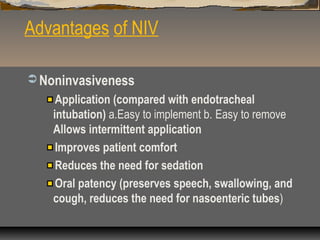
Noninvasive ventilation (NIV) delivers ventilatory support without an invasive airway. It works by reducing inspiratory muscle work and avoiding fatigue. NIV improves lung compliance and gas exchange while allowing oral intake and speech. The main advantages of NIV are that it is noninvasive and avoids complications of intubation. Potential disadvantages include slower correction of abnormalities and issues with masks like leaks or skin damage. NIV can be administered in emergency departments or wards by trained staff and is used to treat conditions like COPD exacerbations, cardiogenic pulmonary edema, and post-extubation respiratory failure.