
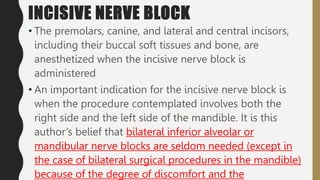
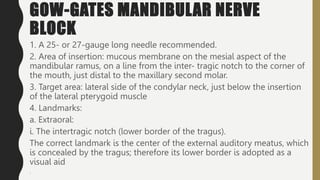
This document discusses techniques for local anesthesia in dentistry. It describes four main types of local anesthesia: topical, infiltration, field block, and regional block. Infiltration anesthesia involves depositing the anesthetic solution near terminal nerve fibers to infiltrate the tissue and anesthetize a localized area. It is commonly used for the front of the maxilla and mandible. Regional block anesthesia deposits the solution near the main nerve trunk to anesthetize a larger area. The document provides details on specific infiltration and regional block techniques for anesthetizing different areas of the maxilla and palate.