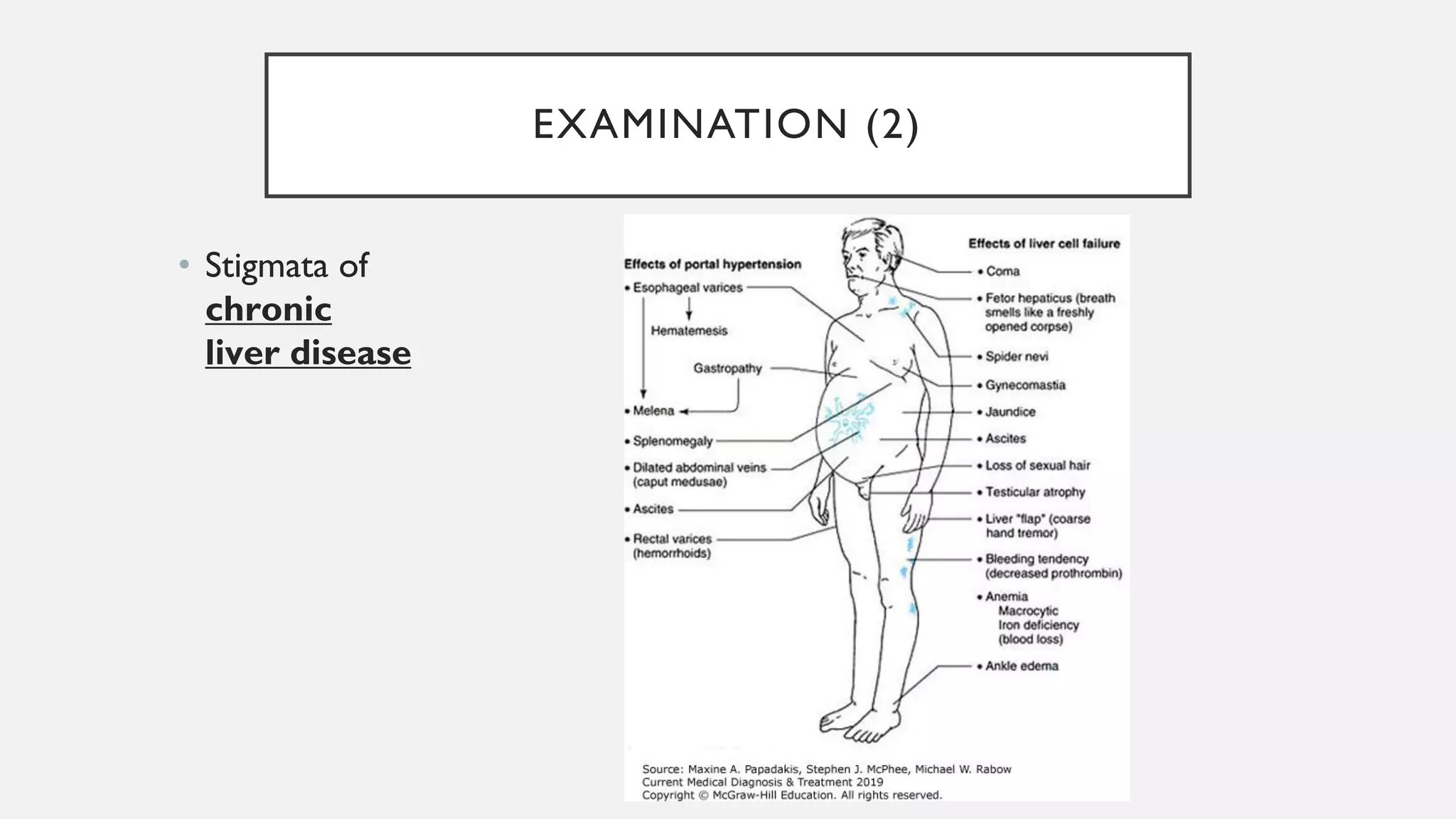
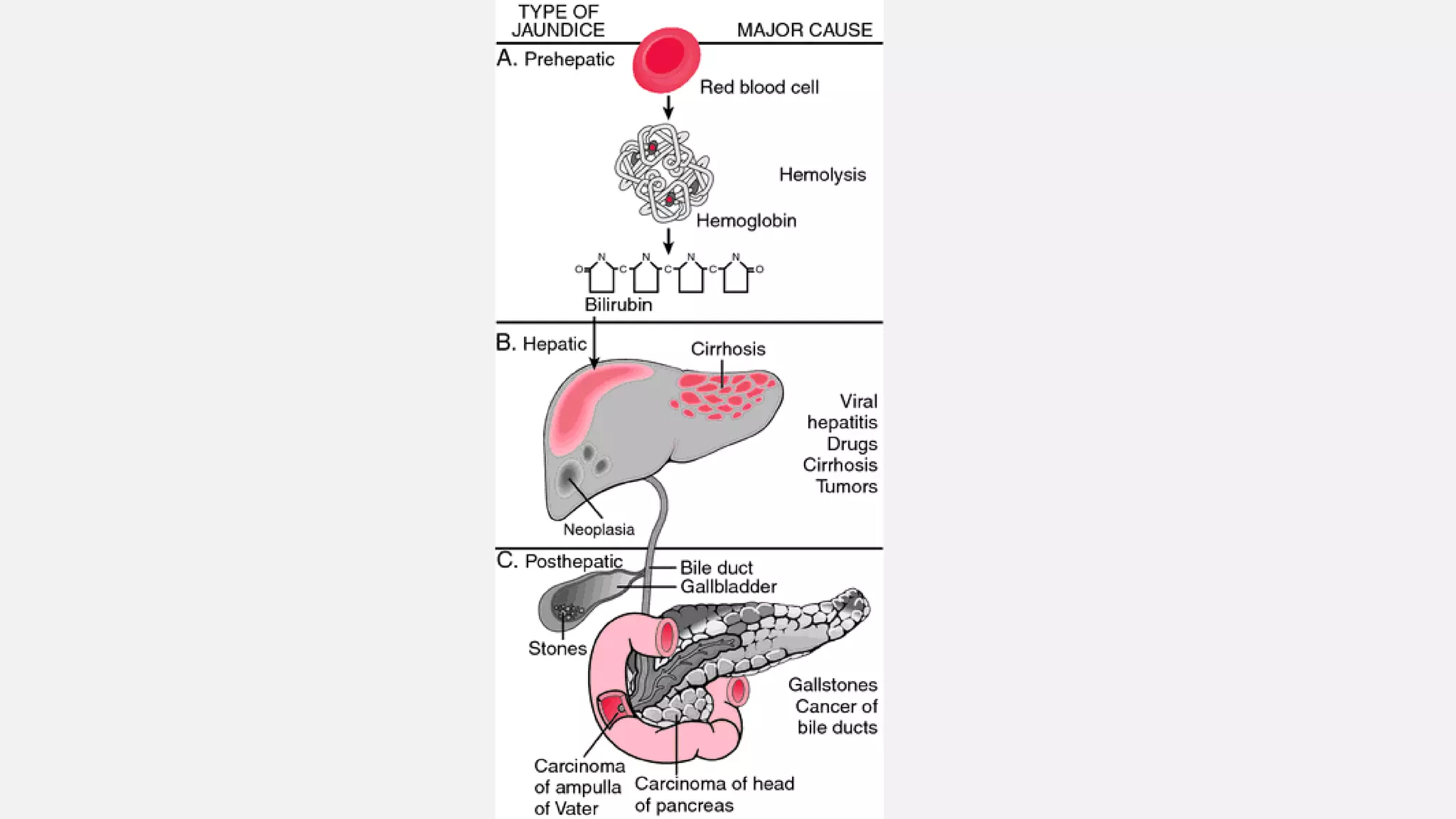
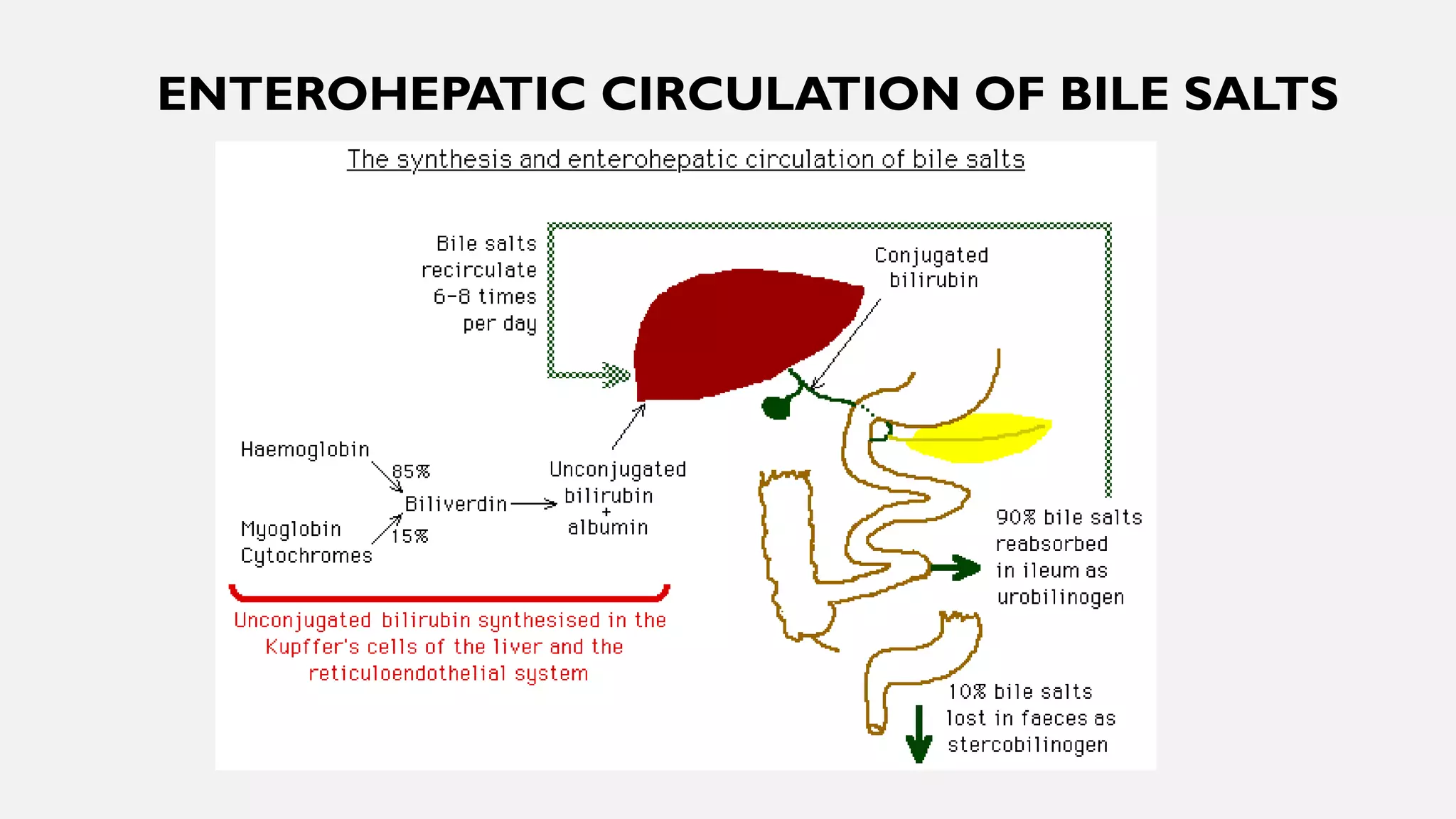
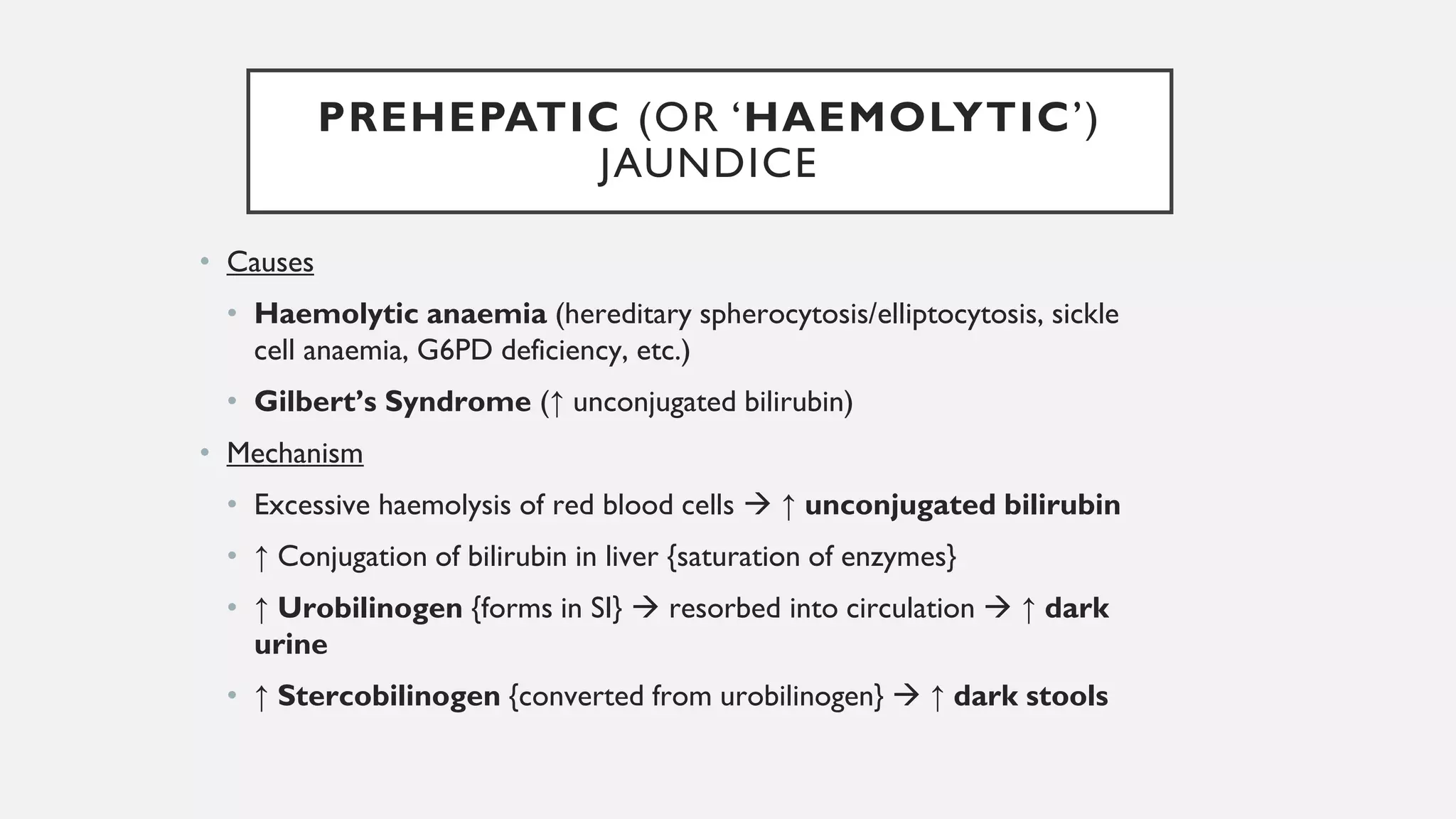
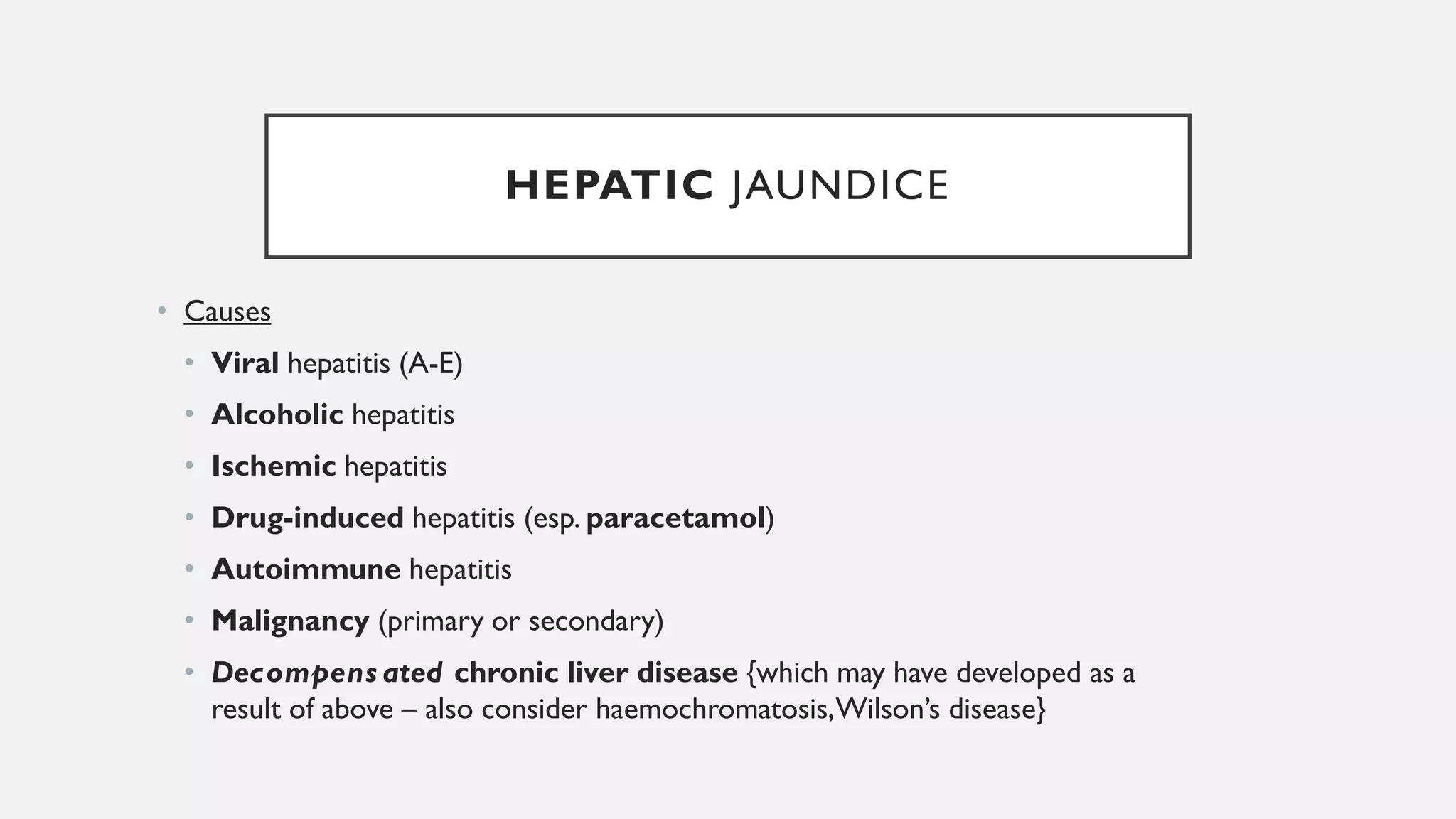
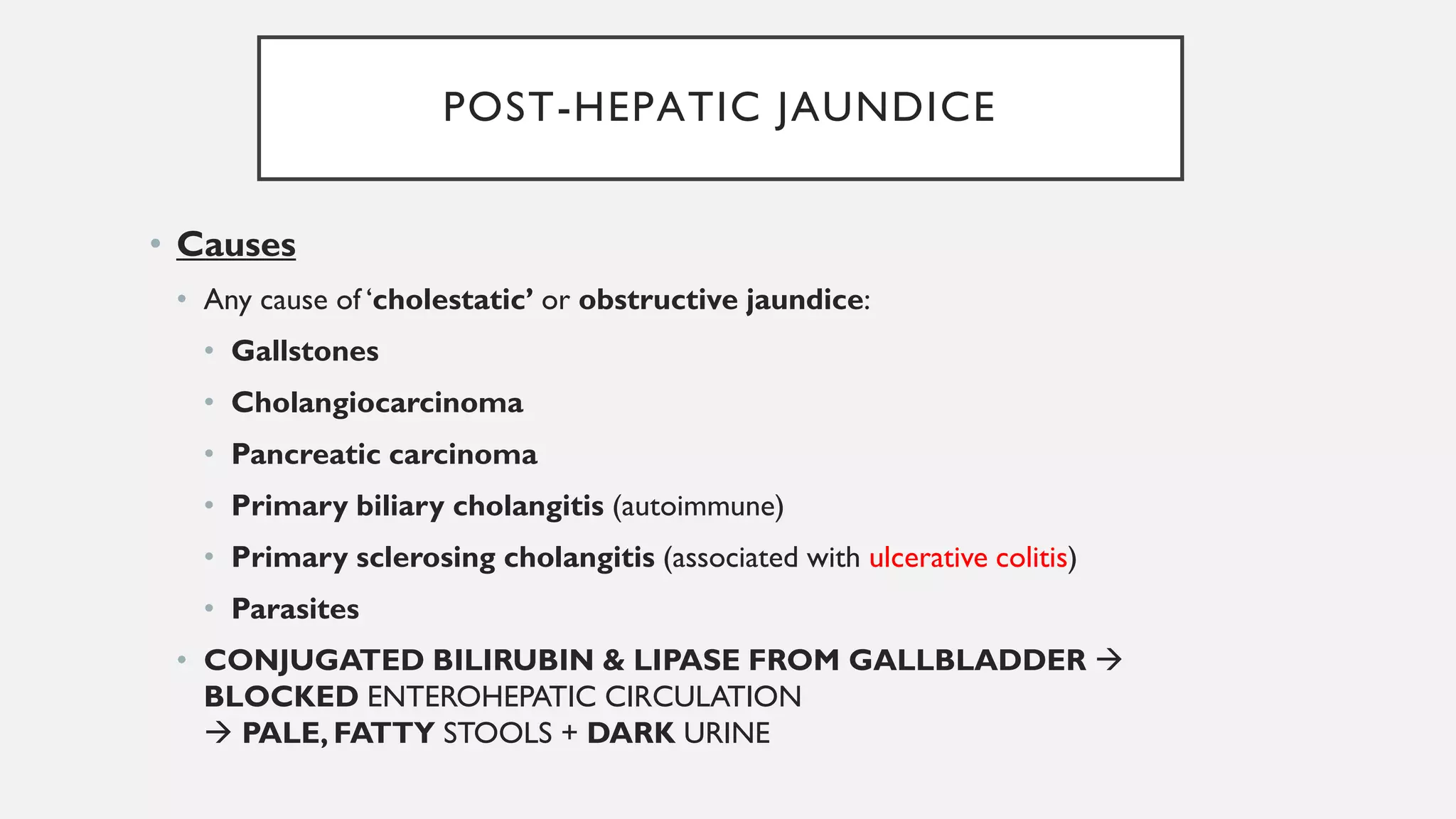
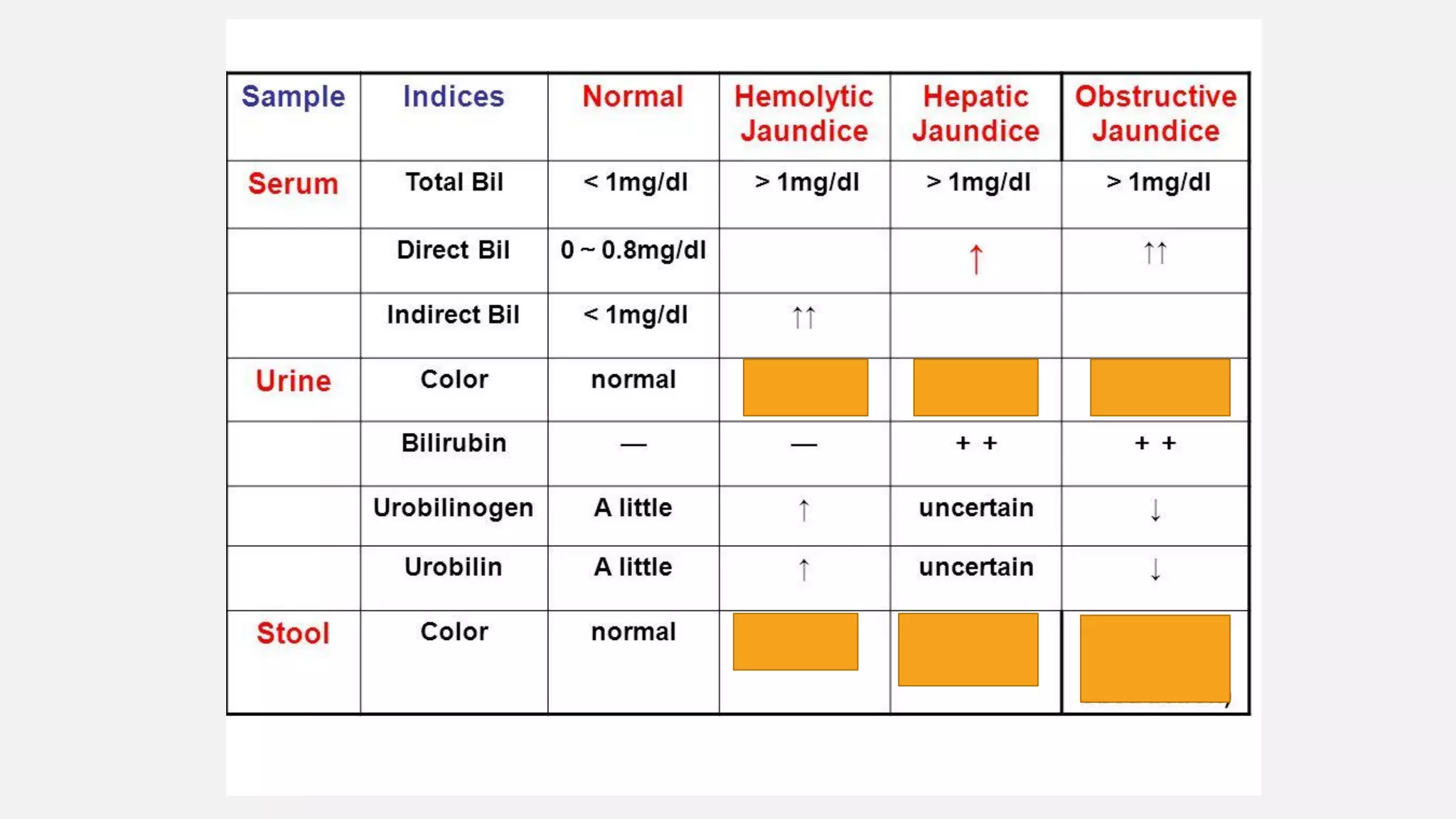
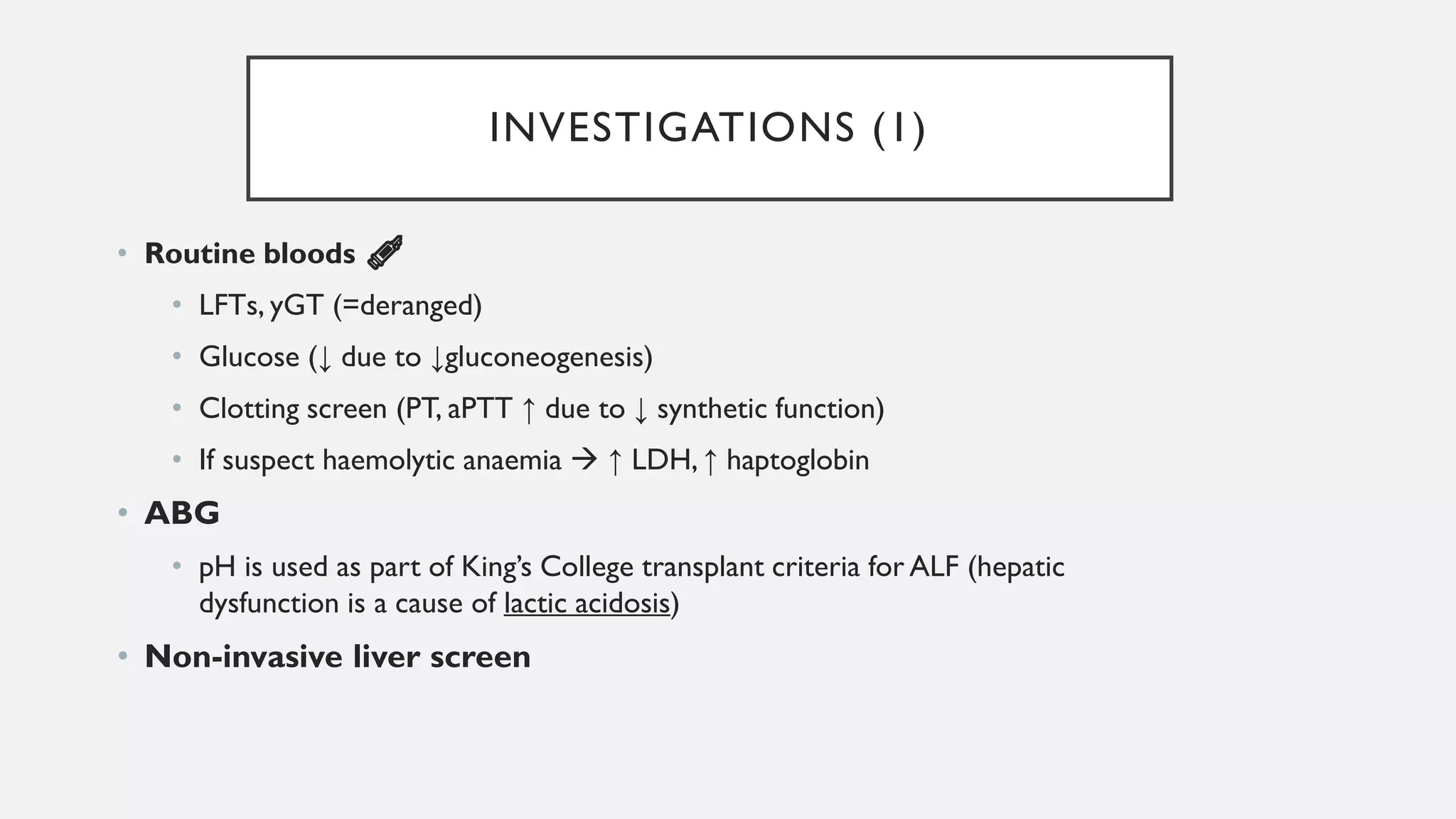
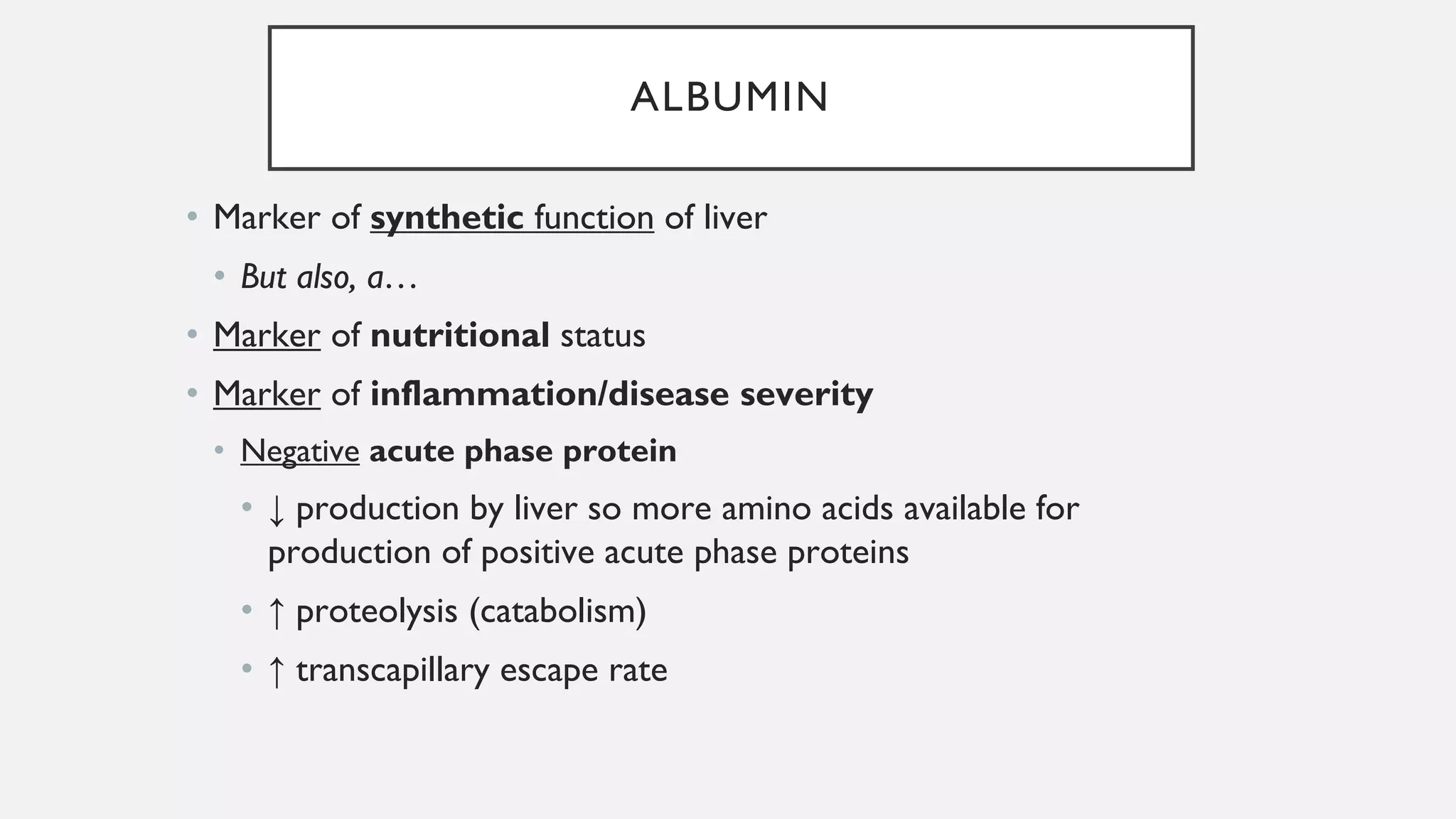
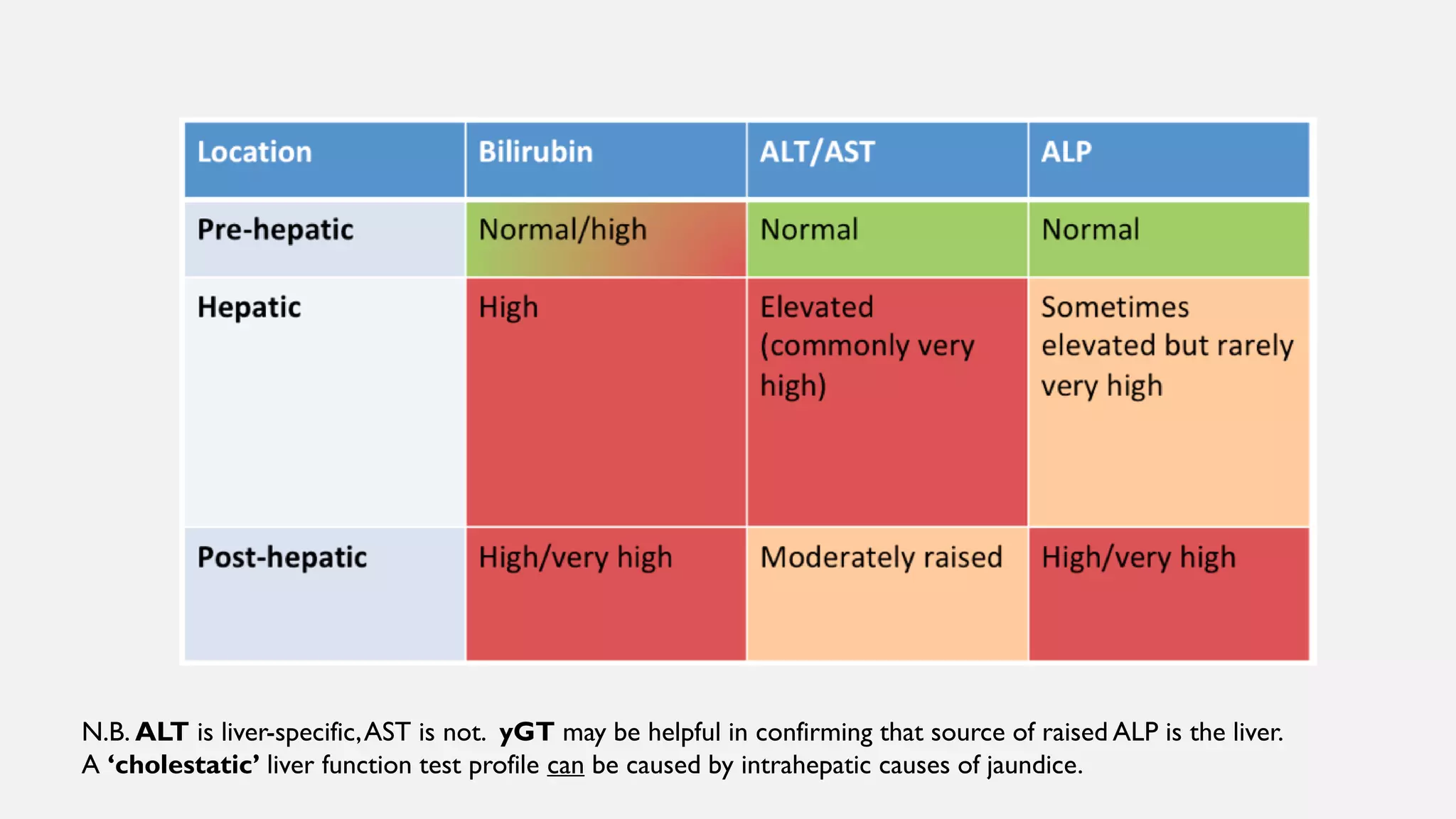
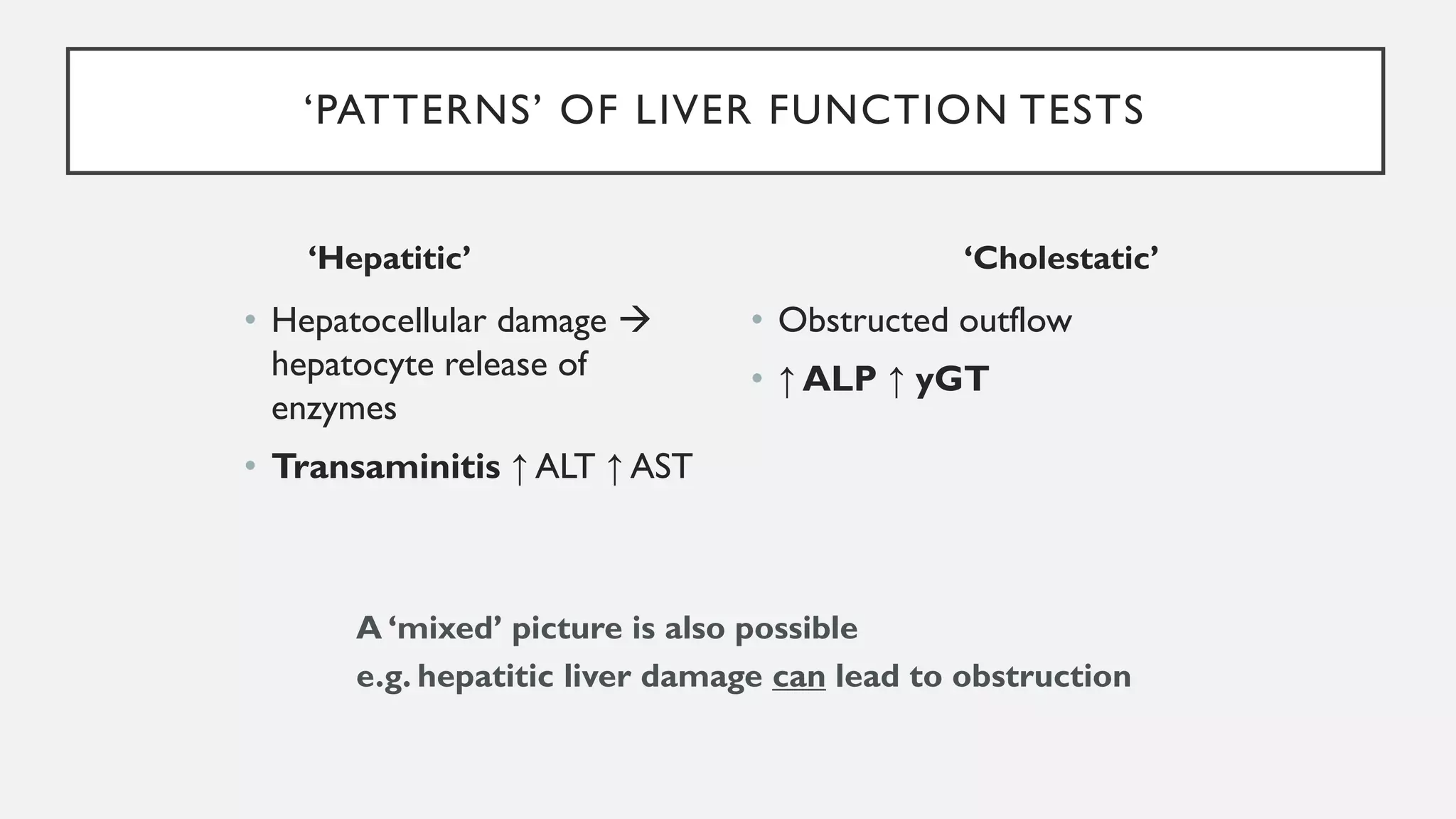
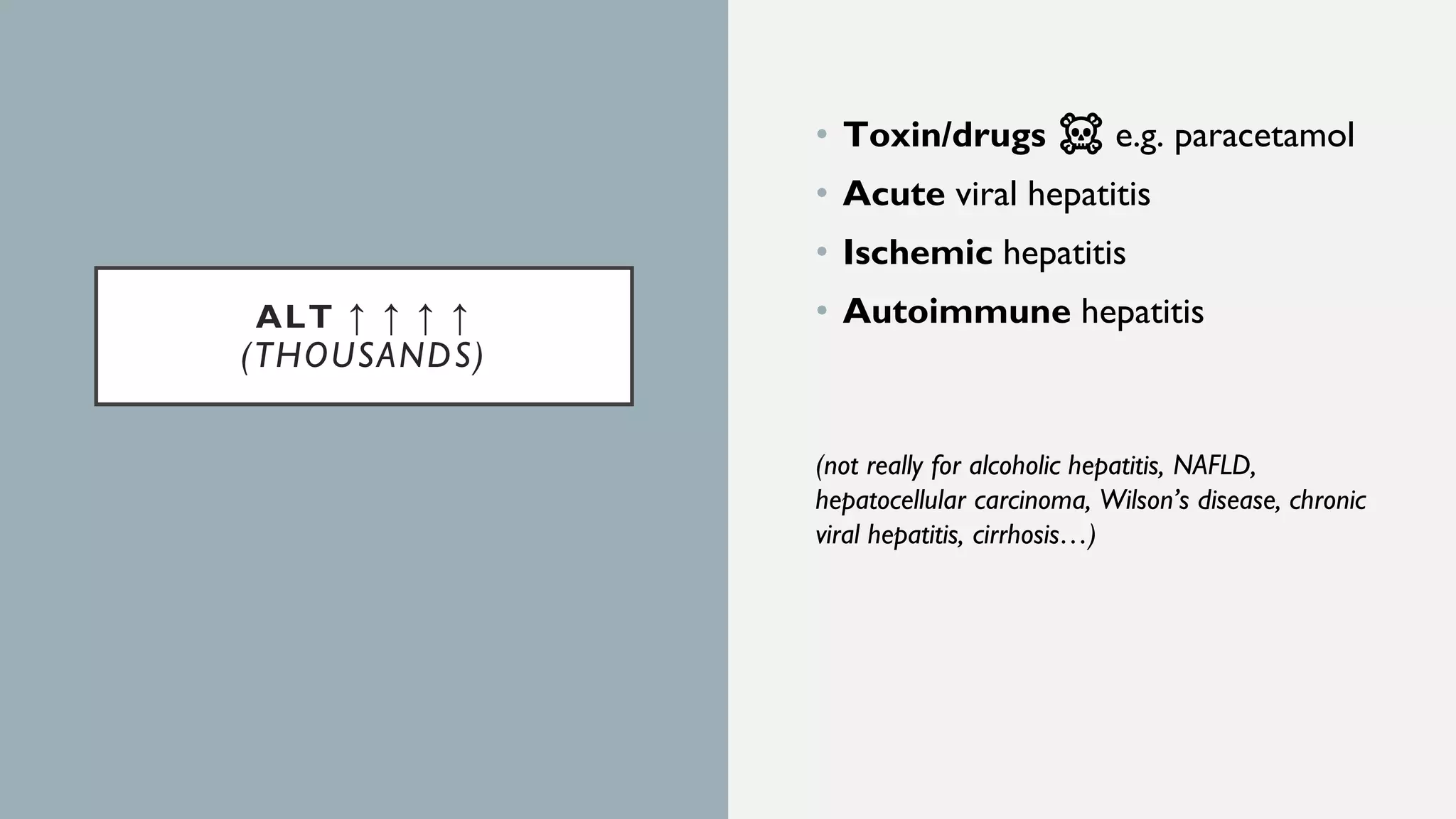
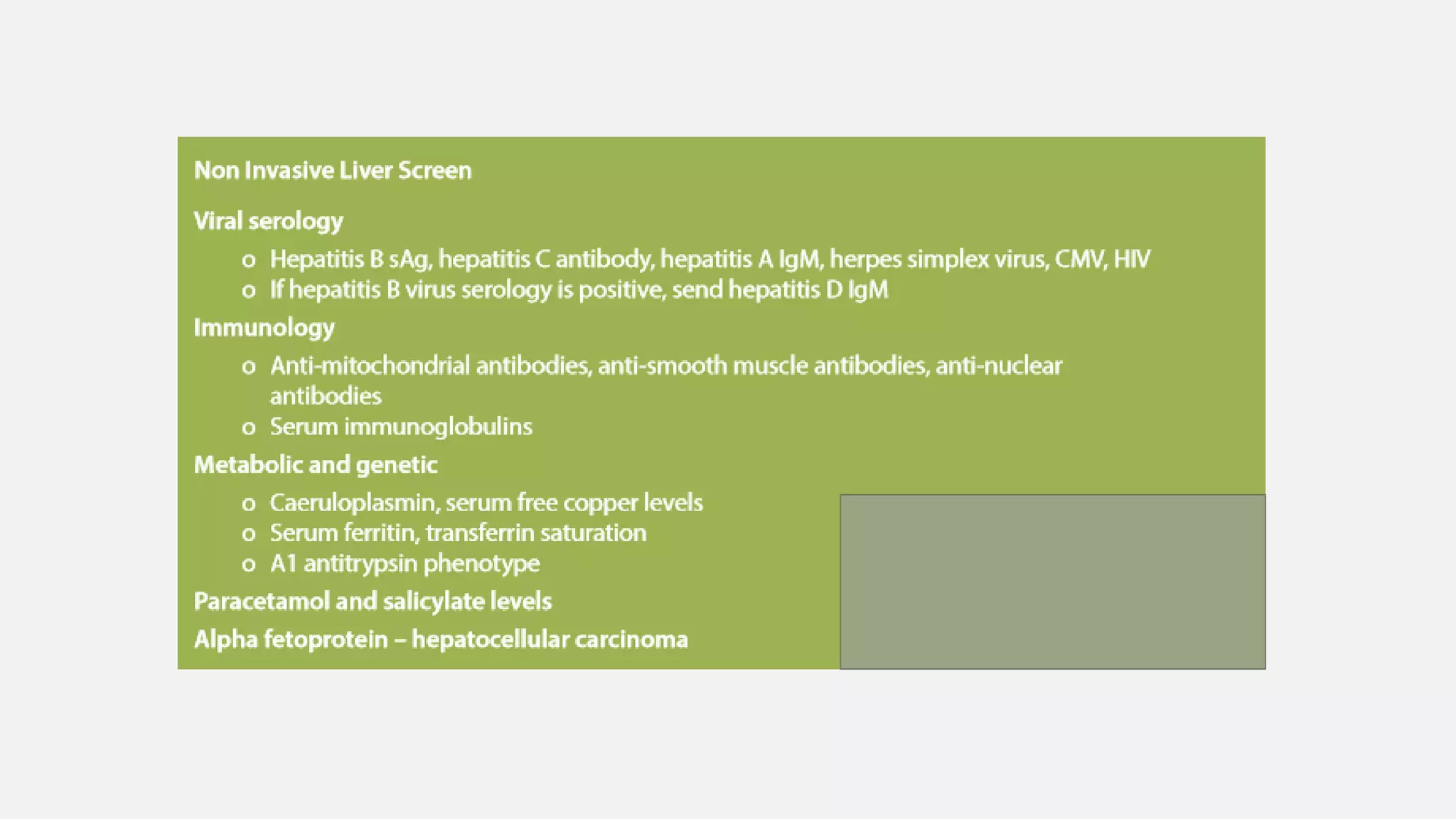
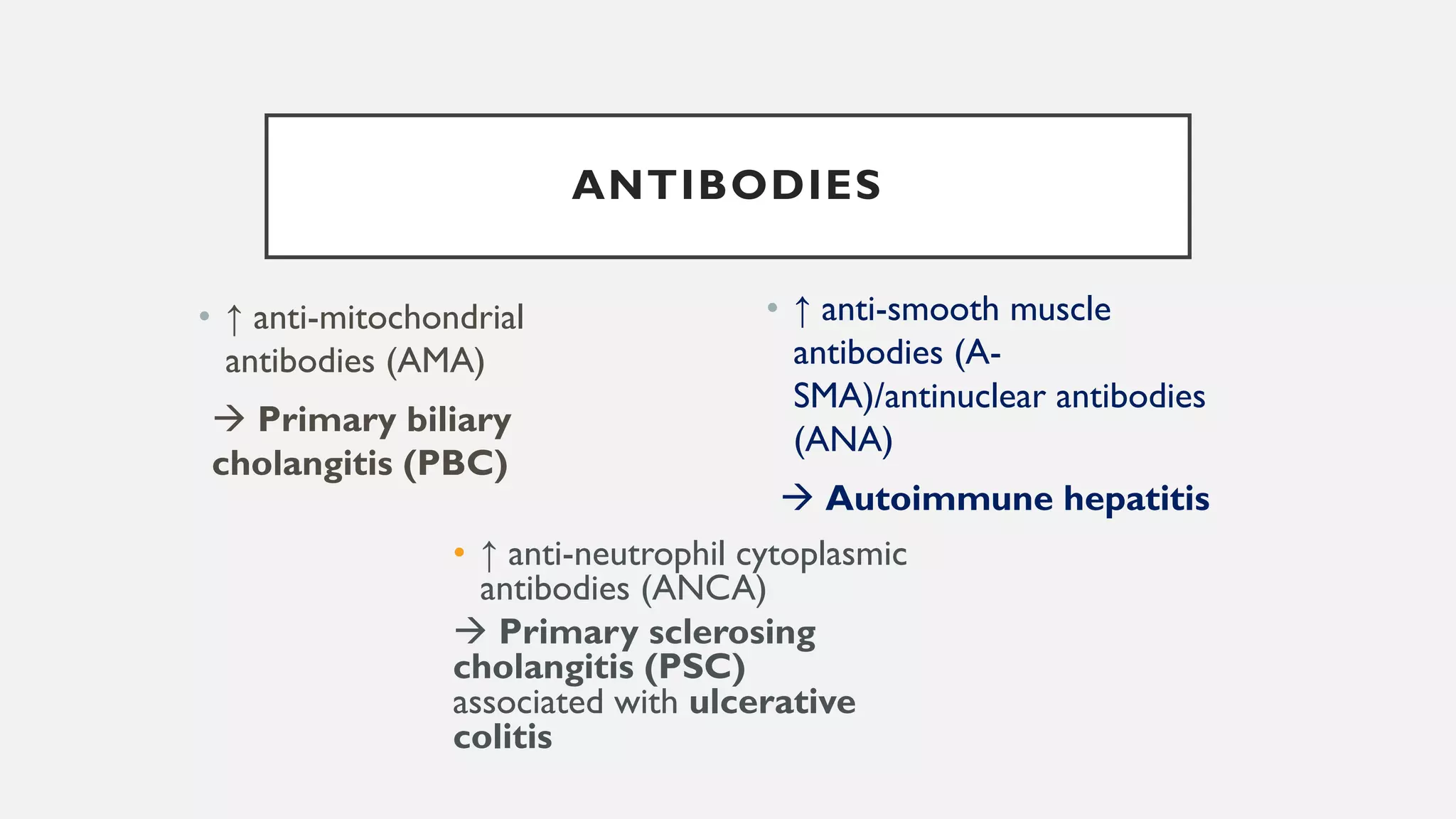
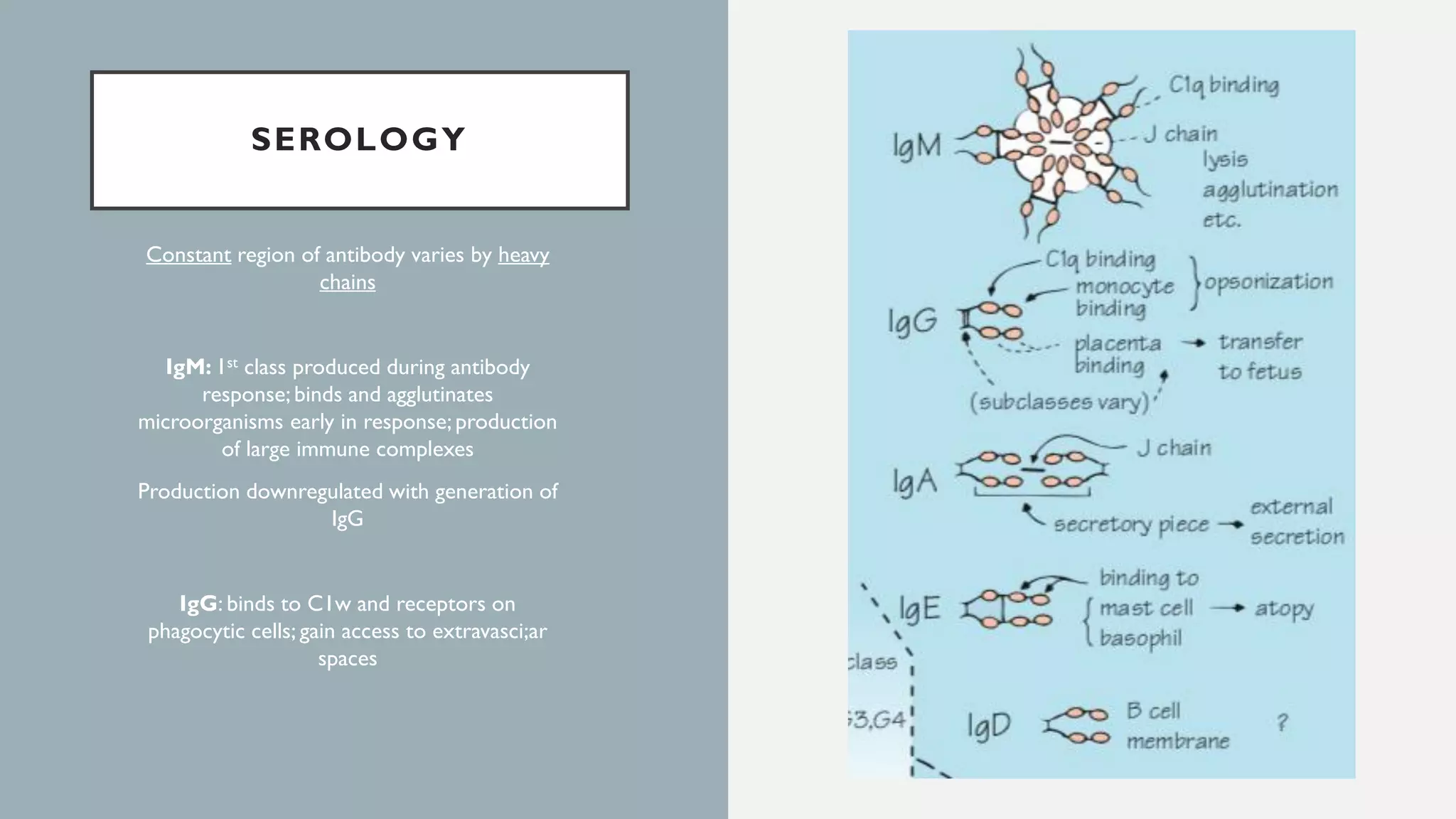
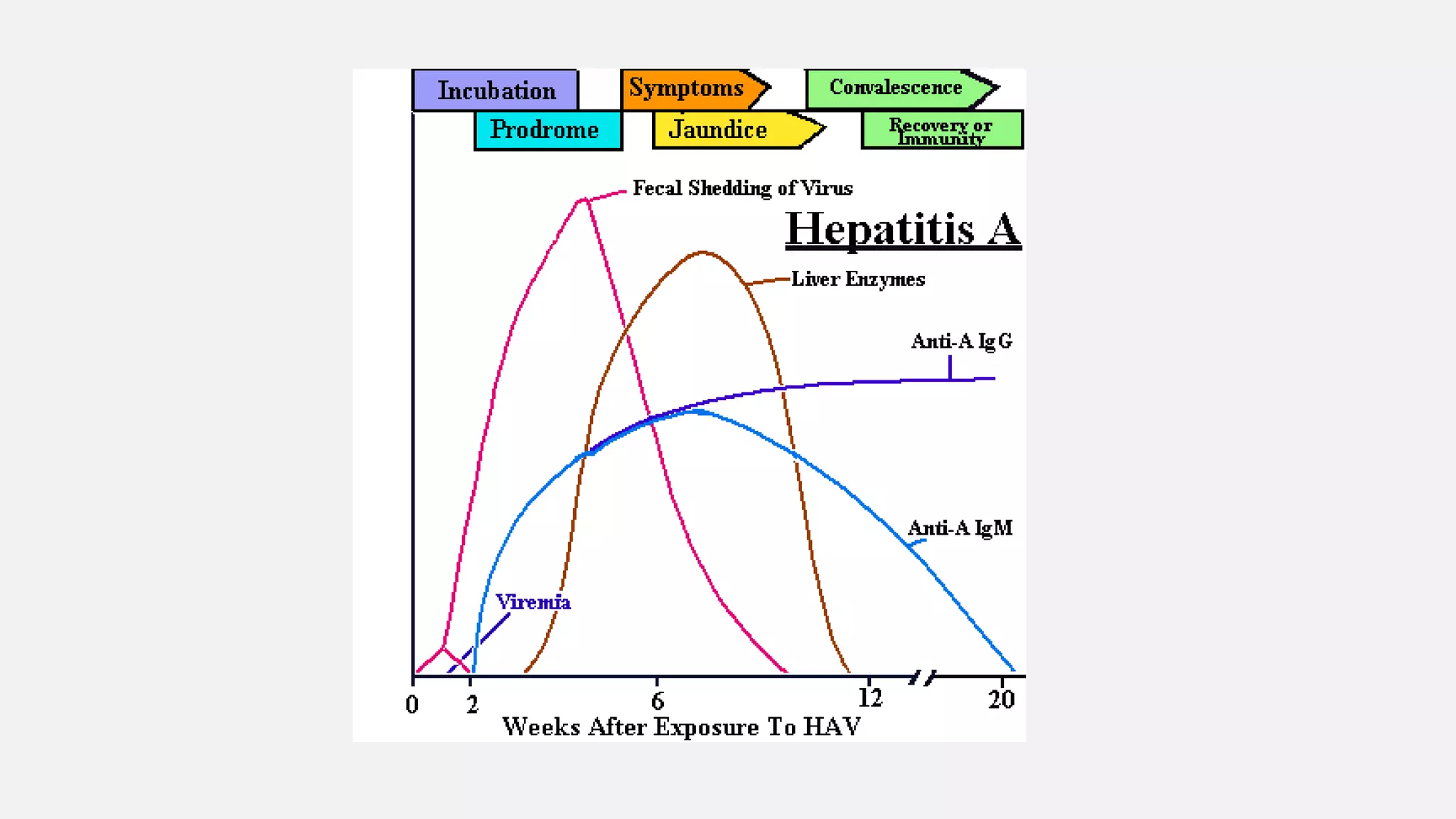
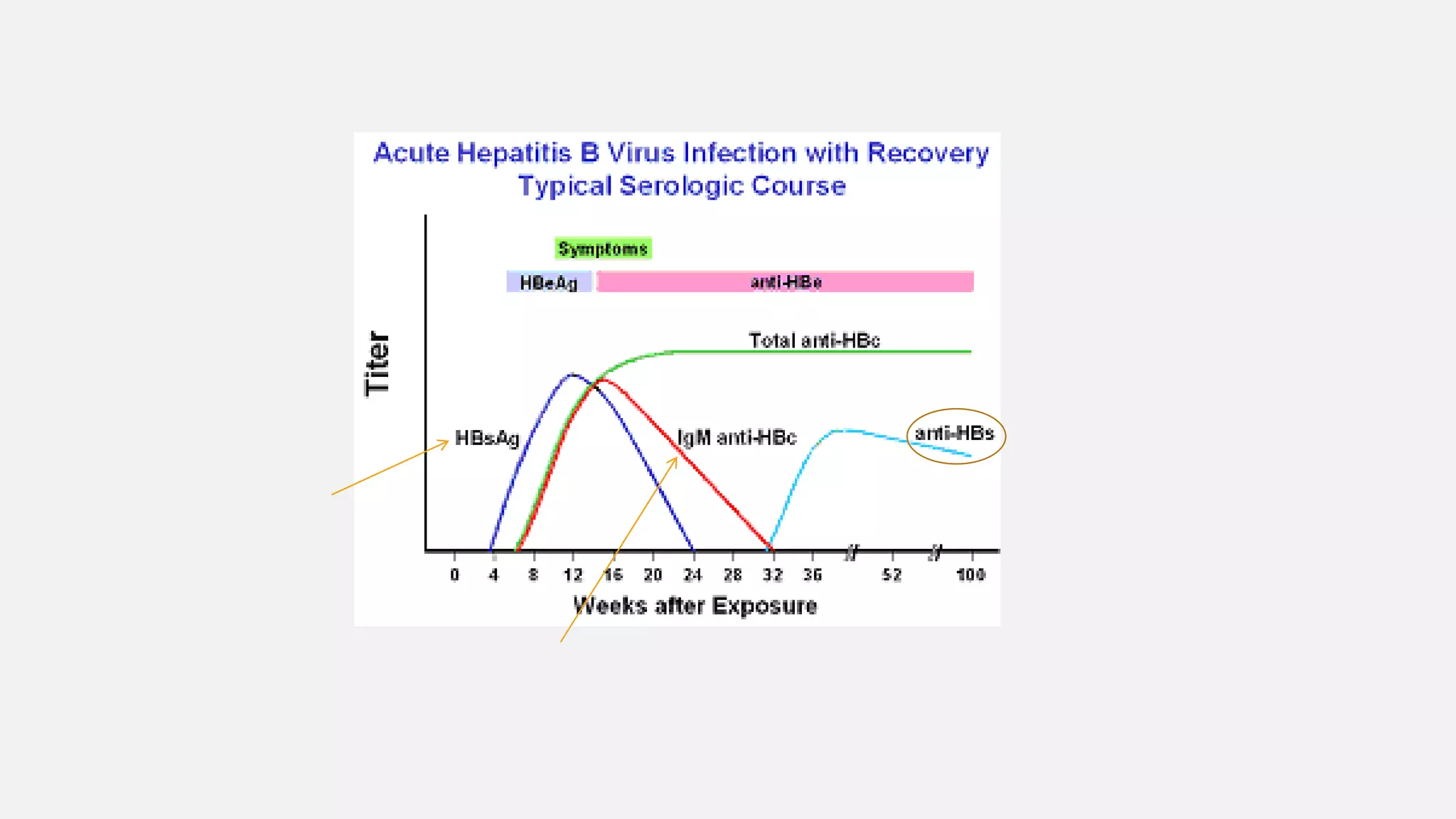
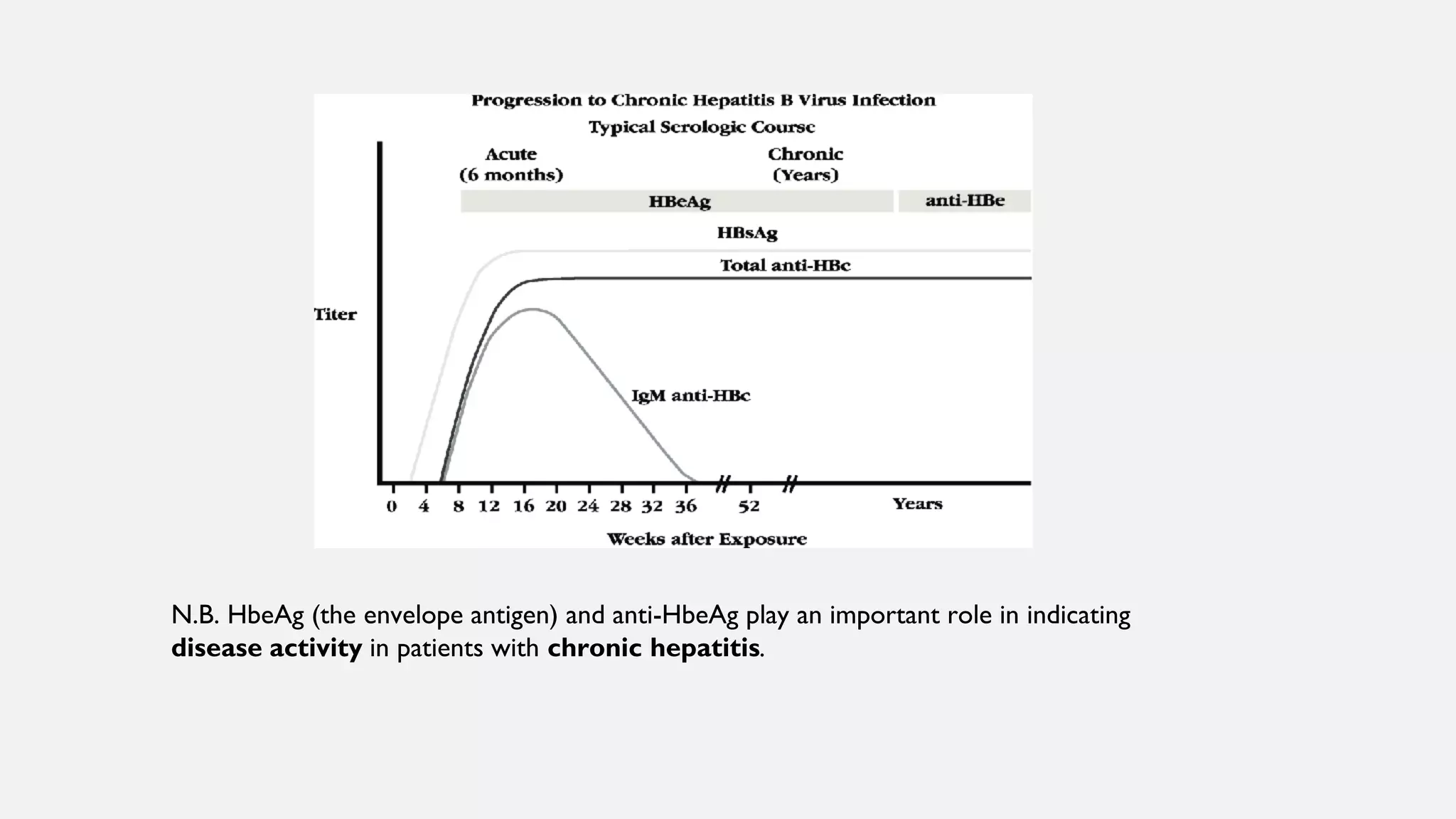
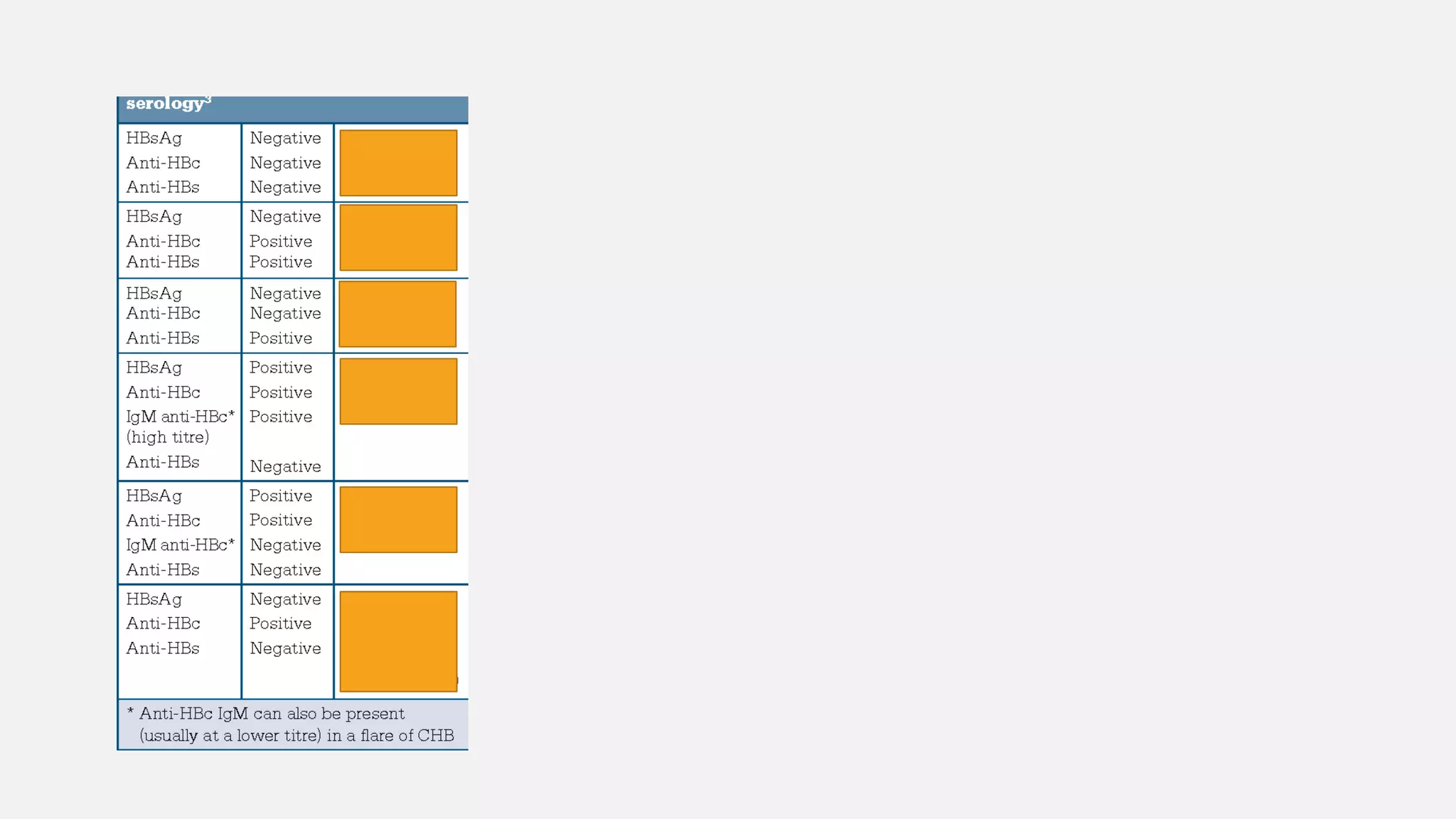
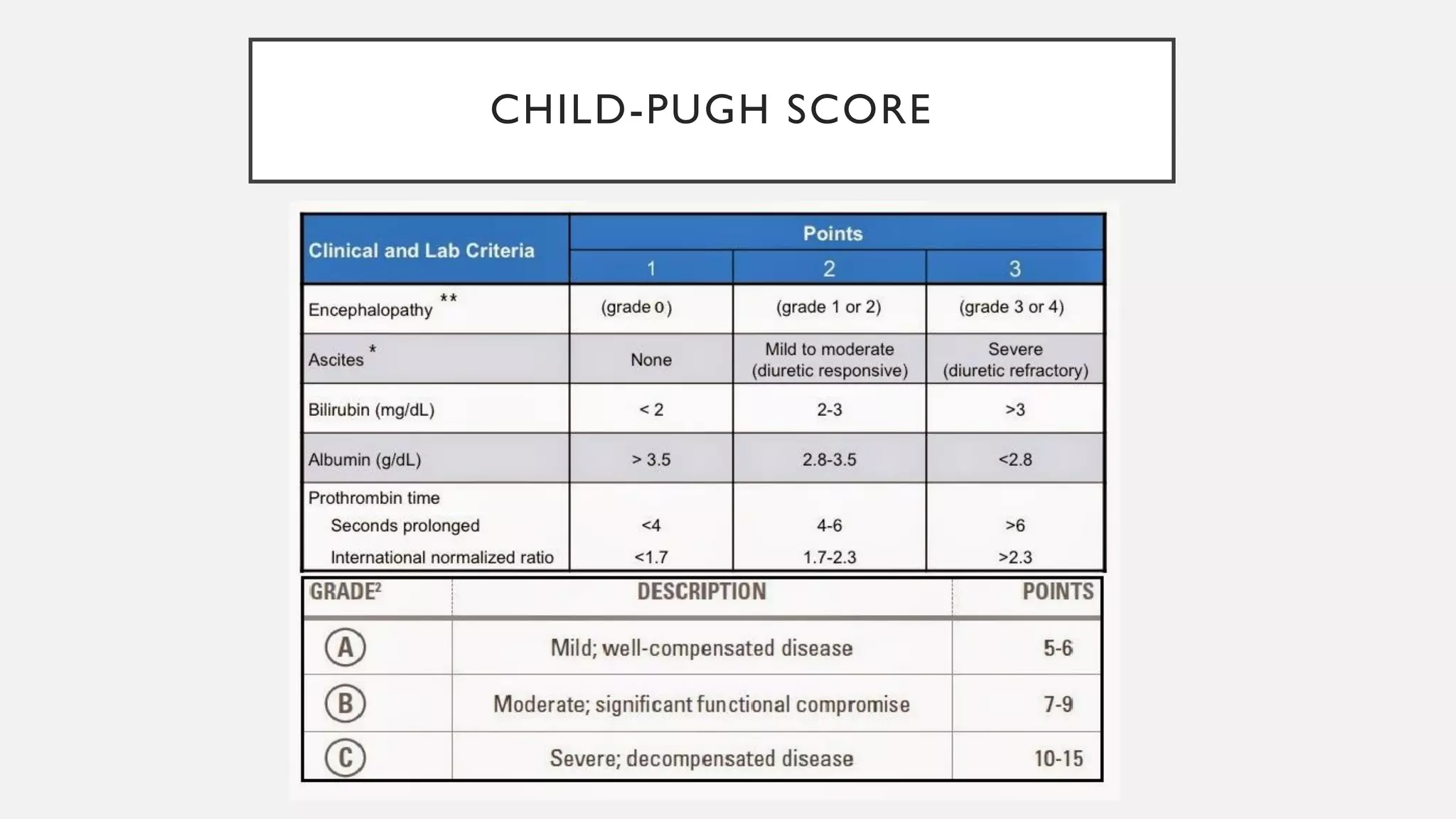
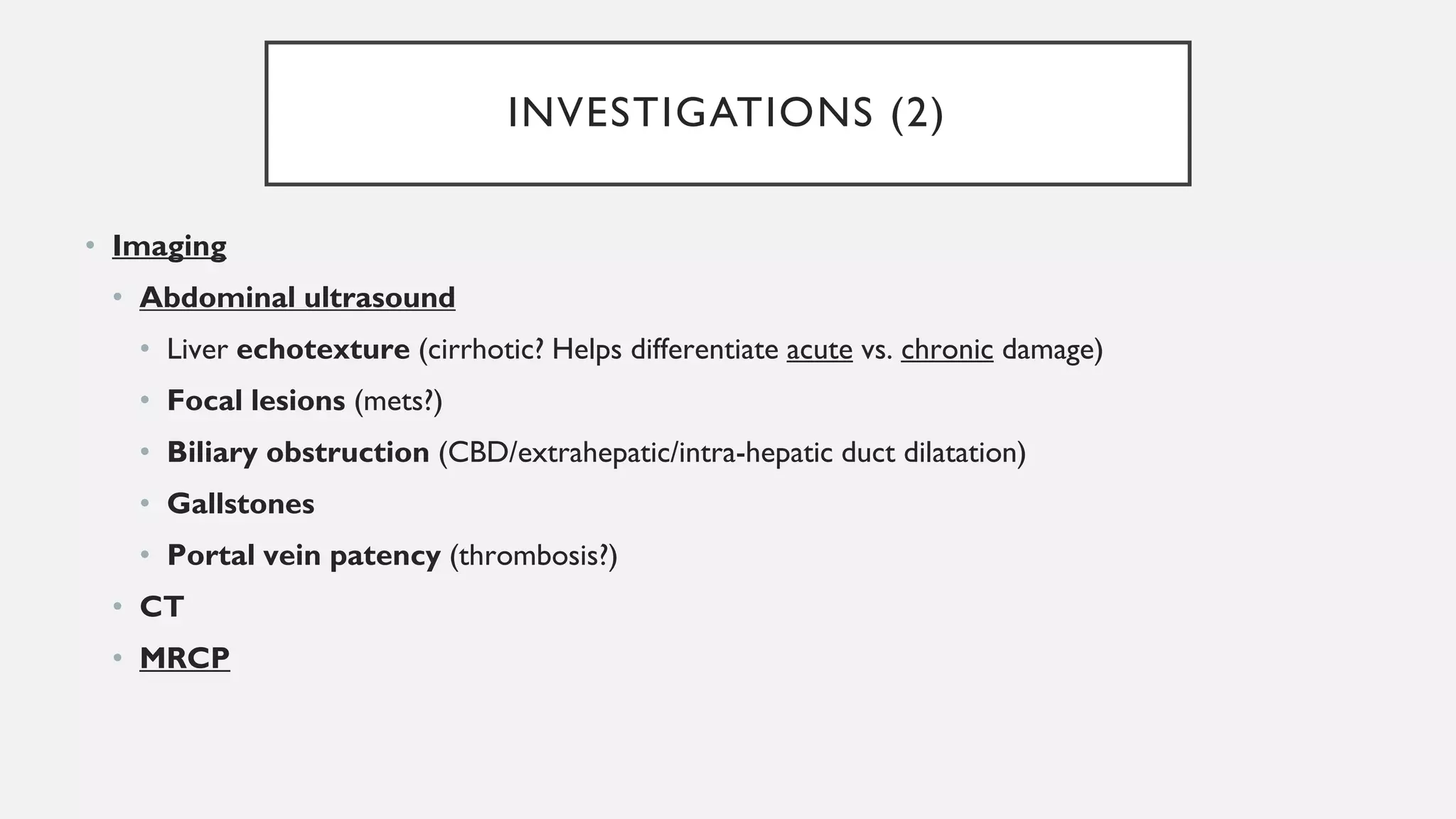
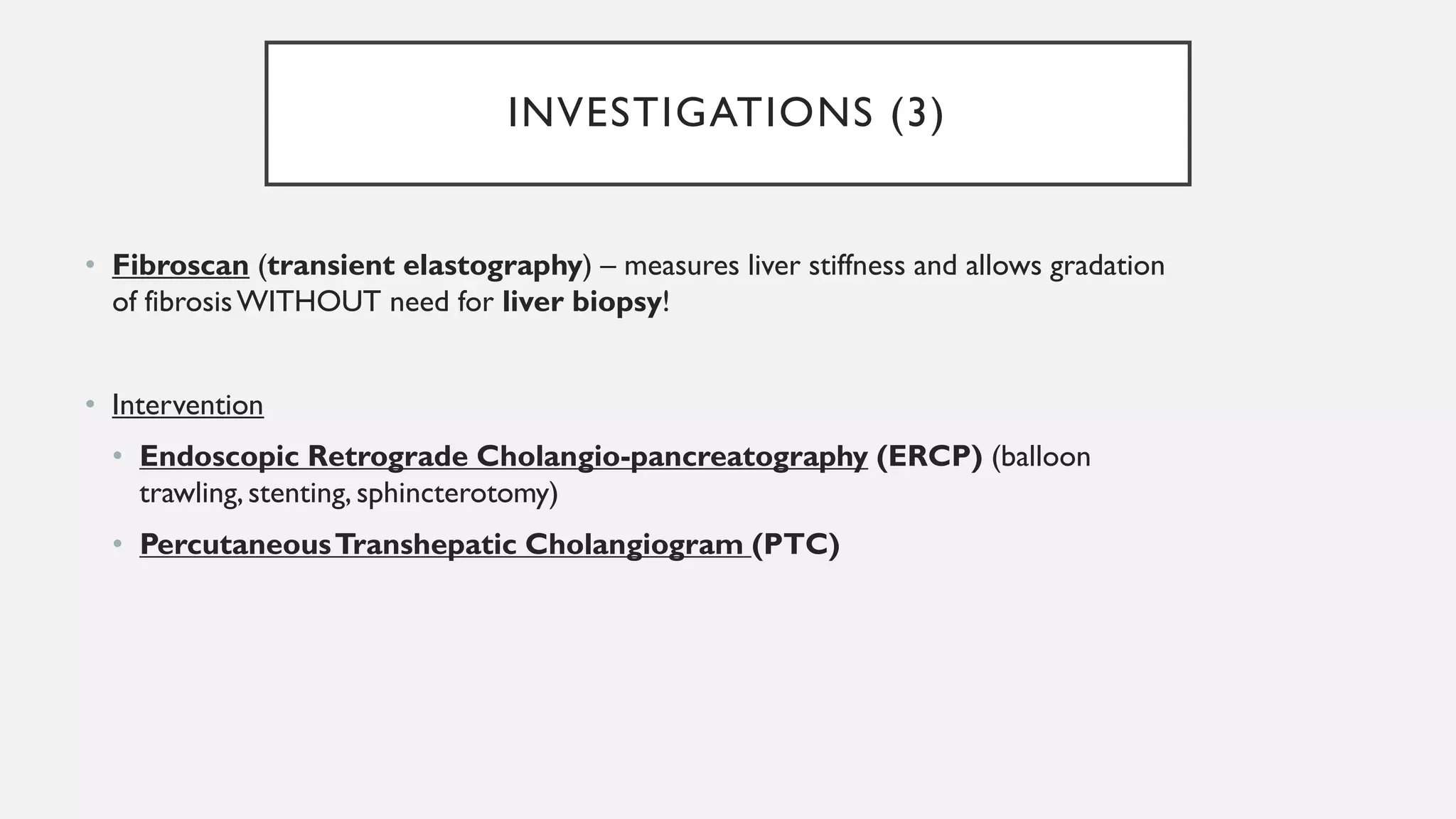
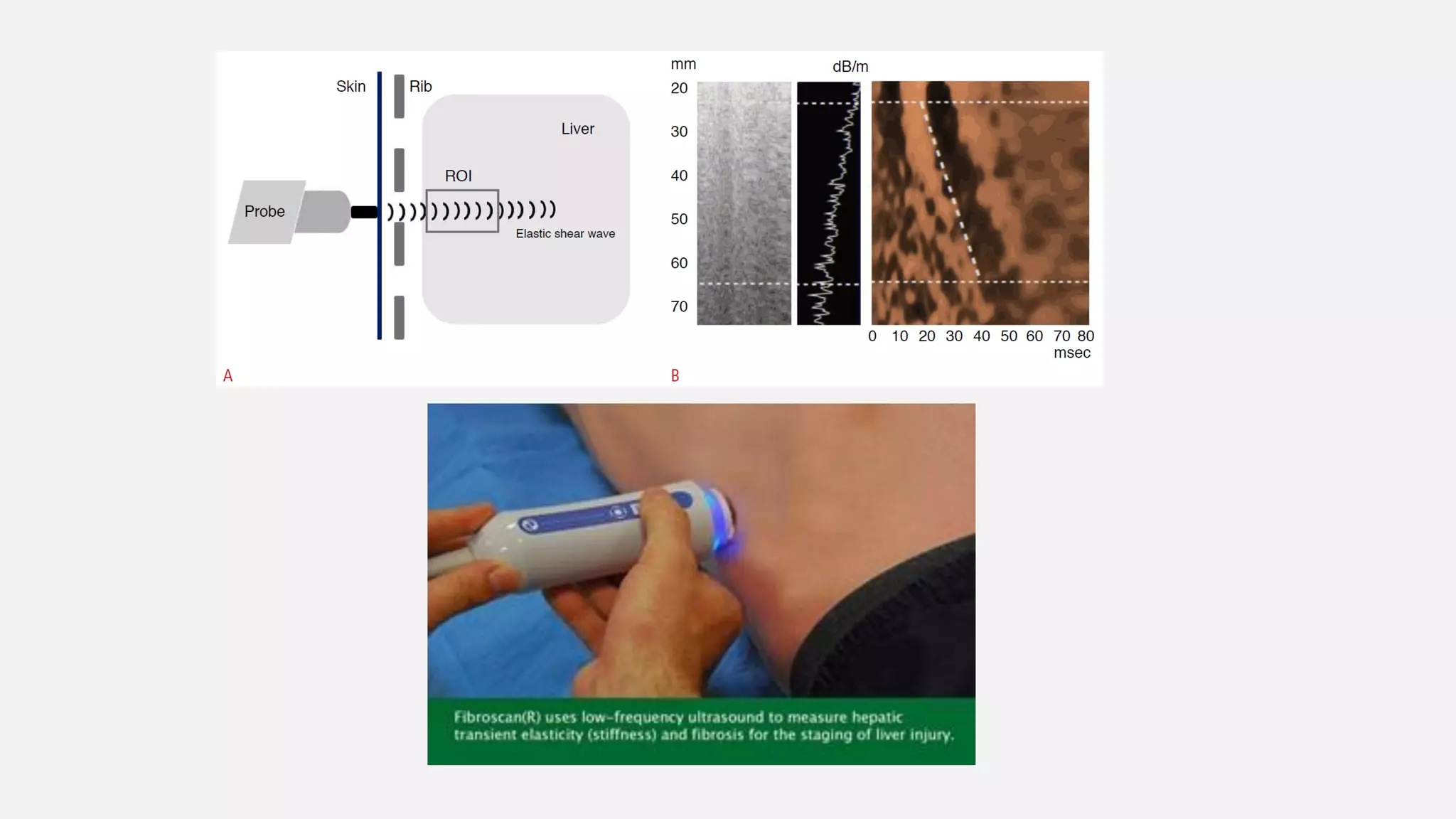
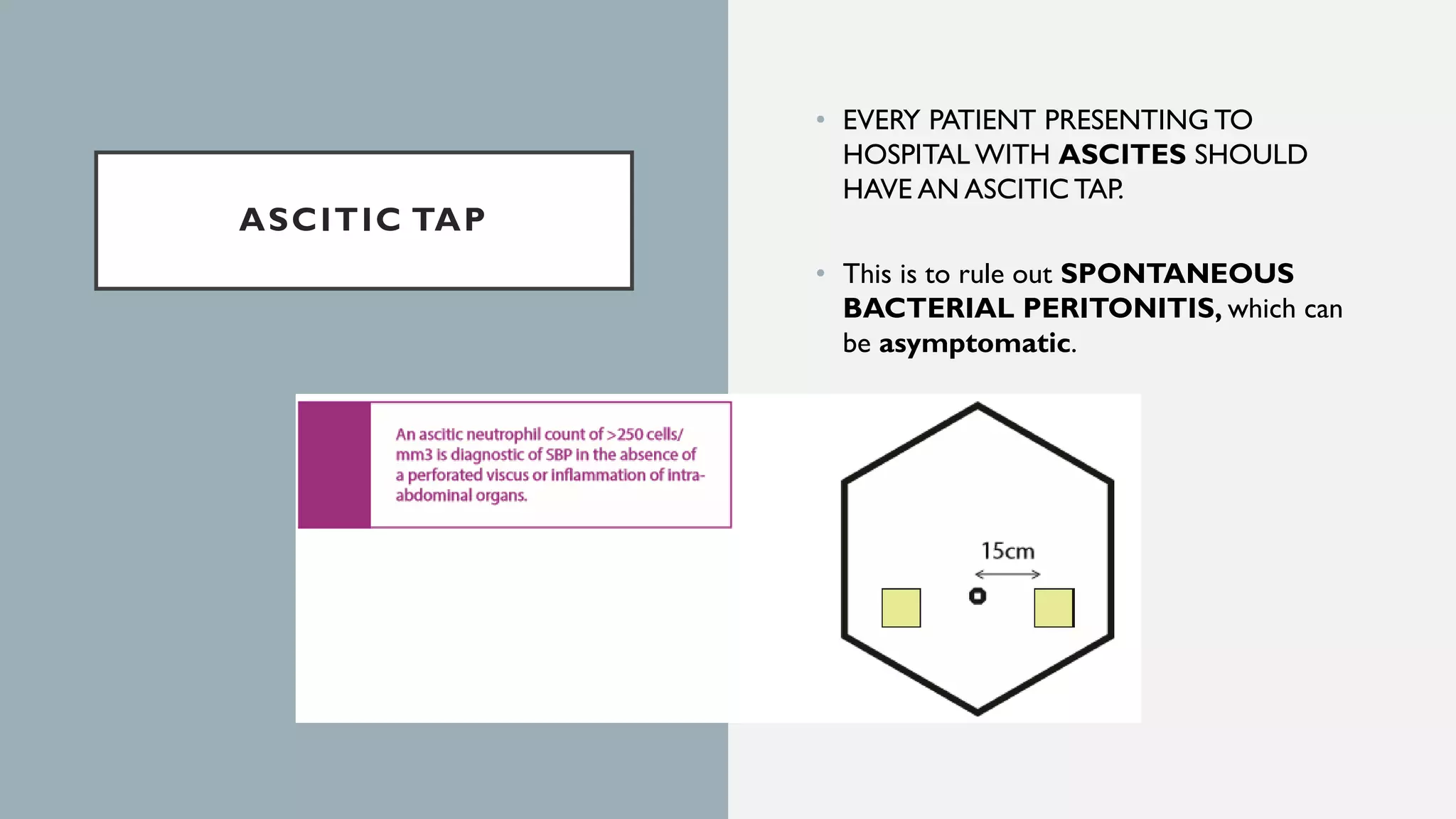
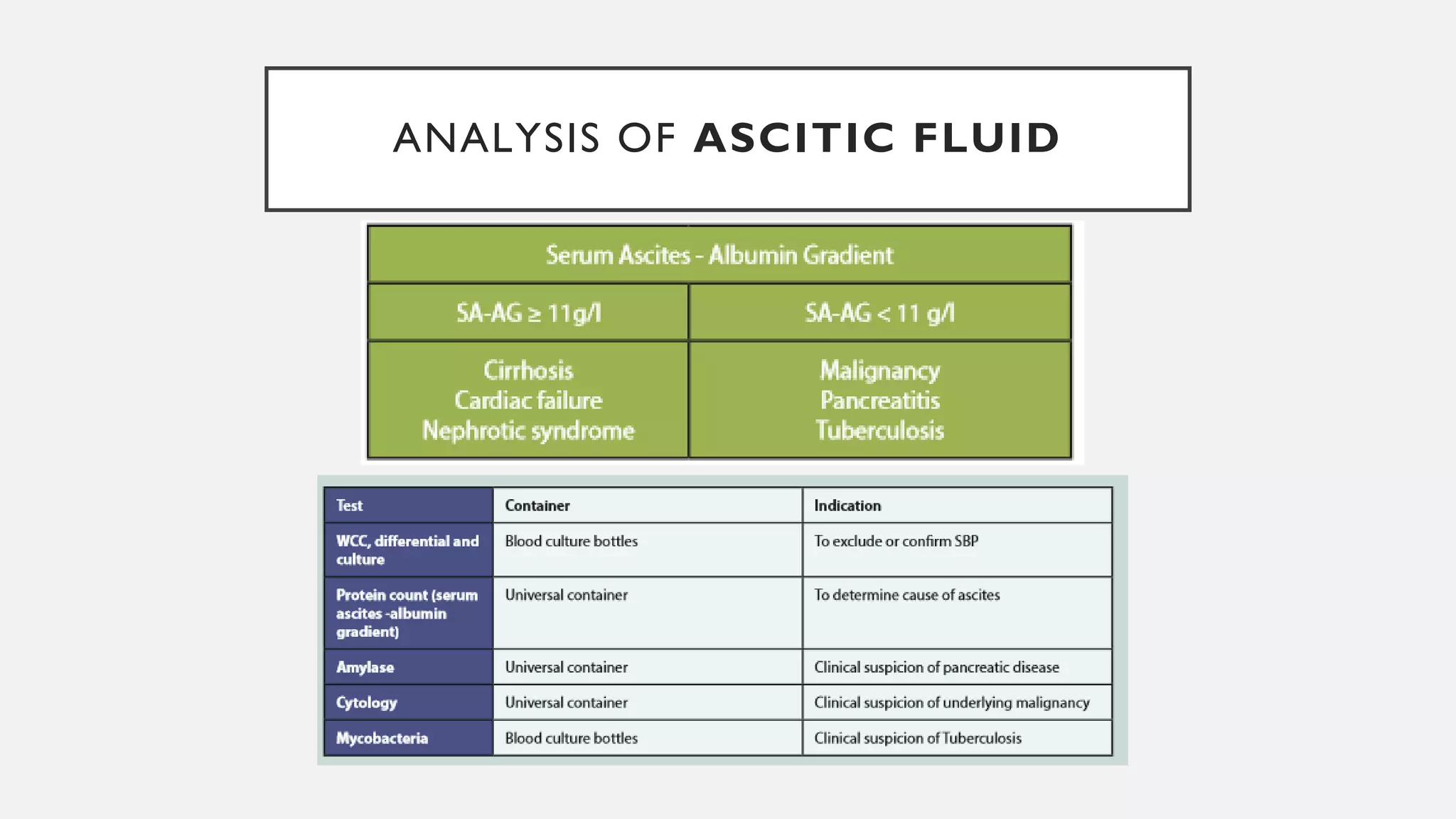
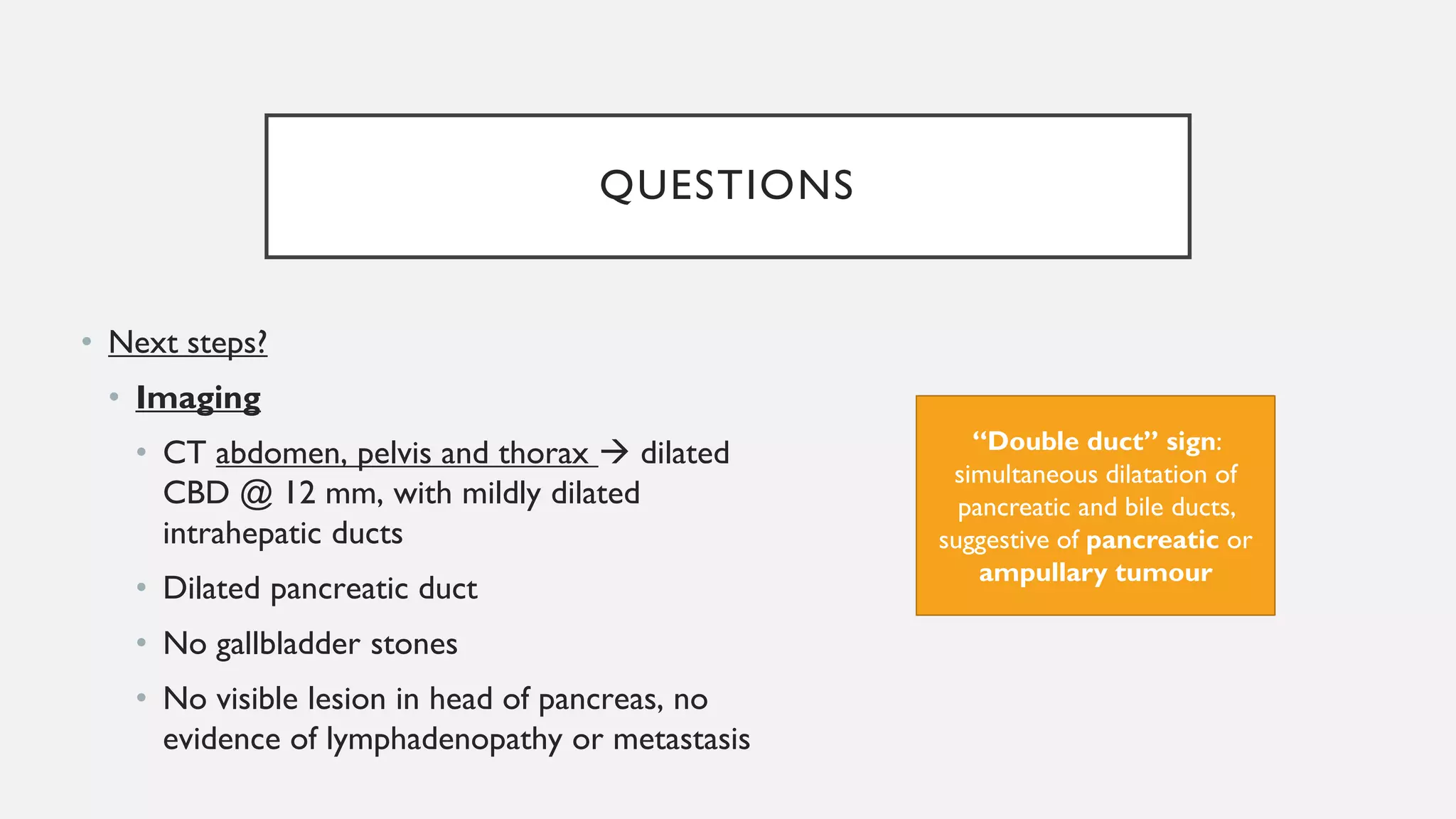
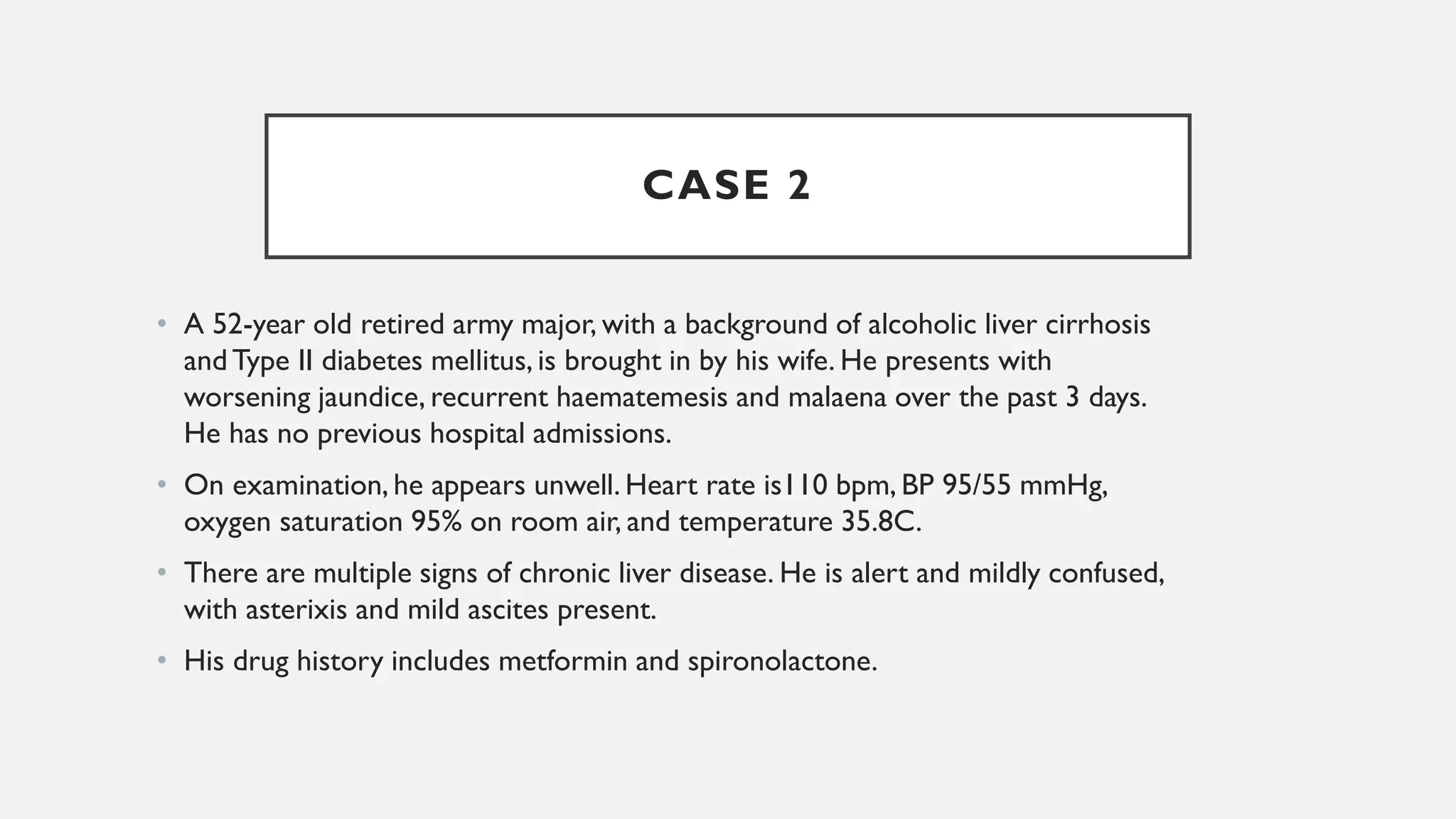
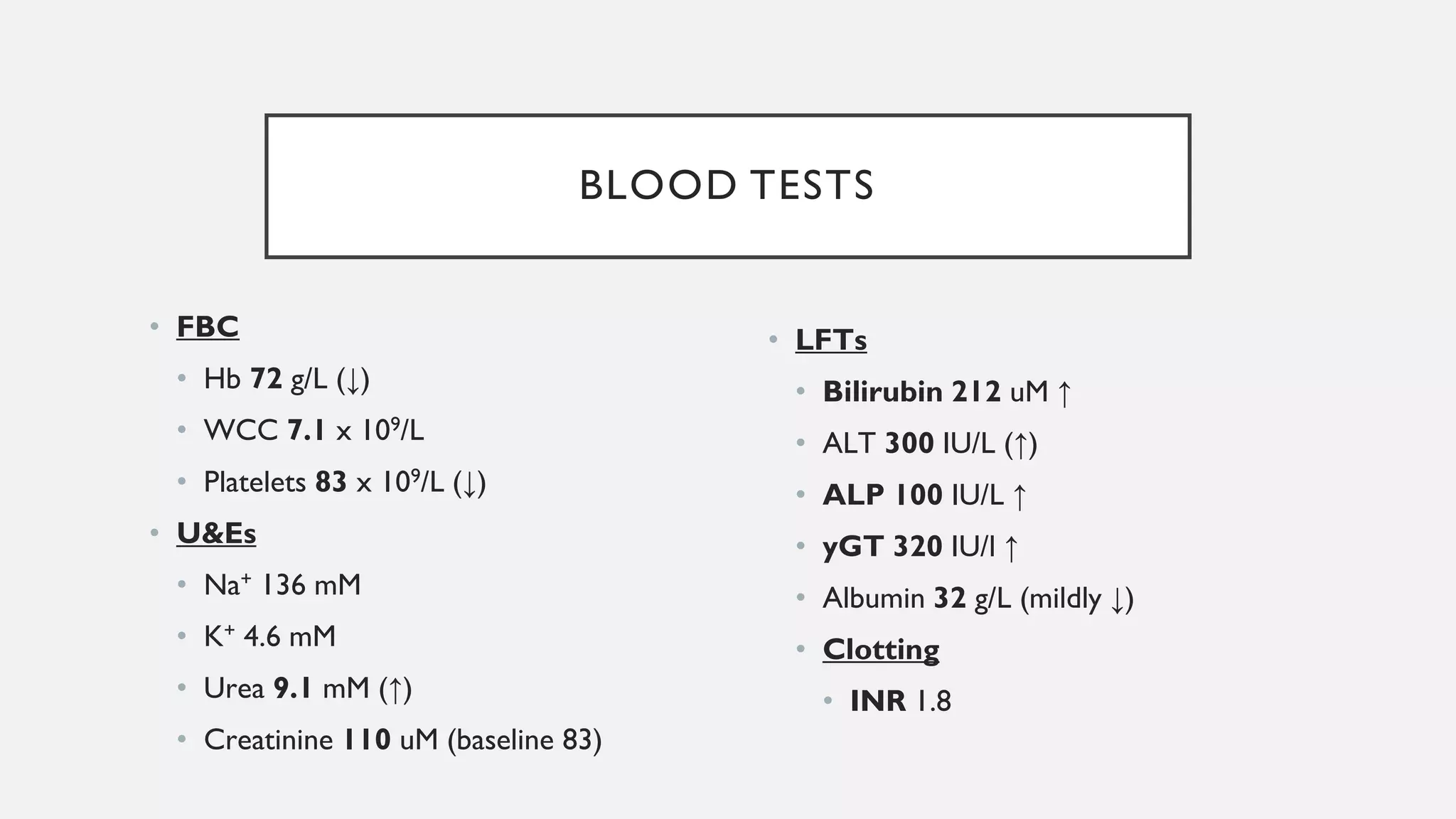
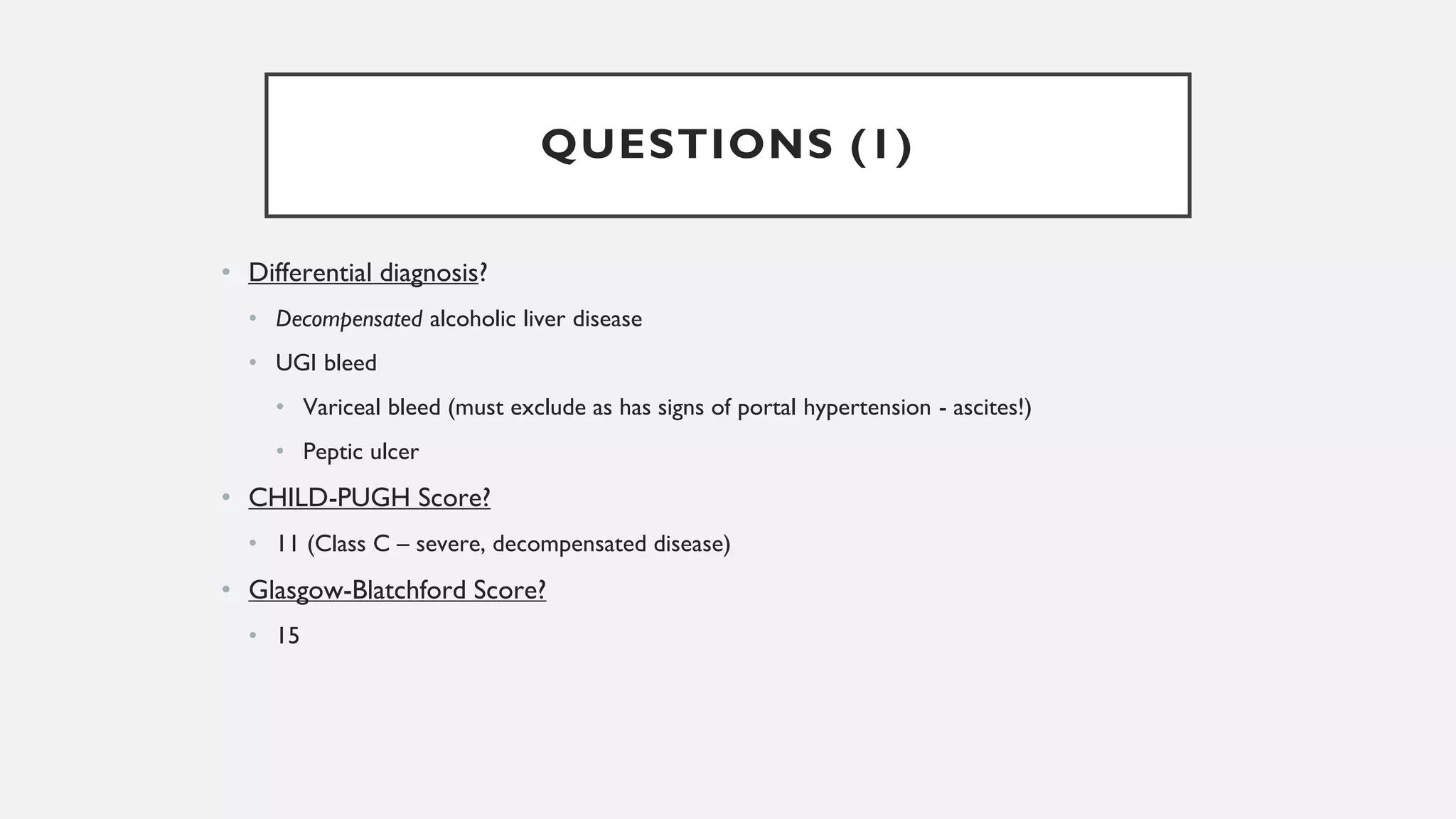
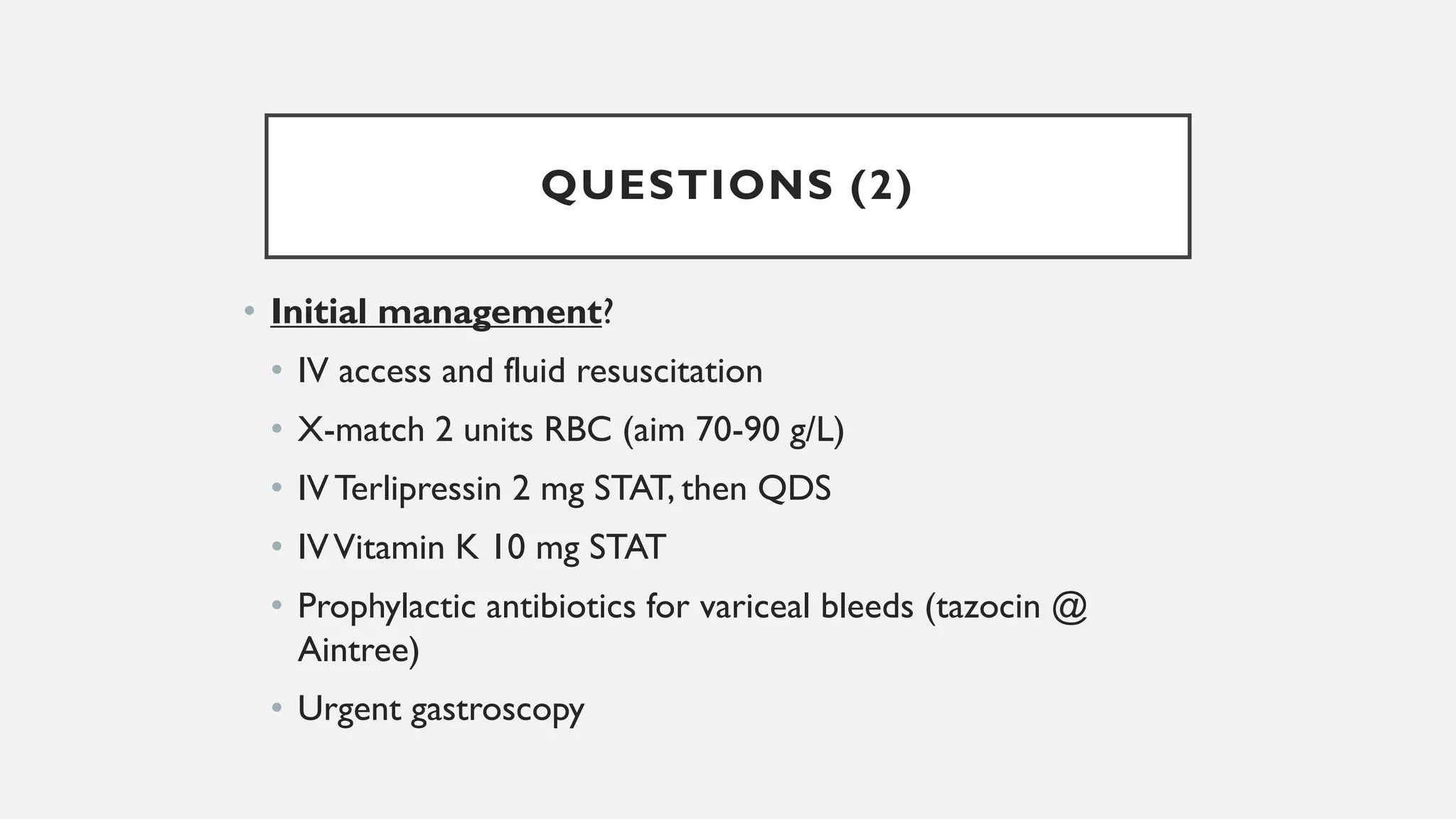
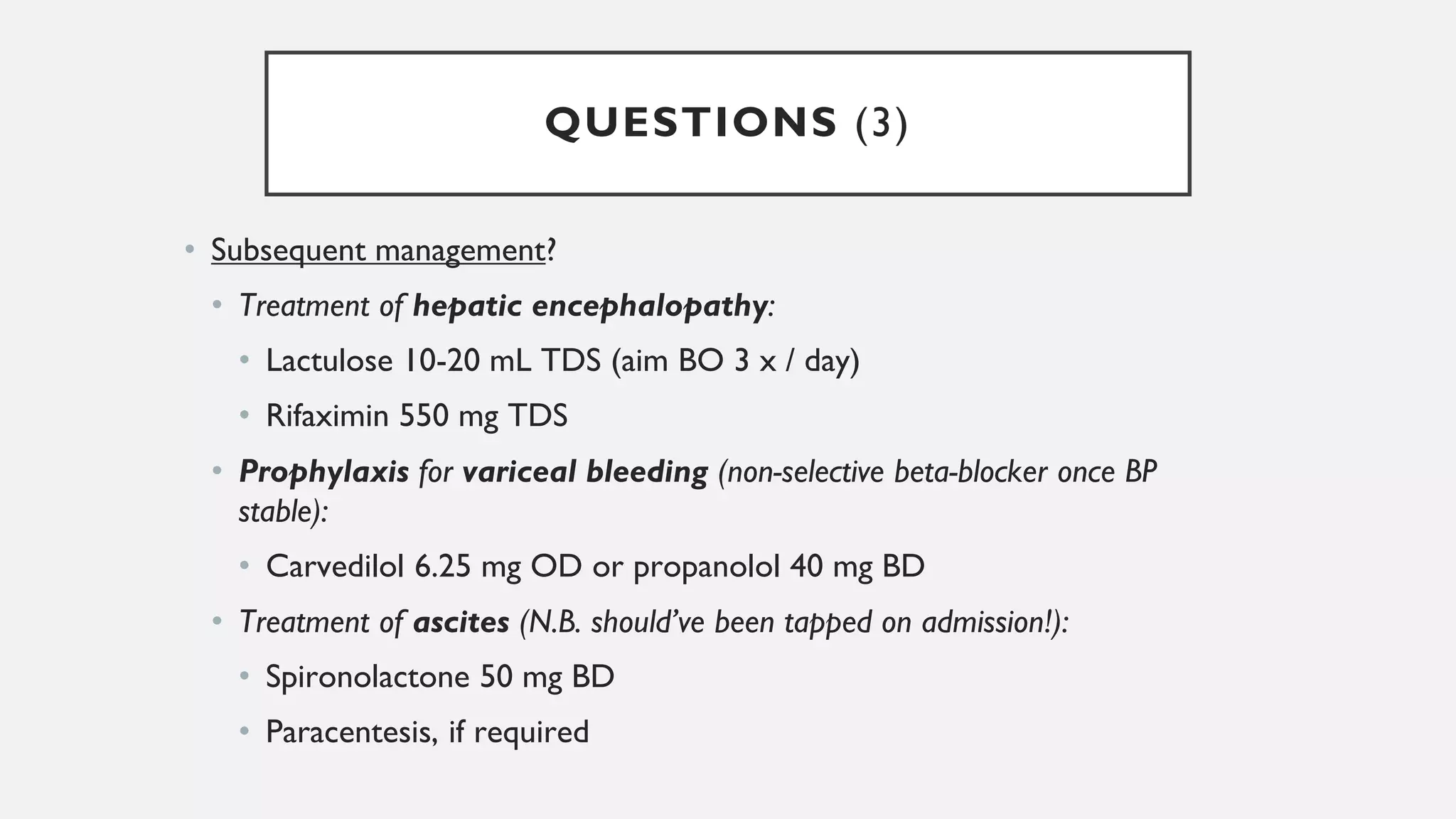
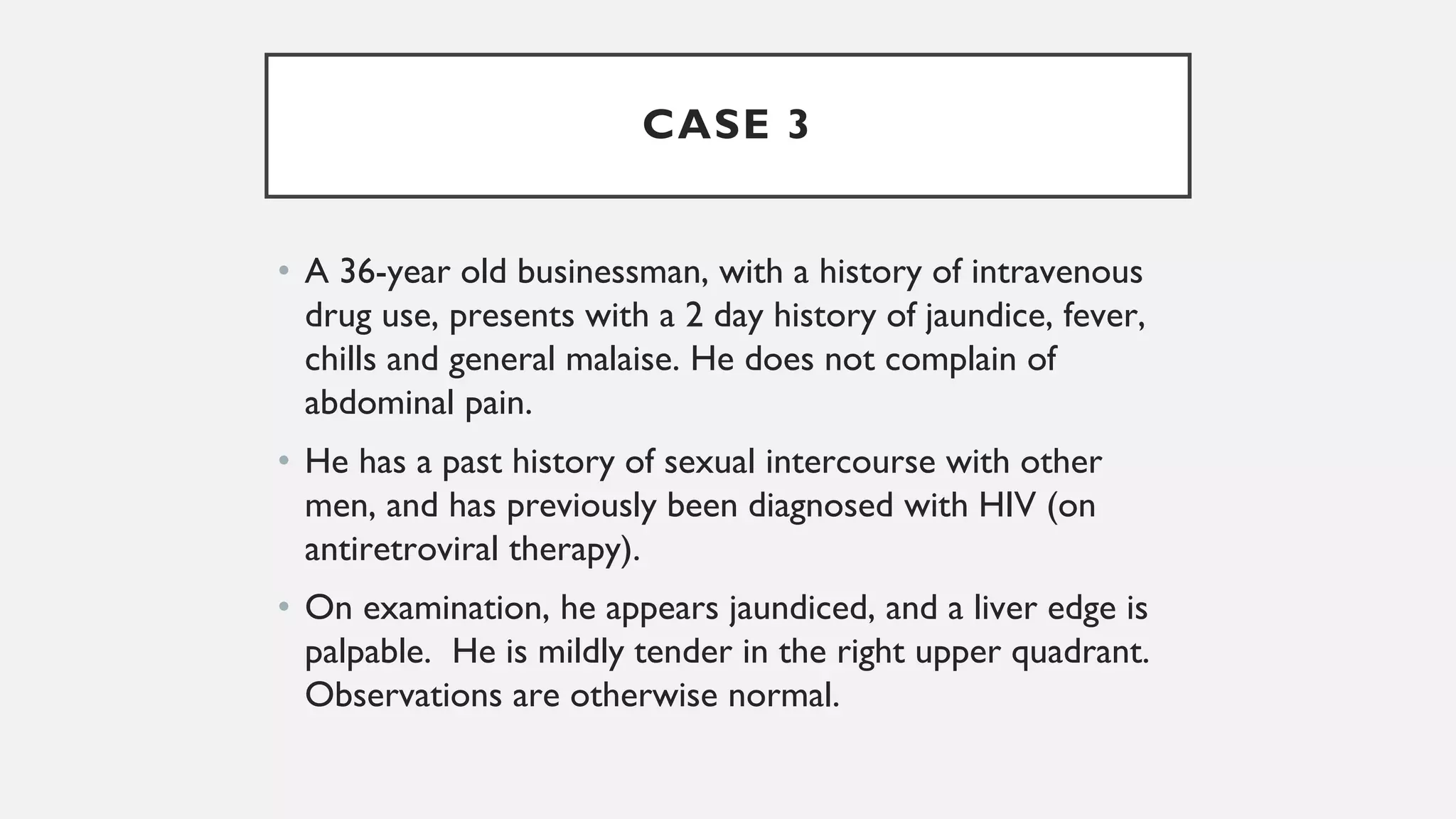
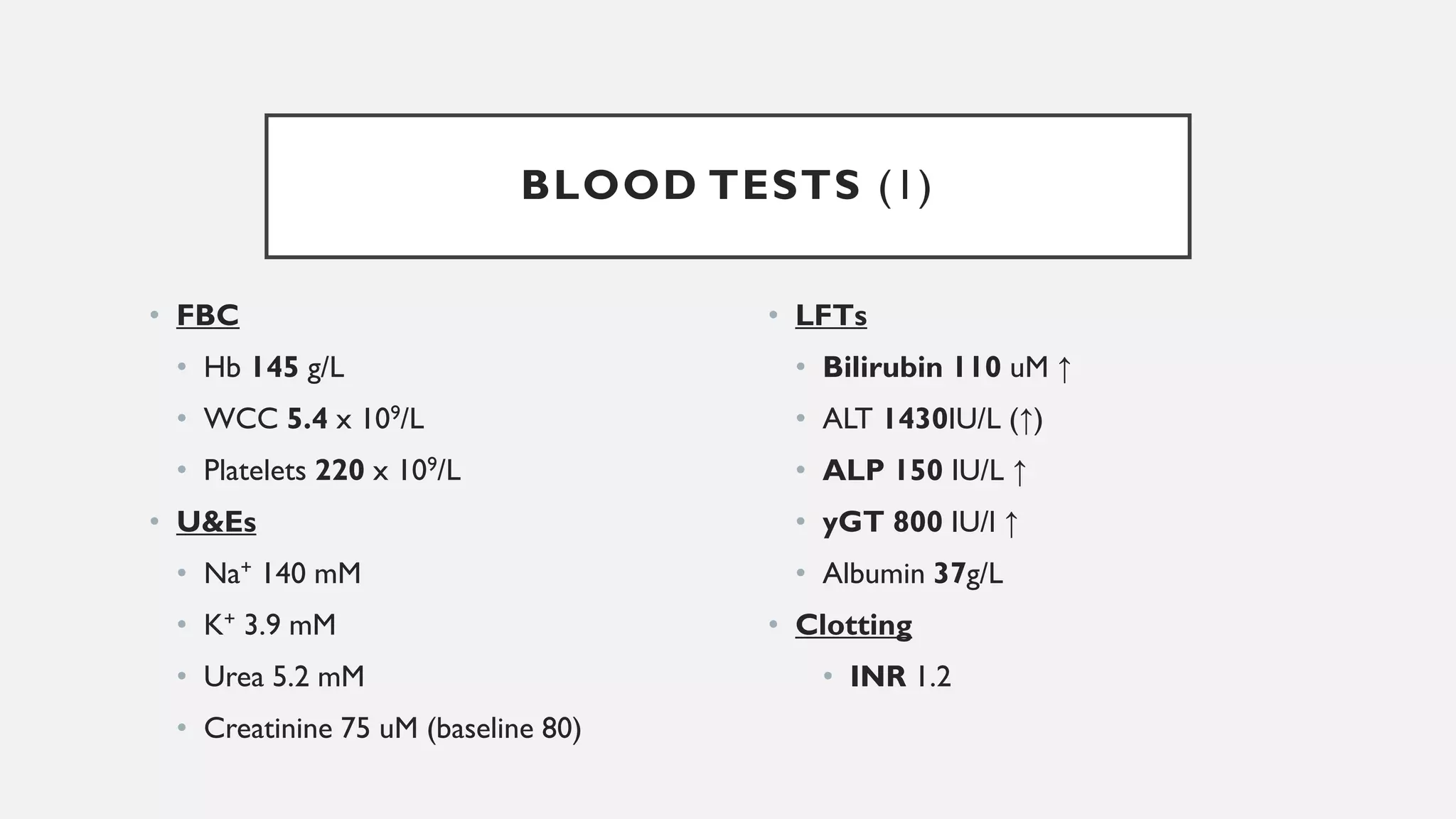
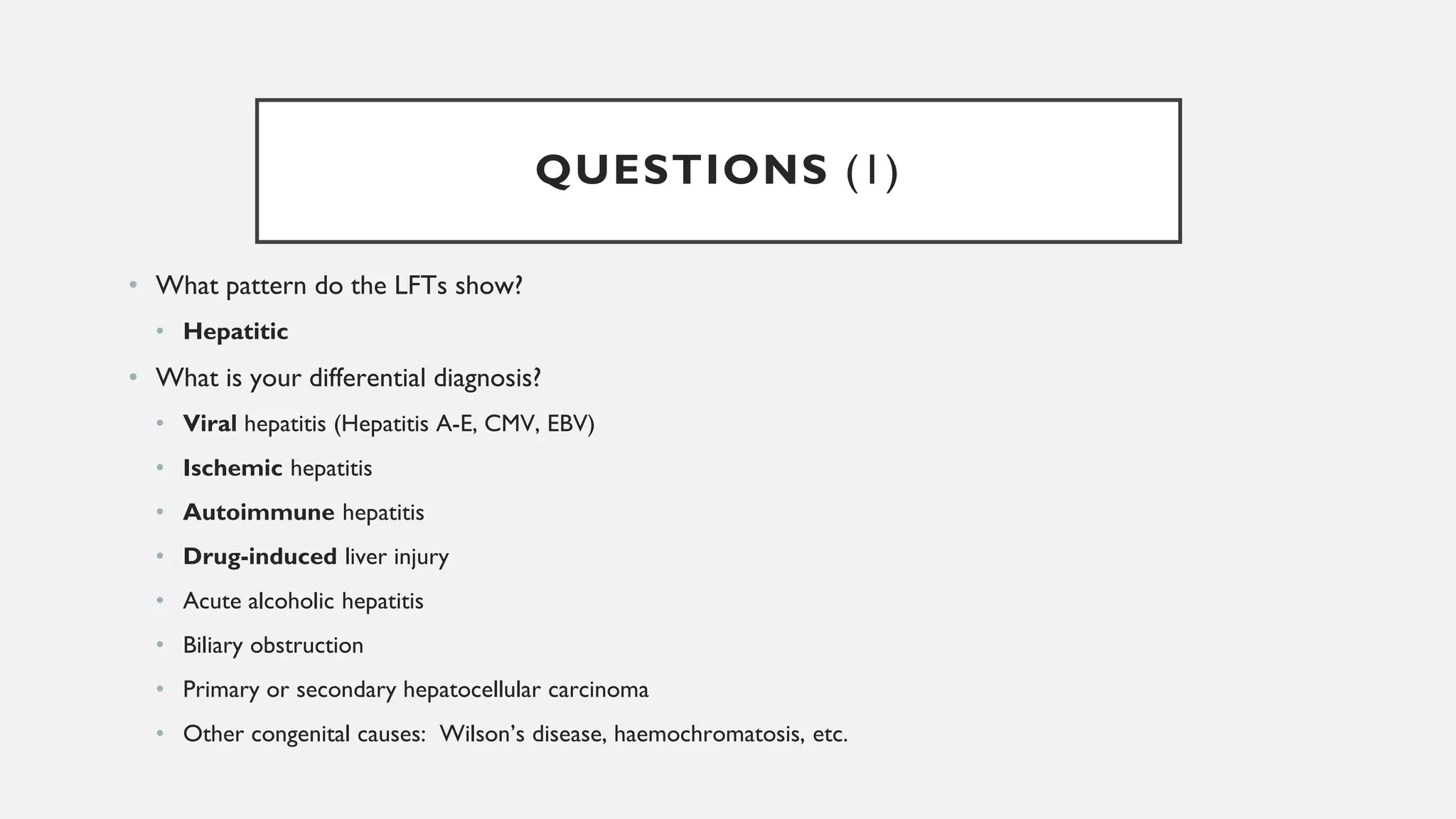
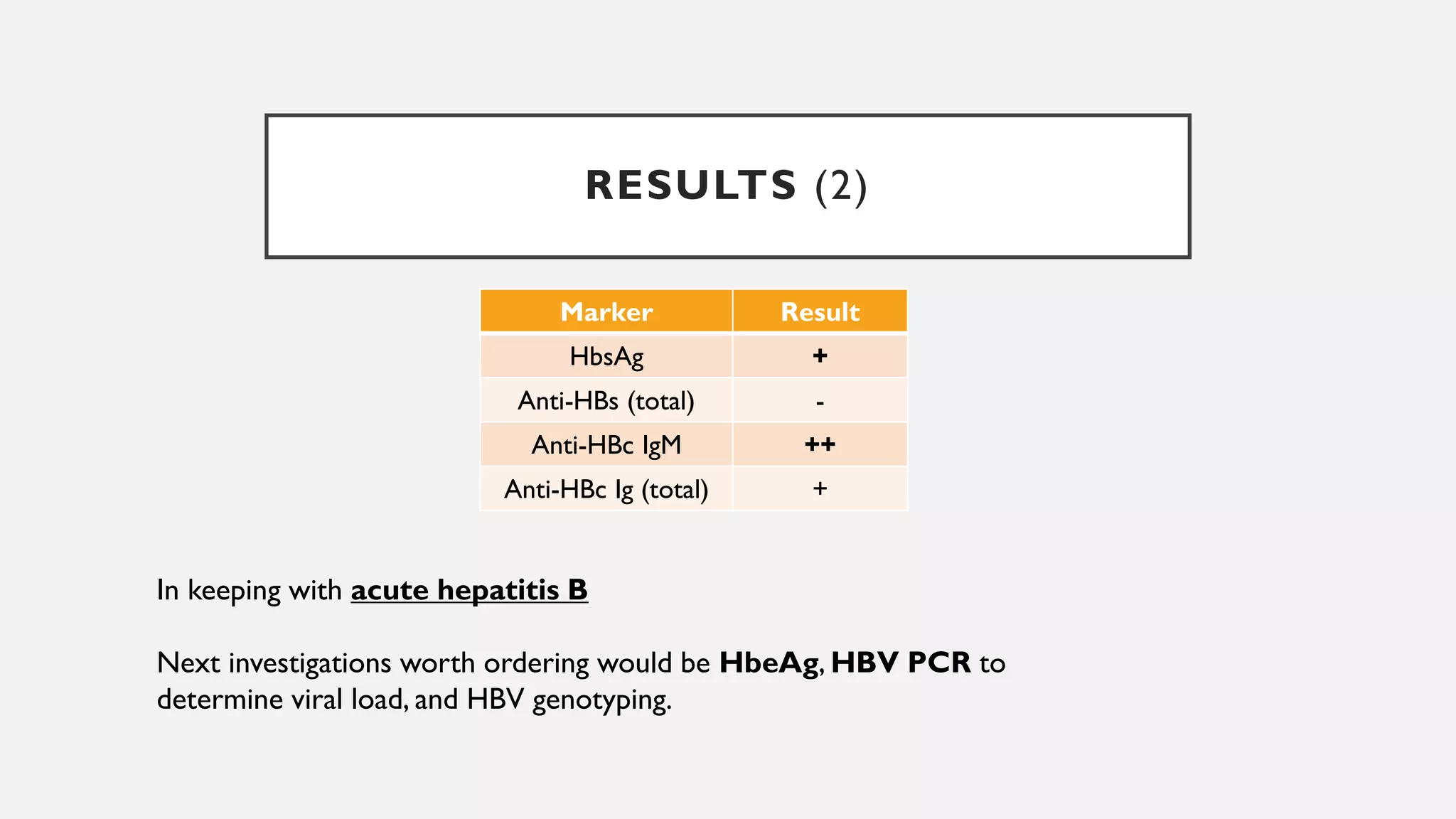
This document provides guidance on evaluating a patient presenting with jaundice. It outlines a systematic approach including focused history, examination, differential diagnosis, and appropriate lab tests and imaging. Liver function tests can indicate hepatitic or cholestatic patterns. Case examples demonstrate applying this approach, such as using imaging and endoscopy to diagnose an ampullary tumor, managing a variceal bleed in cirrhosis, and identifying acute hepatitis B. Key considerations include complications of liver disease and importance of screening high-risk populations.