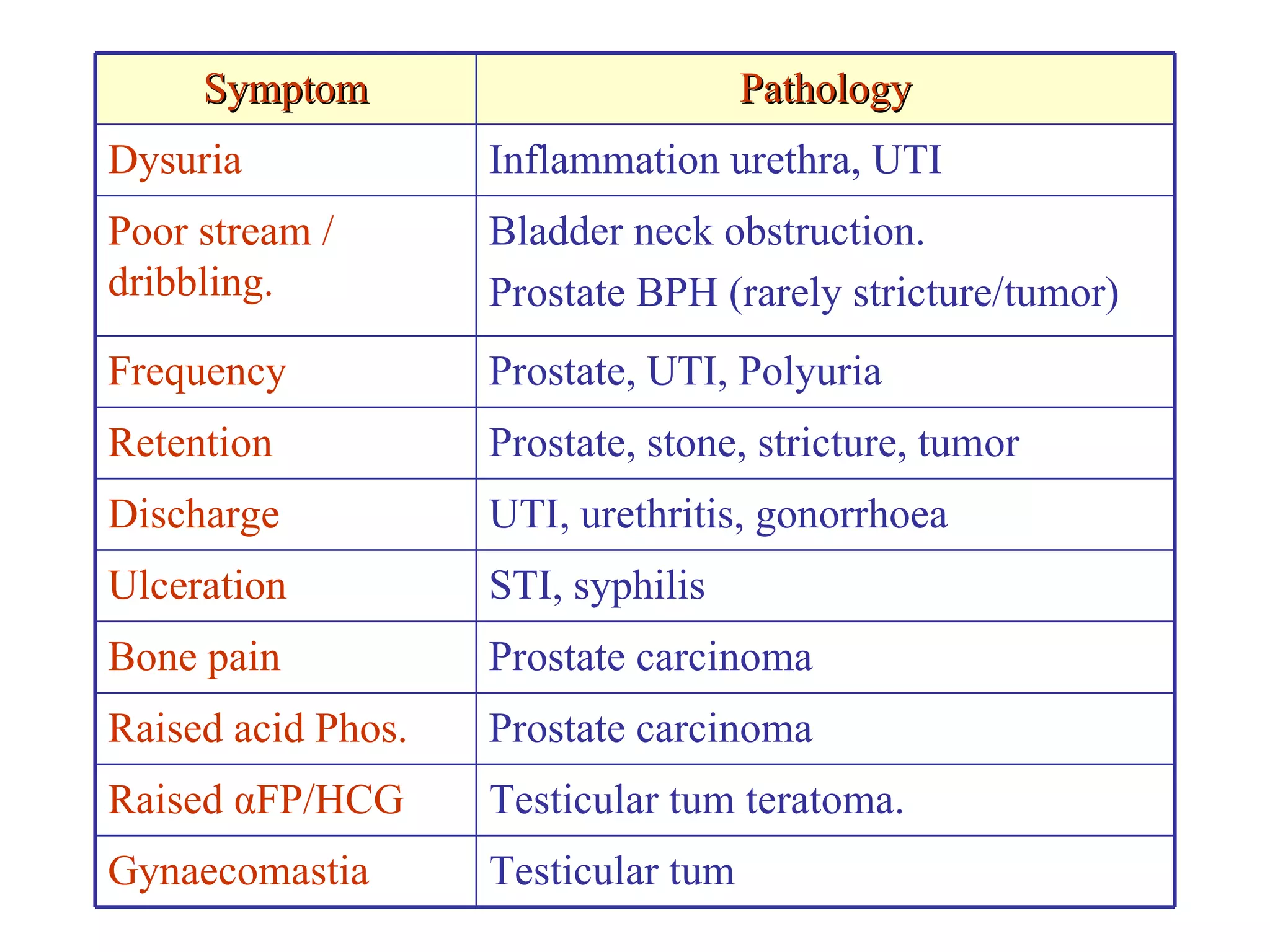
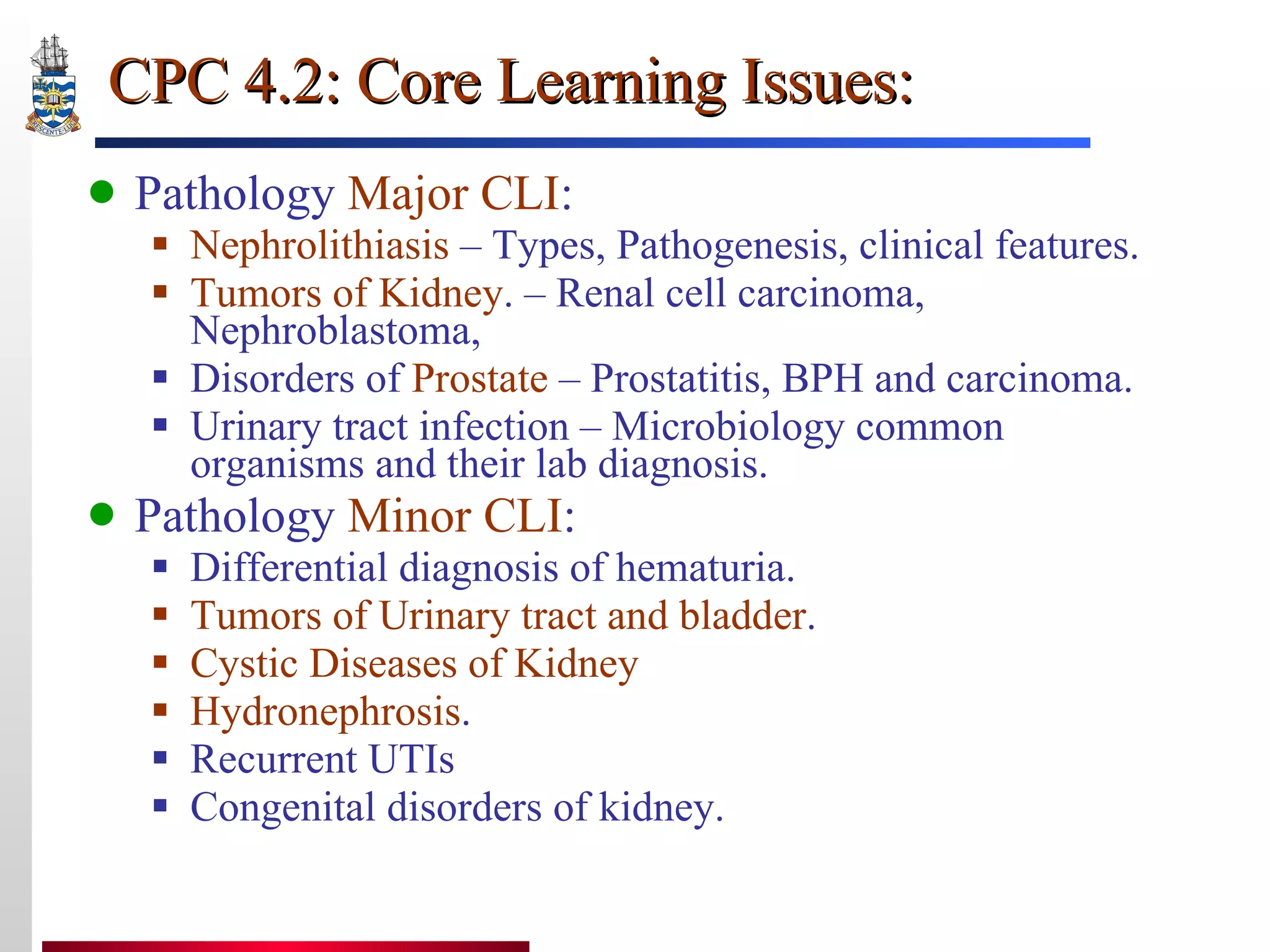
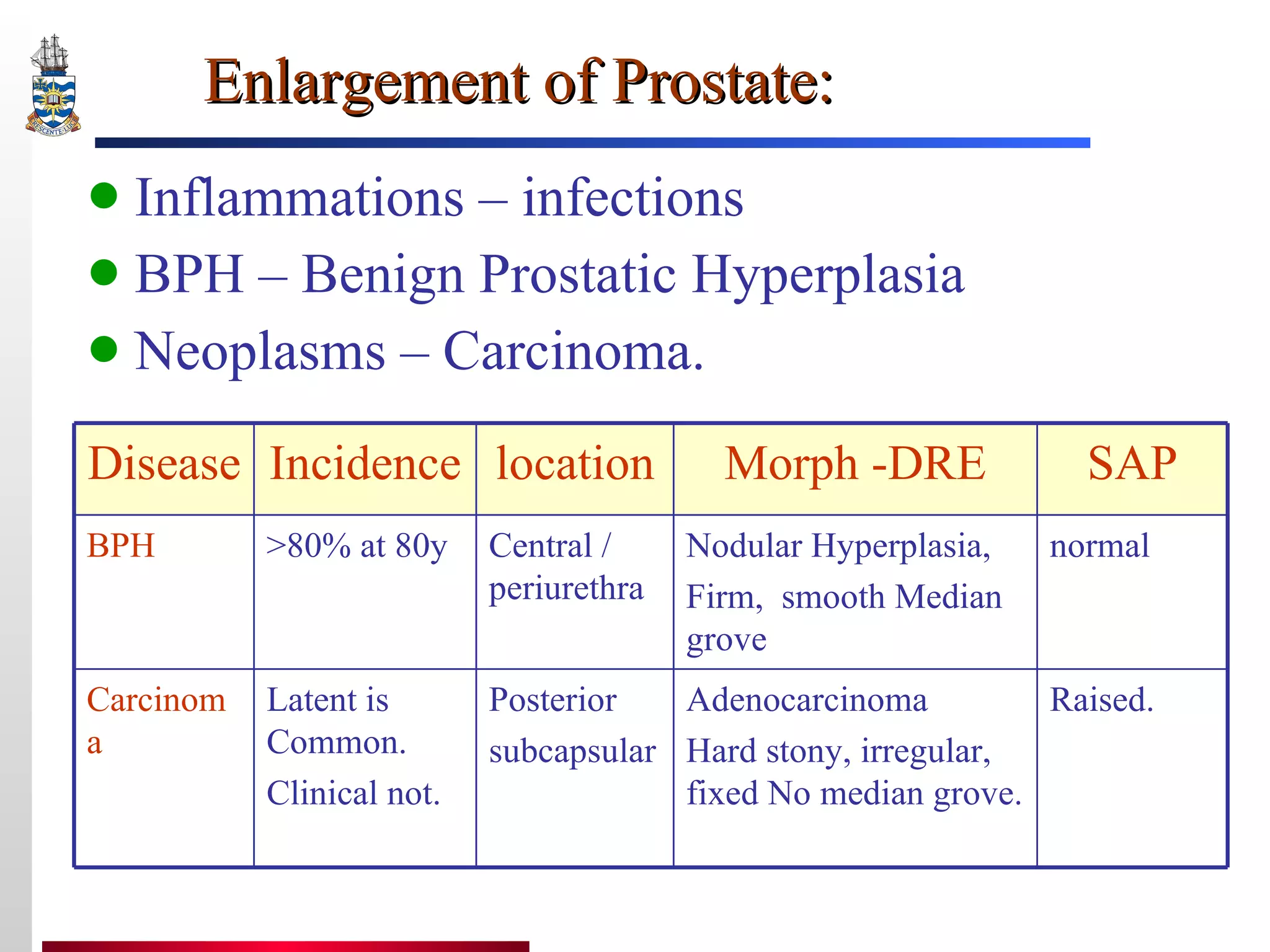
This 68-year-old male carpenter presents with urinary symptoms including frequency, urgency, terminal dribbling, poor stream, and occasional incontinence. His differential diagnosis includes benign prostatic hyperplasia, prostatitis, prostate cancer, stones, and other causes. Further workup is needed to determine the underlying pathology and guide treatment.