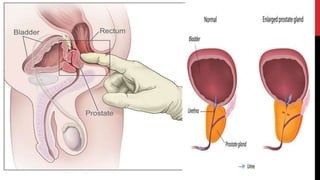
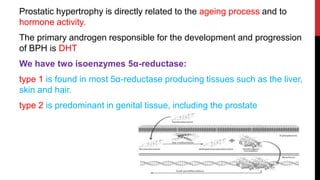
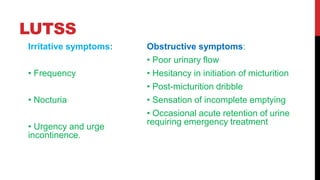
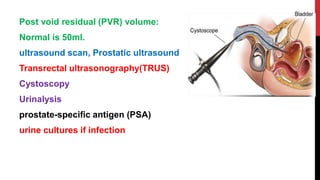
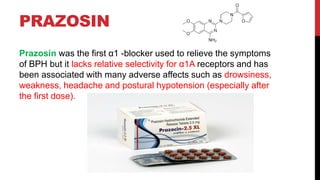
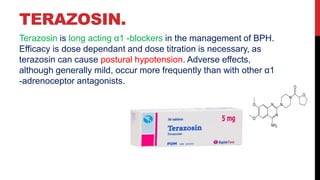
A 64-year-old man experiences poor urinary flow and nocturnal urination, with symptoms indicating potential benign prostatic hyperplasia (BPH), prostatitis, or prostate cancer. Diagnosis involves various investigations including digital rectal examination and ultrasound, while management may include watchful waiting, pharmacotherapy with α1-blockers or 5α-reductase inhibitors, and surgical options if necessary. Recommendations for managing lower urinary tract symptoms include lifestyle adjustments and bladder training.