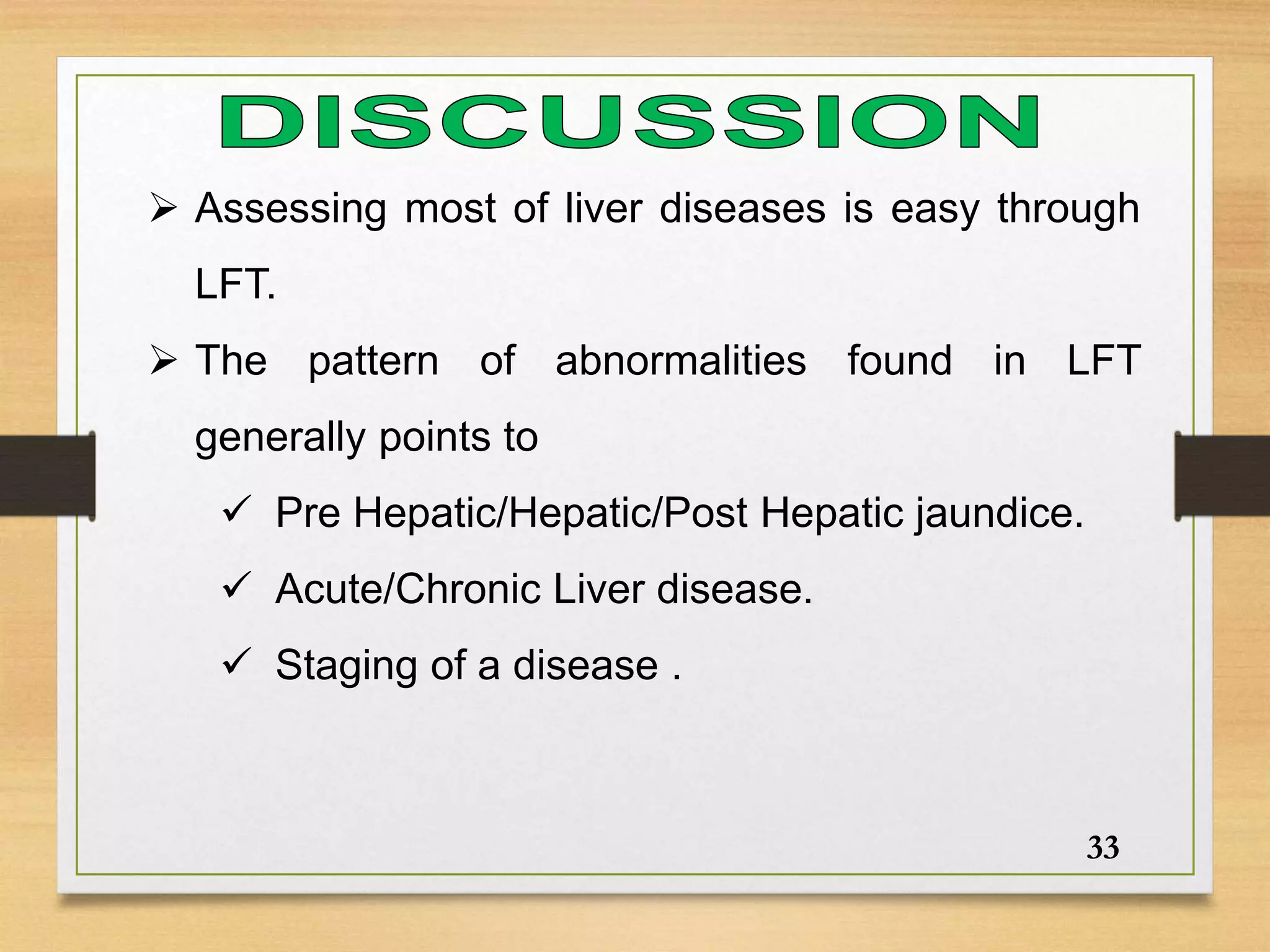
This document discusses liver function tests (LFTs) and their role in diagnosing and managing different types of jaundice (kamala) according to Ayurveda. It covers:
1. The functions of the liver and an overview of LFTs and the values they indicate.
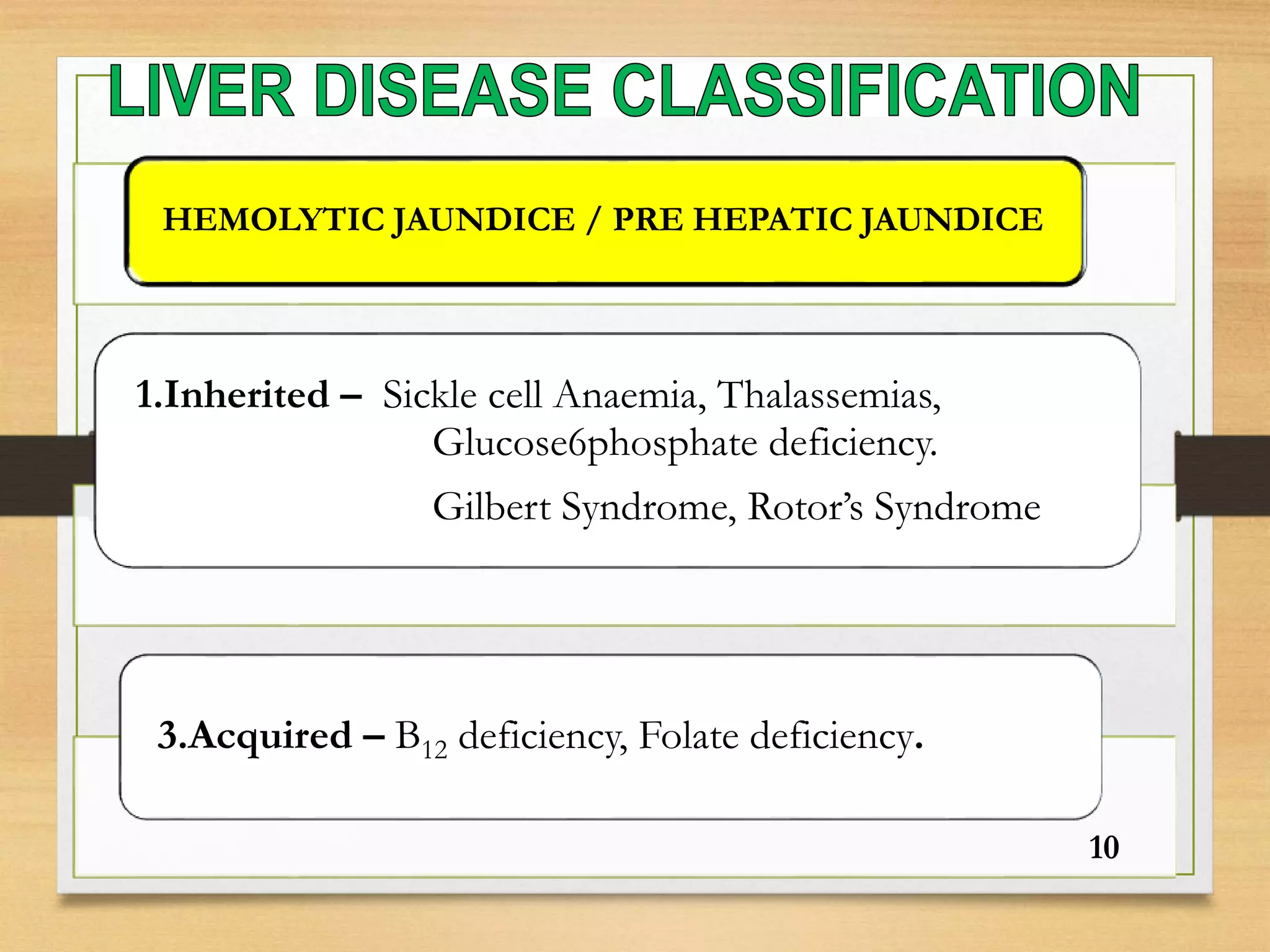
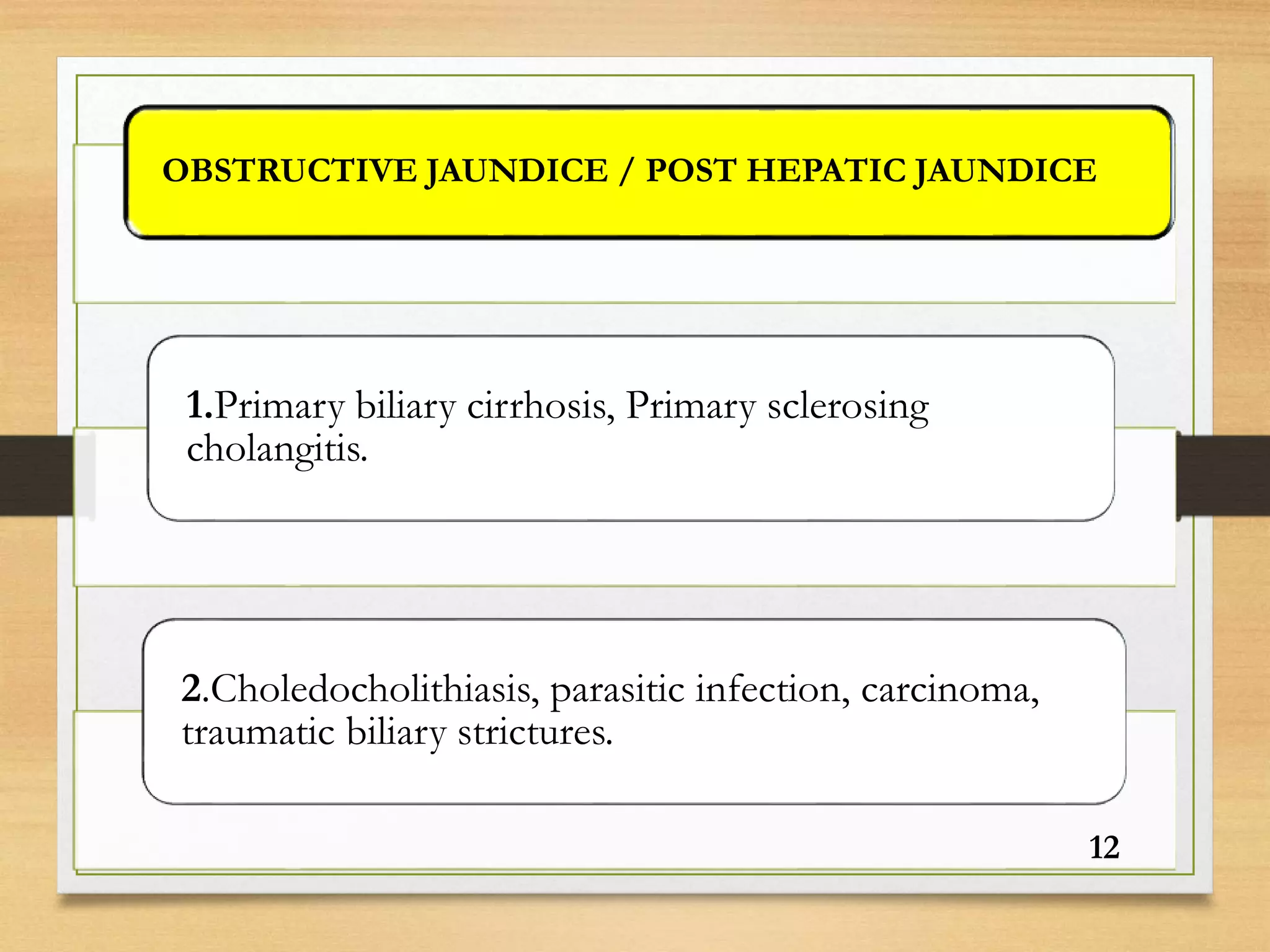
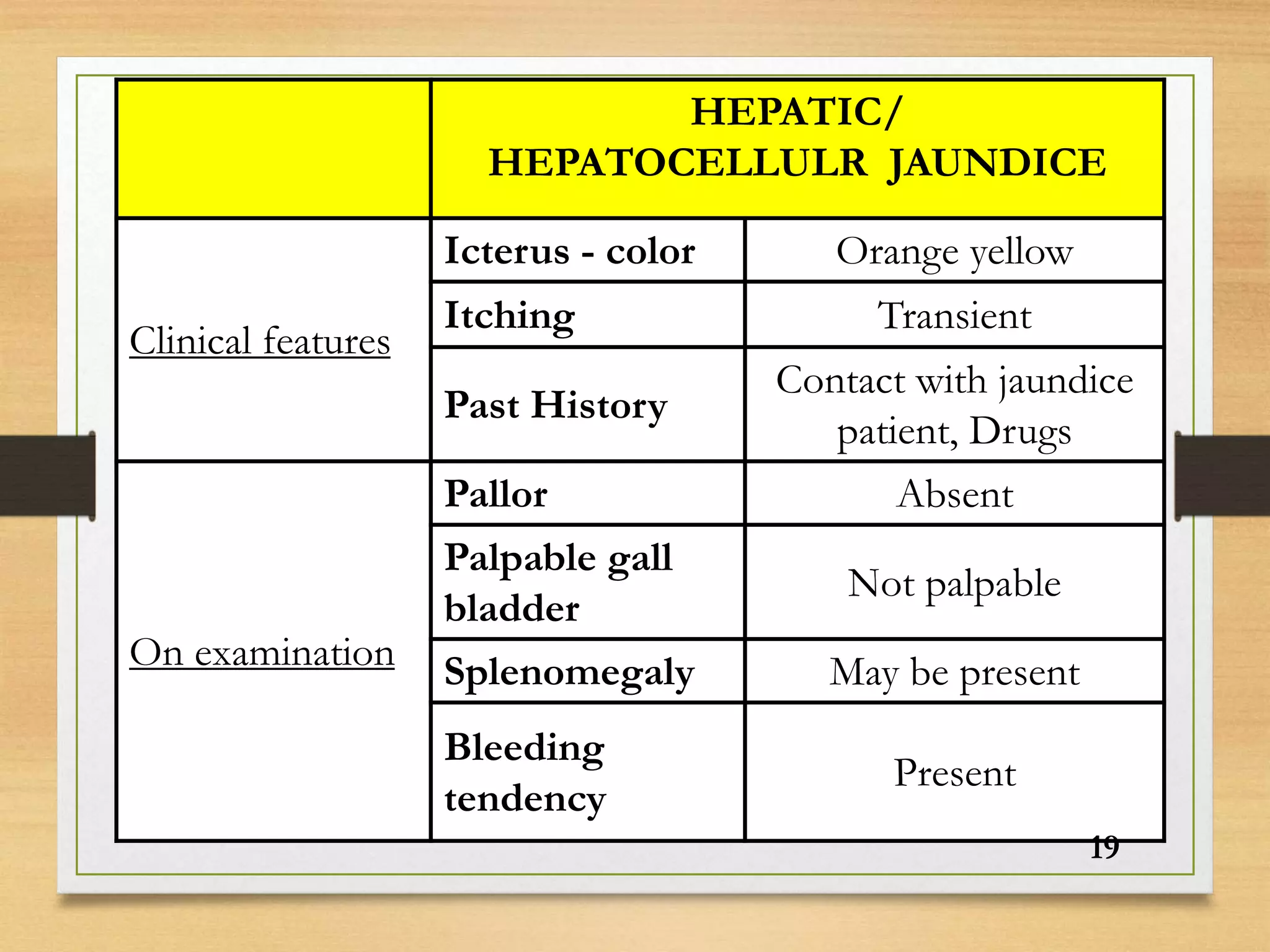
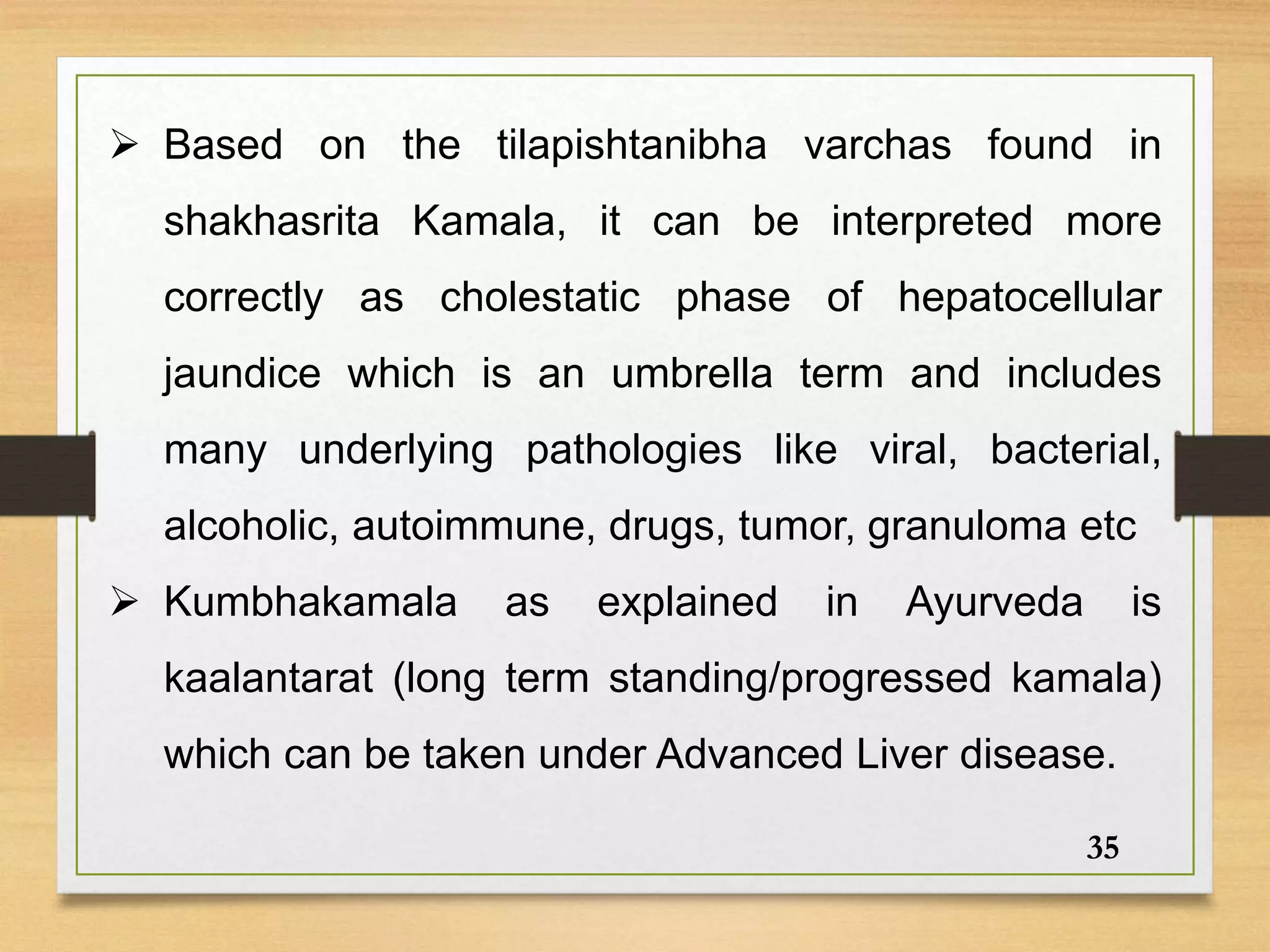
2. How LFT results can help distinguish between pre-hepatic, hepatic, and post-hepatic jaundice. Pre-hepatic jaundice shows elevated unconjugated bilirubin while hepatic jaundice shows elevated conjugated bilirubin and liver enzymes.
3. How correlating LFTs with clinical symptoms can aid in diagnosing koshtashakhas