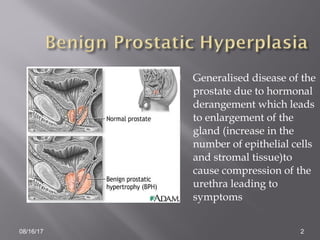
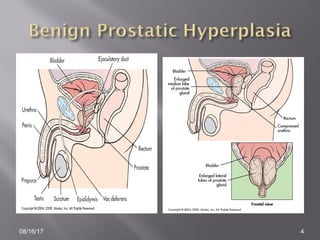
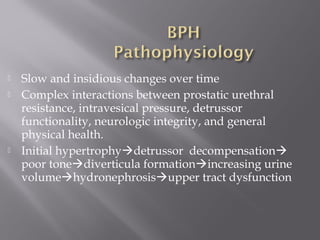
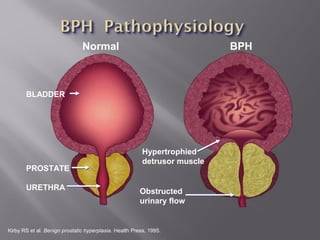
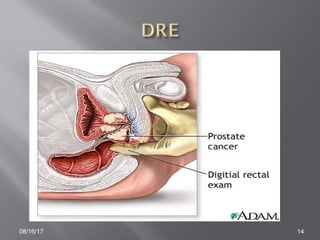
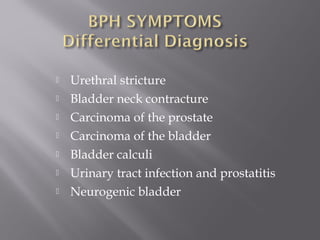
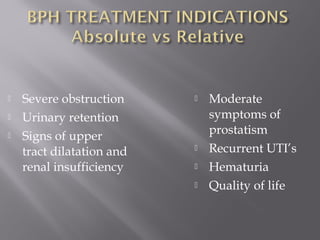
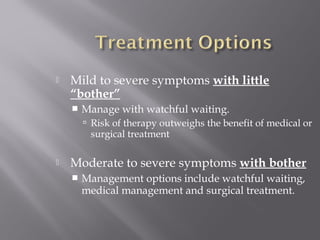
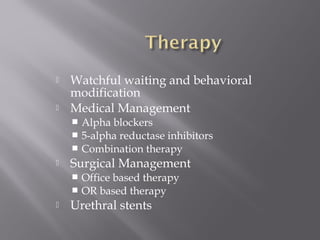
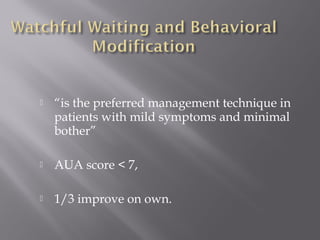
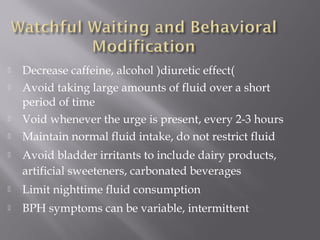
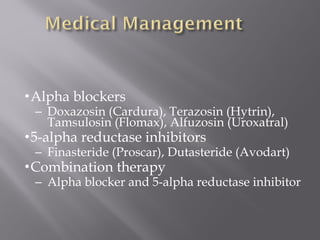
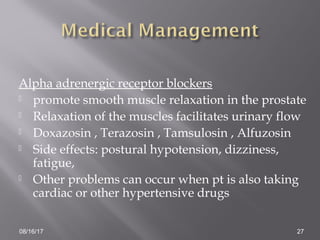
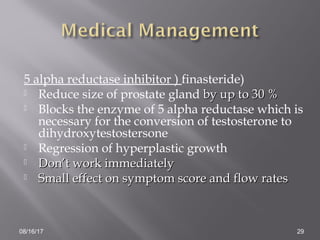
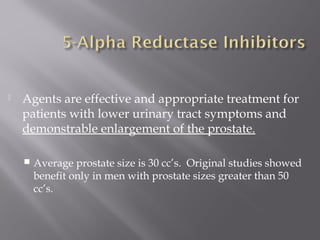
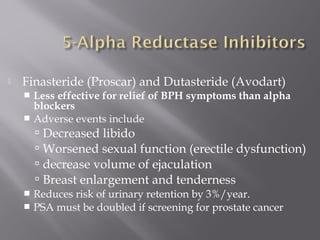
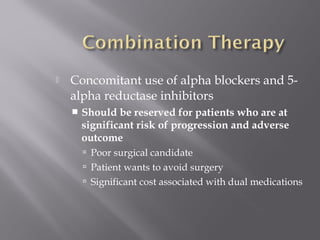
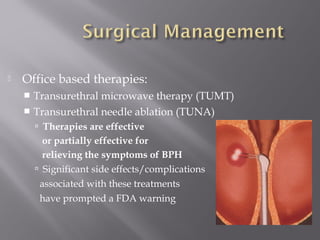
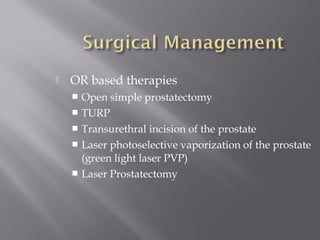
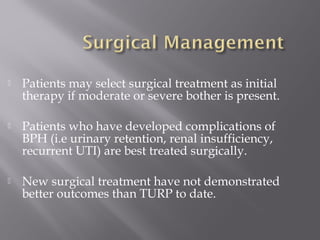
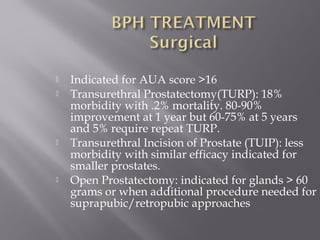
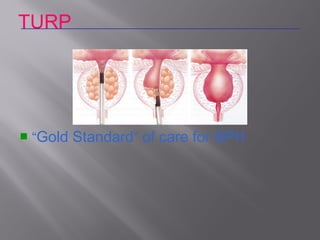
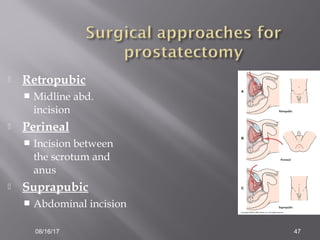
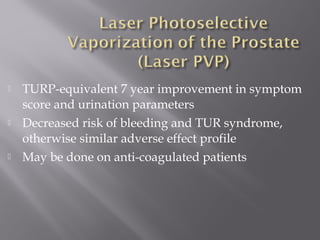
Benign prostatic hyperplasia (BPH) is a non-cancerous enlargement of the prostate gland that occurs in many men as they age. It is caused by hormonal changes that lead to increased cell growth in the prostate. BPH causes compression of the urethra and urinary symptoms like frequent urination, weak stream, and incomplete emptying. Treatment options include watchful waiting for mild symptoms, medication to reduce symptoms, or surgery for more severe cases. Surgical options range from minimally invasive procedures to more invasive options like transurethral resection of the prostate (TURP).