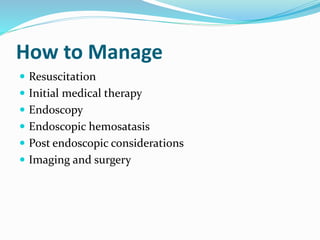
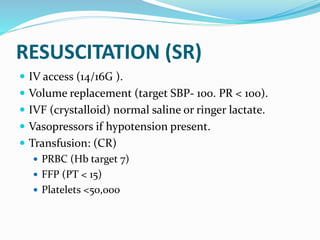
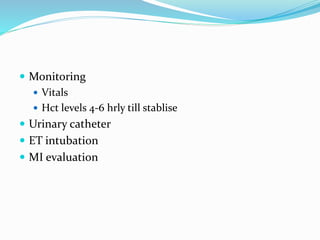
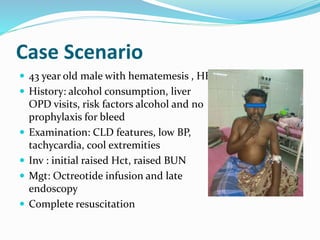
1) Aggressive resuscitation for hemorrhagic shock including IV fluids and blood products.
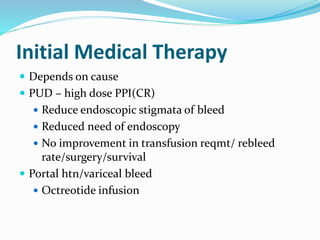
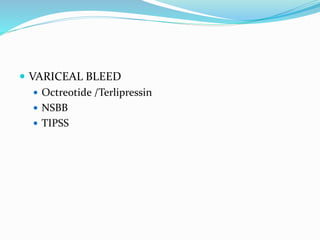
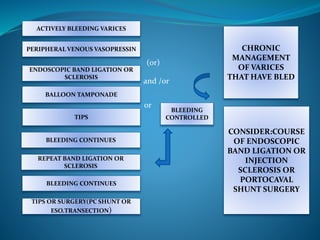
2) Octreotide infusion to help control bleeding.
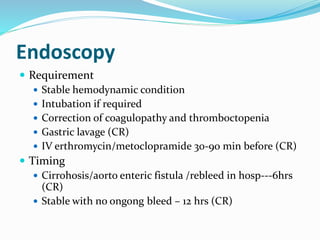
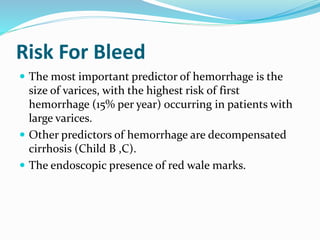
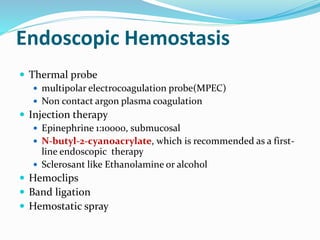
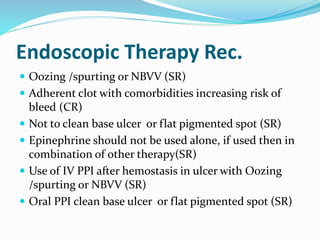
3) Early upper endoscopy within 12 hours to identify the source of bleeding and perform band ligation or sclerotherapy if varices are identified.
4) Continued medical therapy and monitoring to prevent rebleeding, along with counseling on abstaining from further alcohol use to help manage the underlying liver disease.