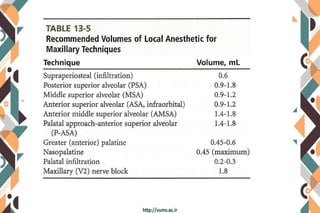
The document provides information on various types of maxillary anesthesia techniques:
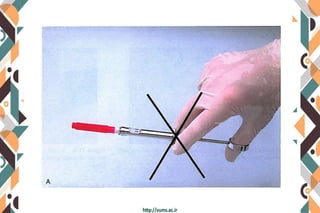
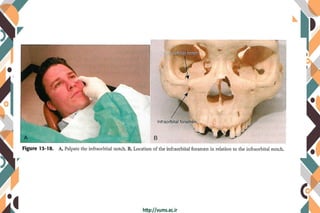
1. Supraperiosteal injection is commonly used to anesthetize one or two maxillary teeth and soft tissues. It has a low risk of intravascular administration.
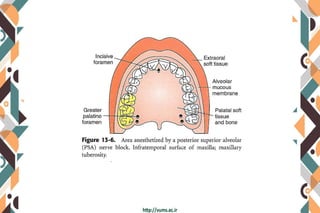
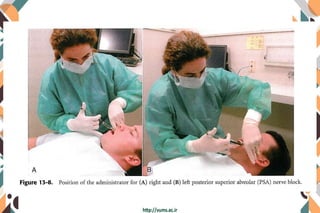
2. Posterior superior alveolar nerve block anesthetizes maxillary molars and buccal tissues through the posterior superior alveolar nerve. It has a high success rate but risks hematoma formation.
3. Nasopalatine nerve block provides wide palatal soft tissue anesthesia using a minimum volume of local anesthetic, minimizing the need for multiple injections.