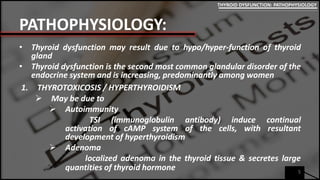
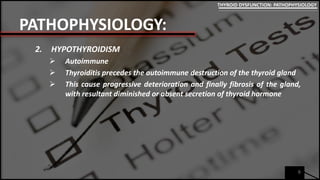
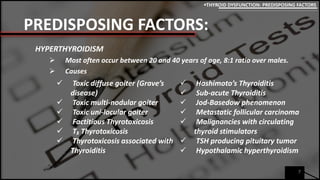
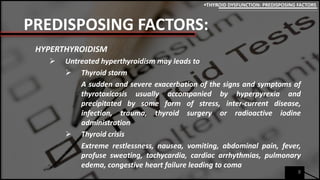
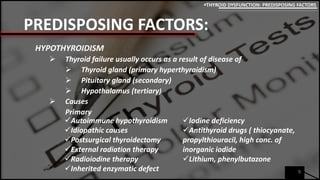
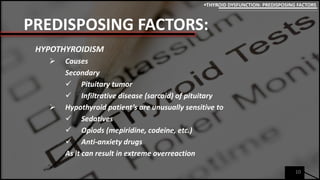
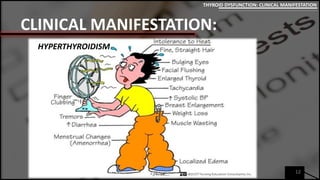
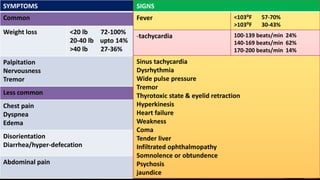
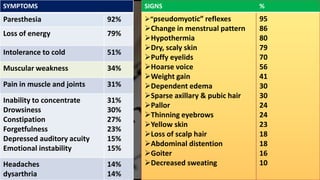
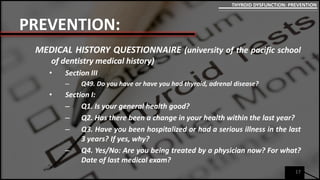
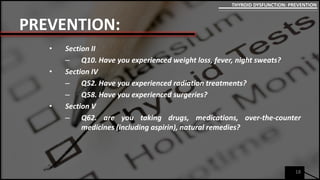
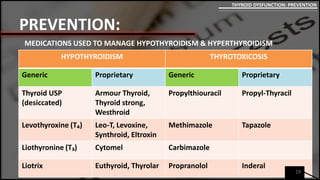
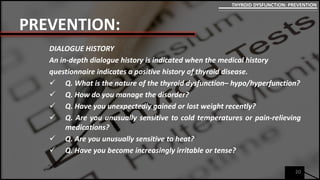
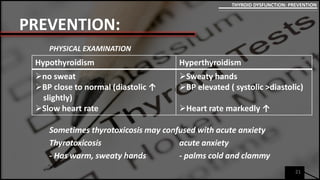
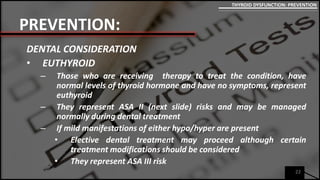
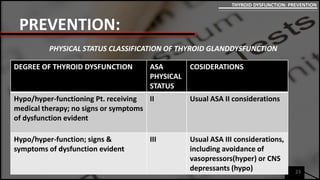
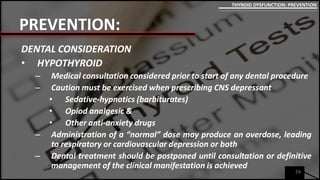
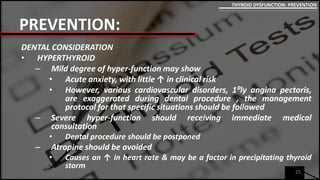
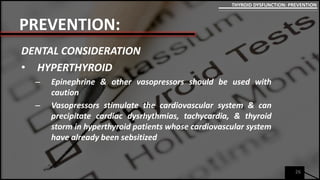
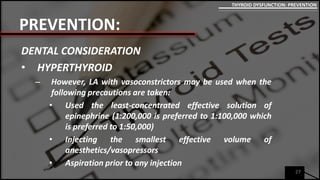
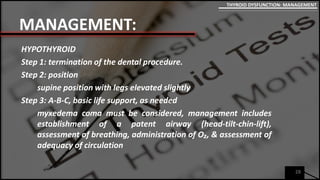
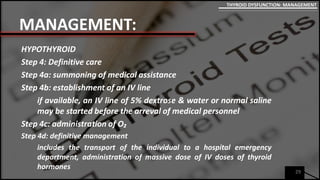
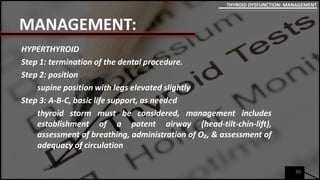
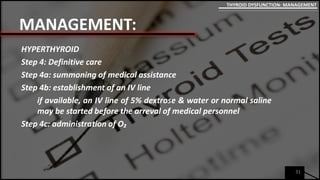
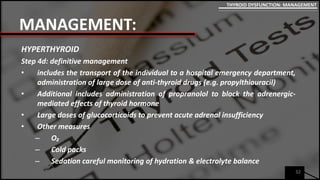
This document discusses thyroid dysfunction, including hyperthyroidism and hypothyroidism. It covers the pathophysiology, predisposing factors, clinical manifestations, prevention, and management. Regarding prevention in dental care, patients with thyroid conditions may require medical consultation and modified treatment to avoid exacerbating their condition through the use of certain medications like sedatives, vasopressors, or CNS depressants. Precautions are especially important for hypothyroid and severe hyperthyroid patients.