vital role
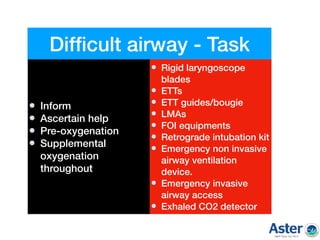
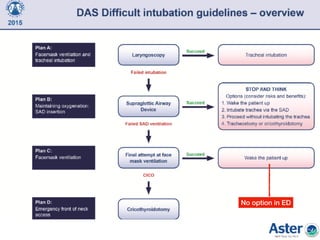
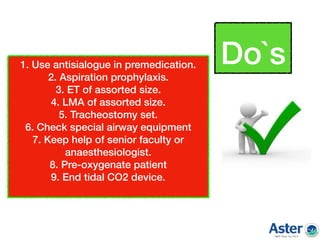
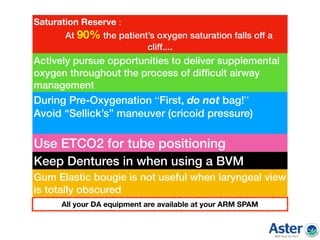
Pre-oxygenation: vital
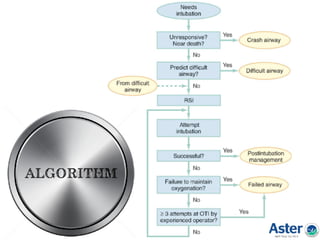
Awake intubation: consider
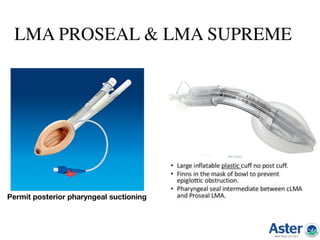
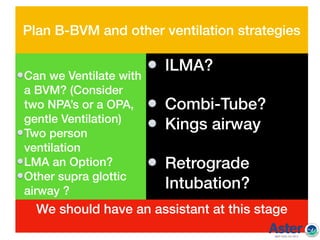
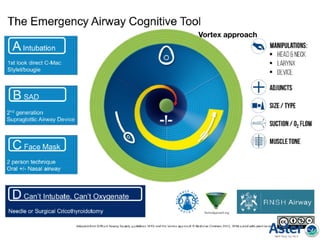
Alternative airway: have ready
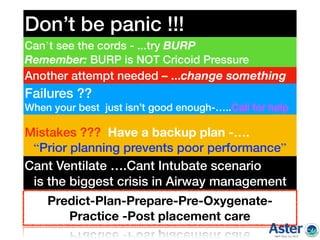
Senior help: call early
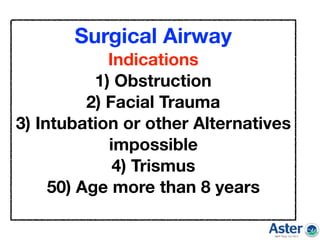
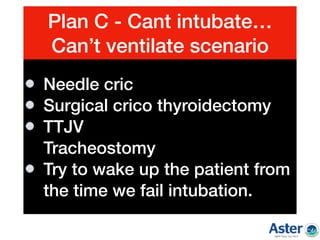
Cricothyrotomy: know how to do
Postpone if not urgent
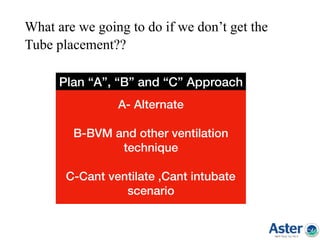
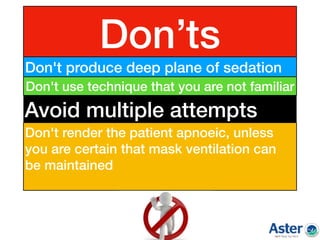
Don't panic, think and act
Document: vitally important
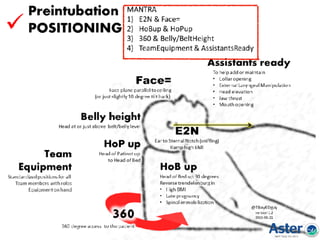
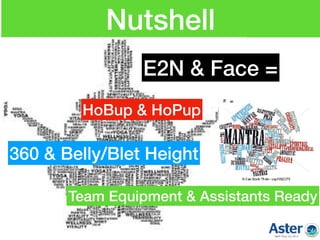
Prepare for worst
Train and practice regularly
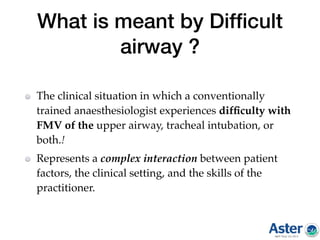
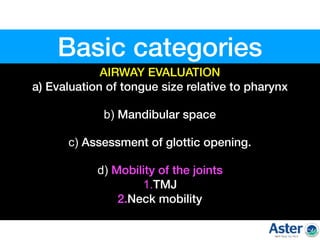
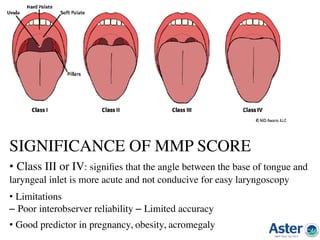
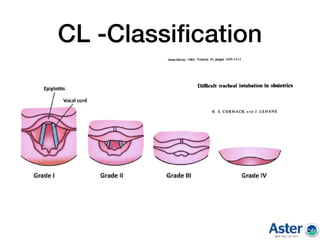
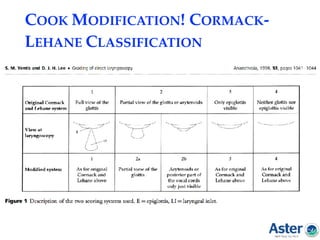
![1.Individual indices
2.Group indices
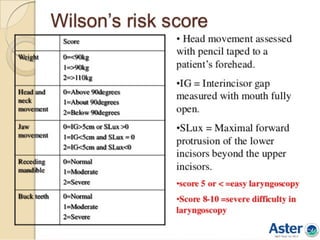
Wilson’s score
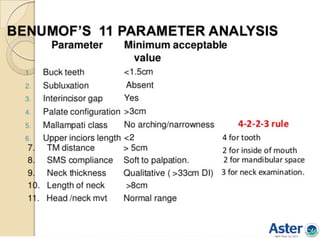
Benumof’s analysis
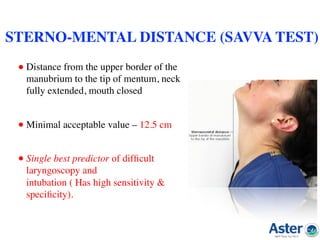
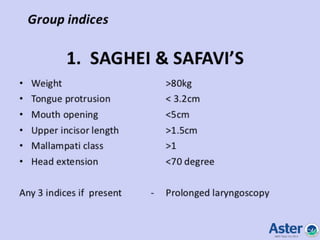
Saghei & safavi test
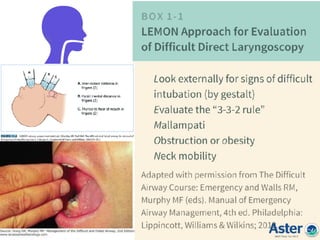
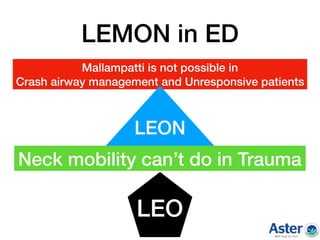
Lemon assesment
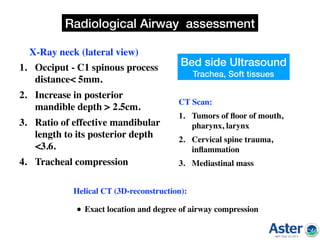
3.Radiological indices
Airway assessment indices
a)X Ray Neck[Lataral]
b)CT Scan
c)Helical CT
d)USG
4.Advanced
indices
• Flow volume
loop
• Acoustic
response
measurement
• Ultra sound
guided
• CT/MRI
• Flexible
bronchoscope](https://image.slidesharecdn.com/airwaypushpagiri-180429065526/85/Difficult-airway-Made-easy-9-320.jpg)