Evaluation of Jaundice by Dr. Sookun Rajeev Kumar
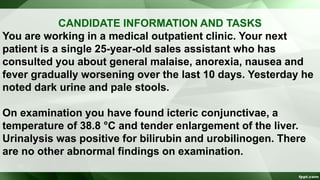
- 1. CANDIDATE INFORMATION AND TASKS You are working in a medical outpatient clinic. Your next patient is a single 25-year-old sales assistant who has consulted you about general malaise, anorexia, nausea and fever gradually worsening over the last 10 days. Yesterday he noted dark urine and pale stools. On examination you have found icteric conjunctivae, a temperature of 38.8 °C and tender enlargement of the liver. Urinalysis was positive for bilirubin and urobilinogen. There are no other abnormal findings on examination.
- 2. CANDIDATE INFORMATION AND TASKS YOUR TASKS ARE TO: 1. Take any further relevant history you require. 2. Tell the examiner what investigations you would arrange. 3. Explain the nature of the illness and possible cause to the patient, indicating which you consider to be the most likely cause. 4. Advise the patient concerning immediate management.
- 3. EVALUATION OF JAUNDICE Dr. Sookun Rajeev K (MD) Dept of General Medicine Anna Medical College
- 4. Definition: • Jaundice is the Yellow colouration of the skin, sclerae and mucous membrane which is caused by the deposition of bile pigment and usually apparent when the serum bilirubin is more than 35 mmol/l
- 5. Classification of Jaundice • Pre Hepatic Jaundice ( causes lemon-yellow skin colouration) e.g Hemolytic Jaundice • Hepatic Jaundice (causes deep yellow jaundice progressing to a greenish tinge) • Post Hepatic Jaundice • The sclerae are not coloured in those with yellow skin caused by hypercarotinaemia.
- 6. Common Causes of Jaundice Viral hepatitis Biliary obstruction from gallstones or carcinoma of the head of the pancreas Drugs (Alcohol,Acetaminophen,psy meds,diuretics,etc.. Metastases Intrahepatic cholestasis (including ascending cholangitis and primary biliary cirrhosis) Infectious mononucleosis Gilbert syndrome
- 7. Uncommon Causes of Jaundice (cont) Haemolytic anaemia Congenital hyperbilirubinaemia Stricture or carcinoma of the major bile ducts or ampulla
- 8. History • Sudden Onset : Viral hepatitis,acute biliary obstruction, trauma or toxin-mediated fulminant liver failure. • Gradual onset : chronic liver disease (including alcoholic cirrhosis) or malignancy. • A lifelong history : suggests an inherited metabolic or haemolytic cause.
- 9. History (cont) • Hx of Right Upper Quadrant pain especially after fatty meal, should suggest Cholestasis or Cholelithiasis • Hx of Fever or prior biliary surgery, points to Cholangitis • Hx of Anorexia, malaise, or myalgia, a viral etiology is most probable
- 10. History (cont) • Hx of Pruritus or weight loss associated with noninfectious etiologies. • Blood transfusion, IVD use, sexual contacts, travel to endemic areas or ingestion of contaminated foods expose patients to viral related Hepatocellular injury. • PMHx,PSHx,FHx of inherited defect in bilirubin conjugation or transport,wilson’s disease,hemochromatoses
- 11. Signs & Symptoms in Jaundice Dark urine
- 12. Signs & Symptoms in Jaundice (cont) Yellow coloration of the skin – should be examined in natural white light Steatorrhea – suggests no breakdown of fats Pruritus - suggests chronic disease Abdominal pain - suggests biliary tract obstruction from stone or pancreatic tumour (obstructive jaundice)
- 13. Signs & Symptoms in Jaundice (cont) Clay coloured stool Painless jaundice in the elderly - think of pancreatic cancer, although most patients with pancreatic cancer have pain Kernicterus - rarely seen in adults due to maturation of blood brain barrier
- 14. Signs & Symptoms in Jaundice (cont)
- 15. Signs & Symptoms in Jaundice (cont) Spider Angioma Caput medusa Gynecomastia Testicular Atrophy Palmar Erythema Dupuytren’s contracture • All suggest Chronic Liver Disease and Portal Hypertension
- 16. Specific features on examination of the abdomen in a jaundiced patient include • Recent operation scars: suggesting cholecystectomy or surgery for intra- abdominal carcinoma • Palpable Enlarged Gall Bladder suggesting bile duct obstruction caused by carcinoma of the pancreas (rather than gallstones)
- 17. Specific features on examination of the abdomen in a jaundiced patient include (cont) • Hepatomegaly: irregular when infiltrated with carcinoma or in early cirrhosis, tender in infectious and acute alcoholic hepatitis and occasionally in congestive heart failure
- 18. Specific features on examination of the abdomen in a jaundiced patient include (cont) • Splenomegaly in portal hypertension, spherocytosis and infectious mononucleosis
- 19. Specific features on examination of the abdomen in a jaundiced patient include (cont) • Ascites.
- 20. Aims for Investigations 1. Investigation aims to discover the site of any biliary outflow obstruction 2. Determine the degree of impairment of liver cell function and its cause 3. Eliminate rare causes such as haemolysis 4. Establish potential for treatment.
- 21. 1. Haematology Full blood count, reticulocyte count and Coombs’ test A normal reticulocyte count virtually excludes haemolytic jaundice. Leukocytosis may suggest infection or carcinoma. Abnormal mononuclear cells suggest infectious mononucleosis or viral hepatitis.
- 22. 2. Liver Function Tests Measure the ability of the liver to perform normal functions (e.g. serum albumin is a measure of protein synthesis; prothrombin time is a measure of synthetic function; bilirubin is a measure of bile salt conjugation and excretion). Liver enzymes (alkaline phosphatase, transaminases) are indicators of ductal or liver cell damage. In obstructive jaundice the alkaline phosphatase is greatly elevated compared with transaminases; in hepatocellular disease transaminases are predominantly raised.
- 23. 3. Bilirubin Bilirubin derived from red cell breakdown is transported to the liver where it is conjugated to glucuronic acid. Conjugated bilirubin is secreted in the bile and degraded in the gut by bacteria to form urobilinogen. Urobilinogen is either excreted in the stool or reabsorbed from the gut and excreted by the kidneys. Serum bilirubin is predominantly unconjugated in haemolytic jaundice and the other liver function tests are usually normal. It is mainly conjugated in obstructive jaundice.
- 24. 3. Bilirubin (cont) Causes of increased bilirubin Hepatocellular failure Biliary obstruction Haemolysis Gilbert syndrome
- 25. 4. Alkaline Phosphatase Elevated in Obstructive jaundice Hepatocellular jaundice Growth in adolescence Pregnancy Normal in Gilbert syndrome Myeloma Alkaline phosphatase is found in high levels in biliary Canaliculi, osteoblasts, intestinal mucosa and placenta.
- 26. 4. Alkaline Phosphatase (cont) • A raised level in the absence of other signs of liver disease or abnormal liver function tests suggests the presence of malignant secondary deposits in the bone or Paget’s disease. Consider measuring isoenzymes if there is doubt.
- 27. 4. Alkaline Phosphatase (cont) Causes of increased hepatic alkaline phosphatase Extra-hepatic cholestasis Obstructive jaundice Intra-hepatic cholestasis (e.g. cirrhosis, drugs, cholangitis, primary biliary cirrhosis) Obstructive phase of hepatitis Causes of increased bone alkaline phosphatase (osteoblastic activity) Paget’s disease Bone metastases Osteomalacia Hyperparathyroidism Normal growth in puberty Fractures
- 28. 5. Transaminases Elevated serum transaminases (alanine aminotransferase, aspartate aminotransferase and gamma glutamyl transferase) indicate hepatocellular damage. Slight elevation is consistent with obstructive jaundice.
- 29. 5. Transaminases (cont) Causes of elevated alanine aminotransferase Active liver cell damage, including drugs, hepatitis and metastatic infiltration Acute myocardial infarction (peaks at 24–48 h, may fall to normal by 72h). The degree of elevation reflects the amount of muscle damage Acute pancreatitis Haemolysis
- 30. 5. Transaminases (cont) Elevated aspartate aminotransferase levels parallel the alanine aminotransferase -glutamyl transferase Inducible microsomal enzyme Most sensitive index of alcohol ingestion Raised in most forms of liver disease including acute and chronic hepatitis, cirrhosis and following drugs that induce microsomal enzymes
- 31. 6. Urinalysis Conjugated bilirubin renders the urine dark yellow Urobilinogen is colourless but on standing the urine turns brown as urobilinogen is converted to urobilin by oxidation. Haemolytic jaundice is acholuric (no bilirubin in the urine) but the urine contains excess urobilinogen because excess bilirubin reaches the intestine and is re-excreted as urobilinogen. Obstructive jaundice produces dark brown urine with excess bilirubin but a reduction of urinary urobilinogen (little or no bilirubin reaches the gut because of the obstruction and therefore cannot be reabsorbed and re-excreted).
- 32. 6. Urinalysis (cont) In the early stages of acute viral hepatitis, excess urobilinogen may sometimes be present before clinical jaundice becomes apparent. This is a result of failure of the liver to take up the excess urobilinogen absorbed from the gut. With increasing severity, biliary obstruction develops and as conjugated bilirubin appears in the urine it disappears from the gut and urobilinogen disappears from the urine. The reciprocal effect also occurs during recovery.
- 33. 7. Serology Viral hepatitis serology – hepatitis A–E, cytomegalo- virus (CMV) and Epstein–Barr virus (EBV) Antimitochondrial antibodies (primary biliary cirrhosis) Antinuclear factor and smooth-muscle antibodies (chronic active hepatitis)
- 34. 8. Abdominal Radiology in jaundice Plain X-ray and ultrasound may show gallstones.
- 35. 8. Abdominal Radiology in jaundice (cont) Ultrasound, CT and MRI may show prImary or secondary tumours, pancreatic carcinoma, stones in the gall bladder and dilated biliary ducts in obstruction. Isotope liver scans may demonstrate secondary deposits.
- 36. 9. Needle Liver Biopsy Biliary obstruction is a relative contraindication because of the potential danger of biliary peritonitis. Ultrasound and CT-guided biopsy may provide the histological diagnosis in focal lesions. Check the prothrombin time and platelet counts are normal. Fresh frozen plasma will quickly reverse the prothrombin time for the duration of the procedure.
- 37. 9. Needle Liver Biopsy (cont)
- 38. 10. Other investigations Endoscopic retrograde cholangiopancreatography (ERCP) is valuable to define obstruction of the pancreaticoduodenal tree, for sphincterotomy, to release stones and to relieve obstruction by insertion of a stent. -fetoprotein is raised in hepatocellular carcinoma.
- 39. ERCP