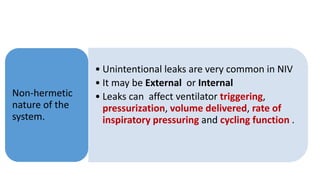
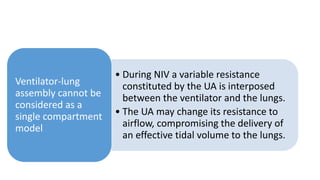
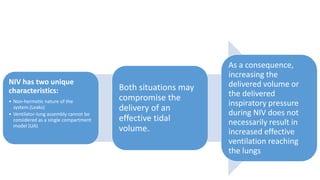
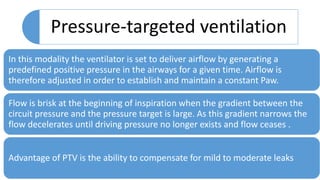
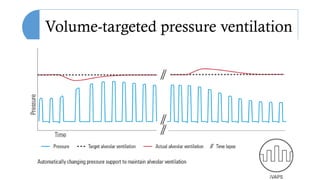
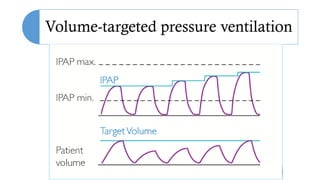
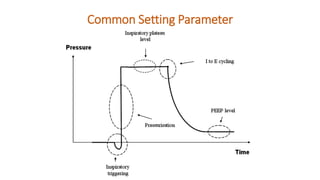
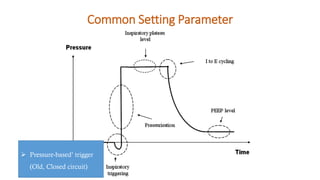
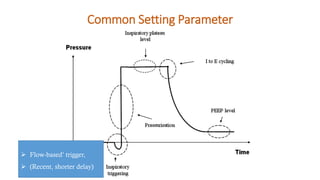
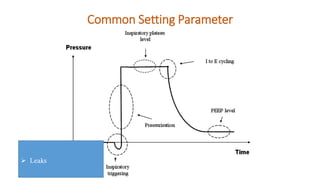
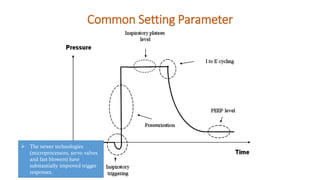
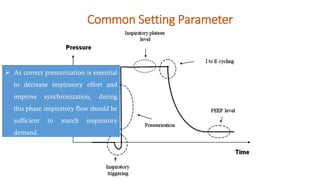
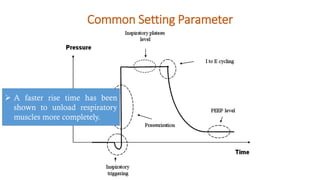
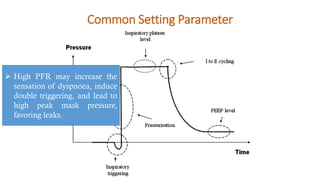
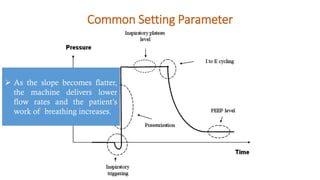
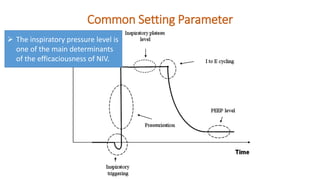
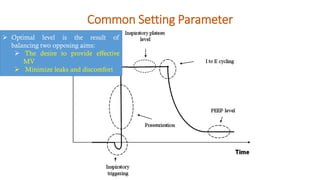
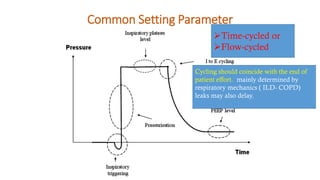
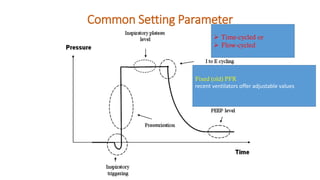
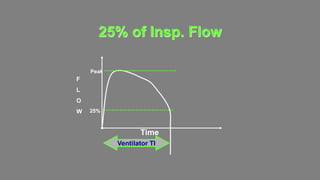
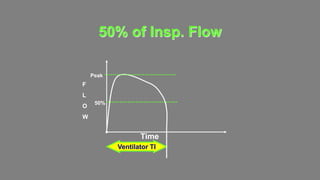
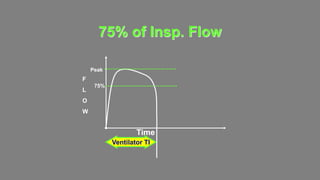
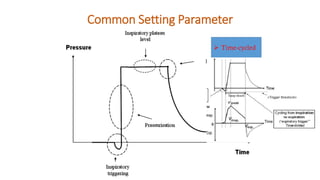
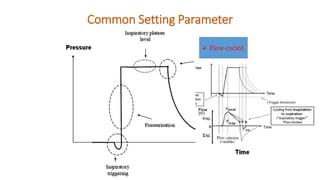
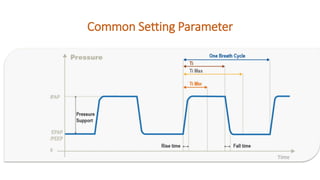
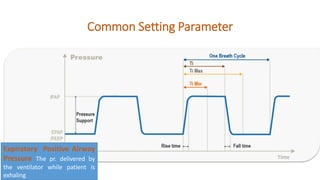
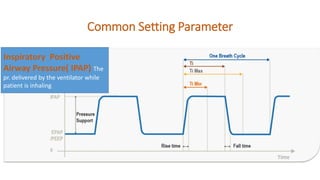
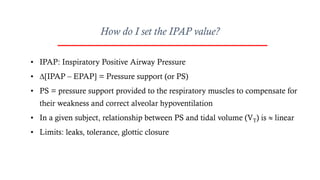
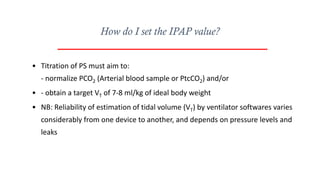
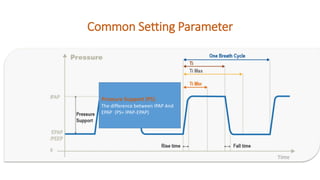
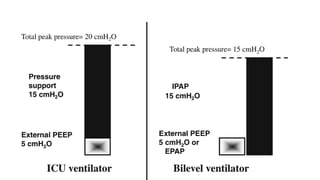
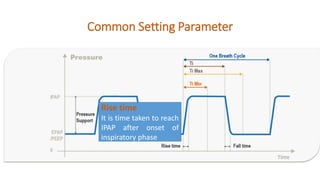
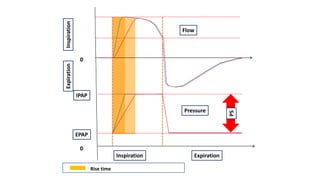
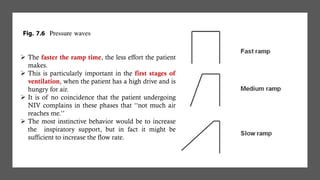
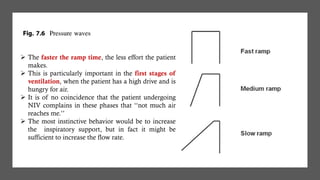
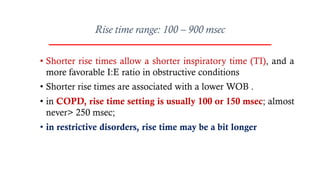
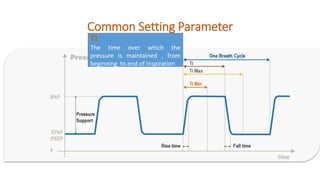
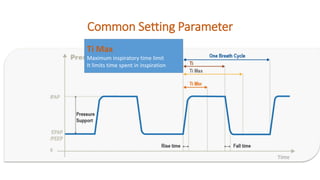
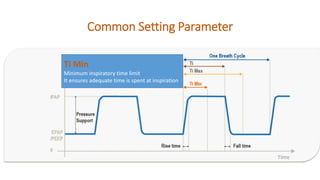
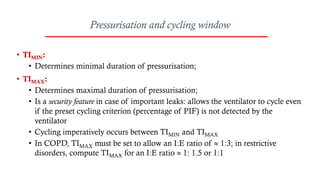
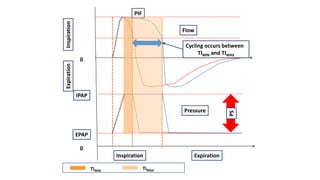
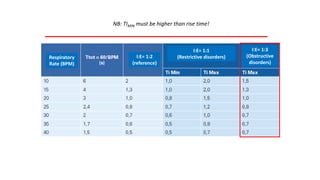
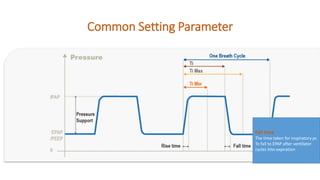
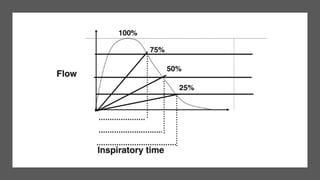
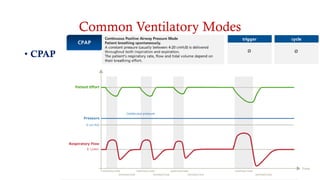
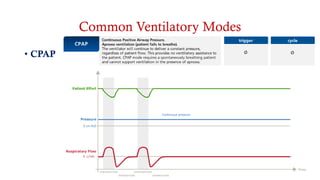
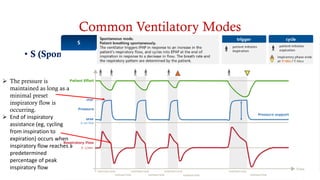
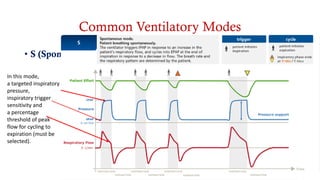
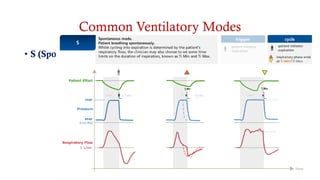
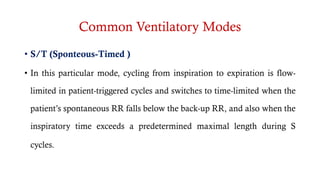
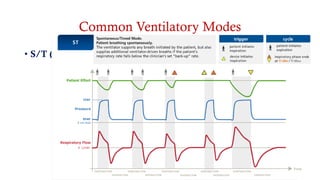
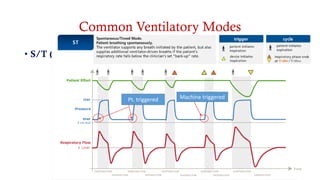
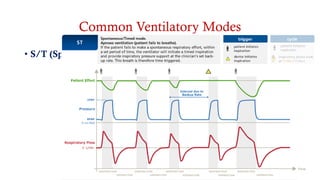
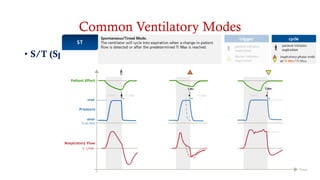
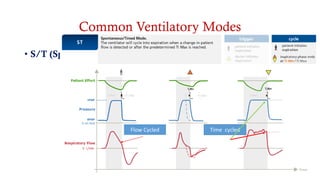
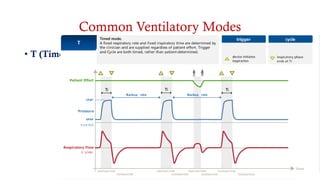
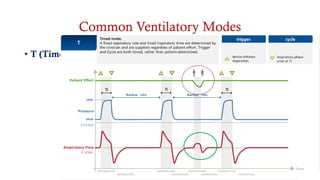
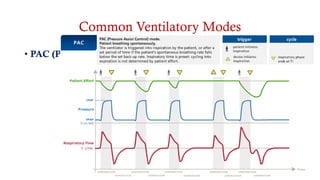
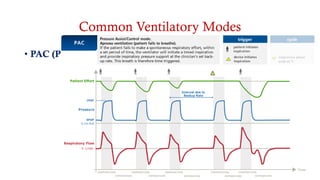
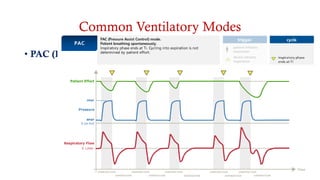
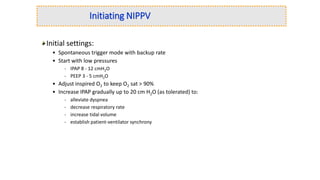
This document discusses various ventilatory modes and settings used in non-invasive ventilation (NIV). It begins by explaining the unique characteristics of NIV, namely the non-hermetic nature of the system due to leaks, and the variable resistance of the upper airway. It then describes common ventilator modes for NIV including spontaneous, spontaneous-timed, pressure assist control, and timed modes. The document outlines optimal settings for various parameters such as inspiratory and expiratory pressure, pressure support, rise time, inspiratory time and cycling criteria. It emphasizes titrating settings to achieve adequate ventilation while minimizing patient effort and discomfort.