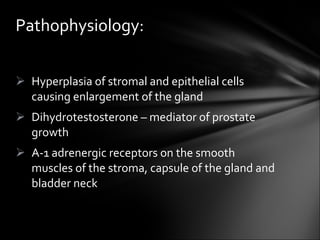
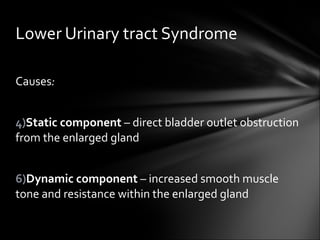
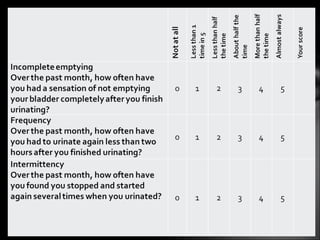
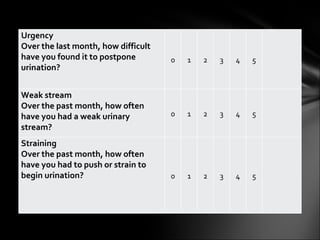
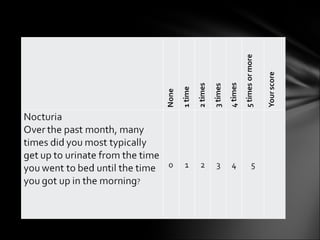
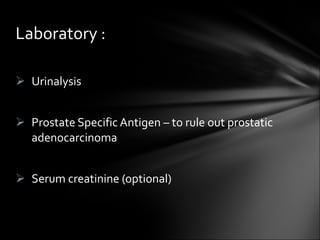
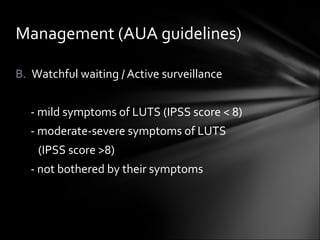
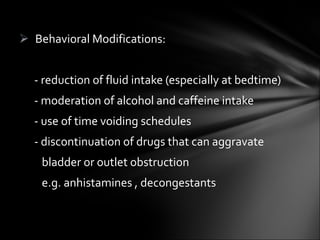
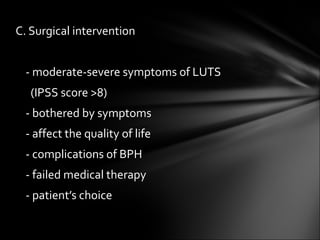
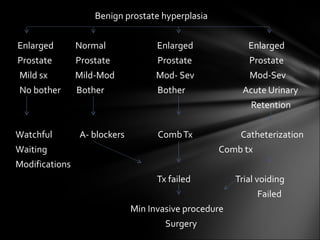
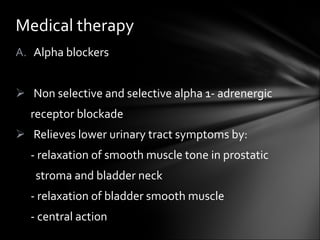
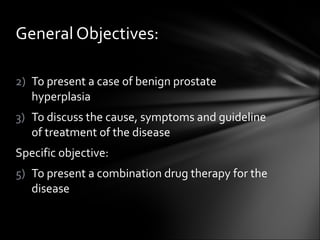
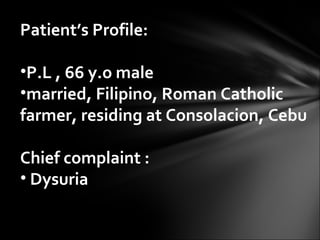
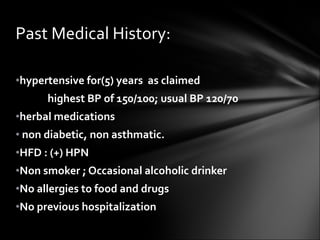
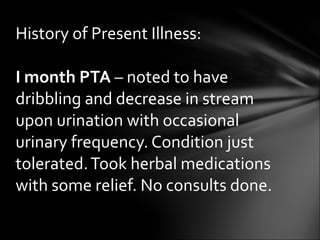
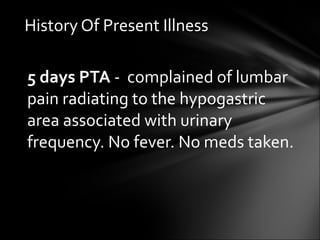
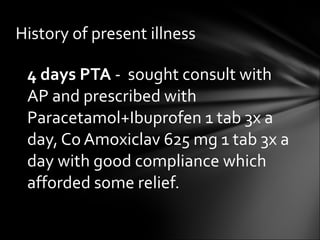
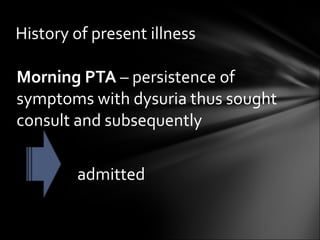
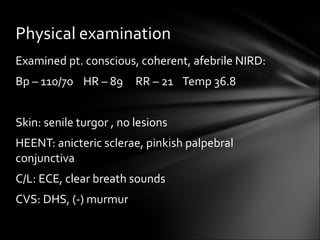
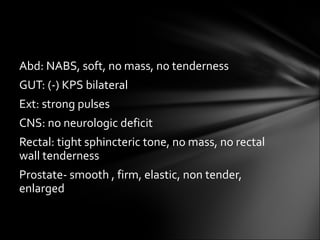
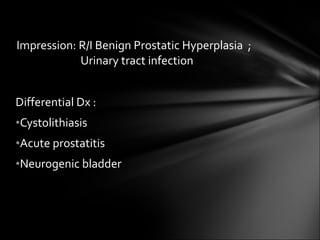
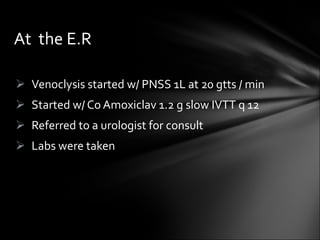
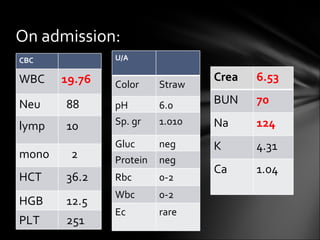
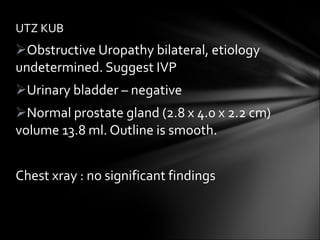
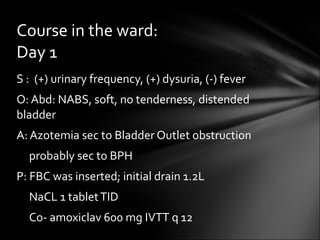
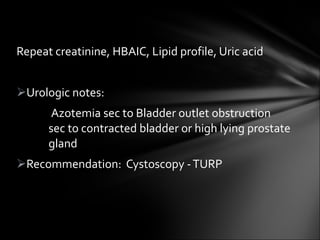
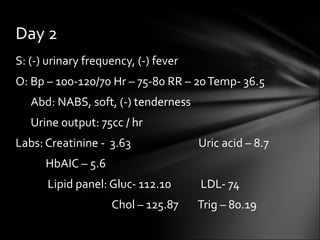
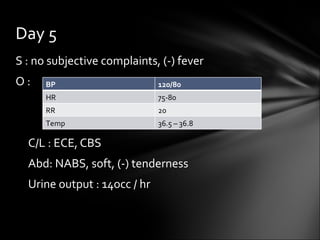
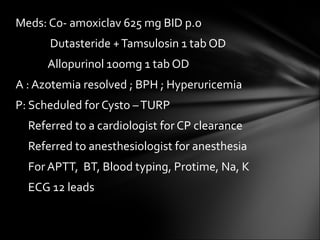
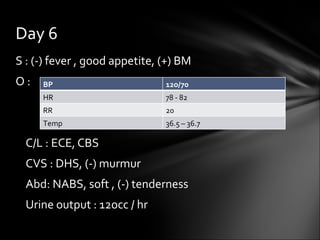
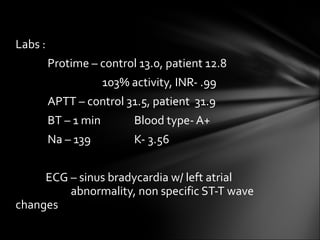
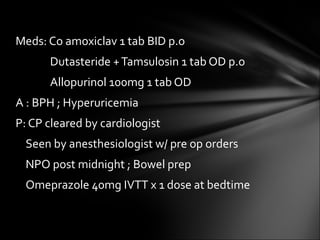
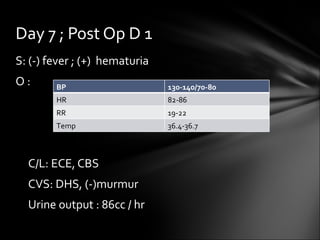
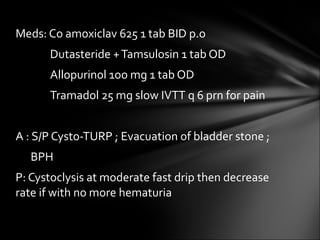
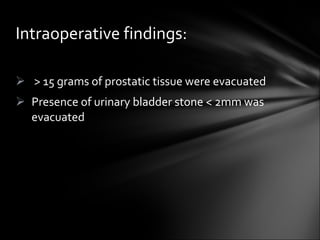
This case report summarizes the treatment of a 66-year-old male patient presenting with benign prostatic hyperplasia (BPH). The patient reported symptoms of dysuria, urinary frequency, and lumbar pain. Physical examination and tests revealed an enlarged prostate, elevated creatinine, and urinary tract infection. The patient was treated with antibiotics and combination drug therapy. He later underwent a cystoscopy and transurethral resection of the prostate, which successfully resolved his symptoms.


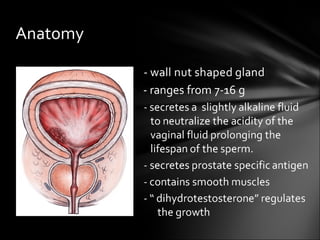
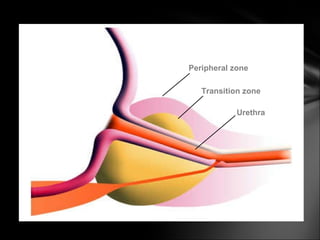
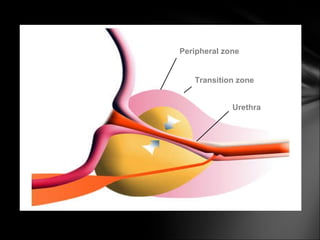
![Name Fraction of gland Description Peripheral zone (PZ) Up to 70% in young men It is from this portion of the gland that ~70-80% of prostatic cancers originate. [14] [15] Central zone (CZ) Approximately 25% normally This zone surrounds the ejaculatory ducts. Transition zone (TZ) 5% at puberty The transition zone surrounds the proximal urethra and is the region of the prostate gland that grows throughout life and is responsible for the disease of benign prostatic enlargement Anterior fibro-muscular zone (or stroma) Approximately 5% This zone is usually devoid of glandular components, and composed only, as its name suggests, of muscle and fibrous tissue .](https://image.slidesharecdn.com/powergrandrounds-111116022703-phpapp01/85/Benigh-prostatic-hyperplasia-38-320.jpg)