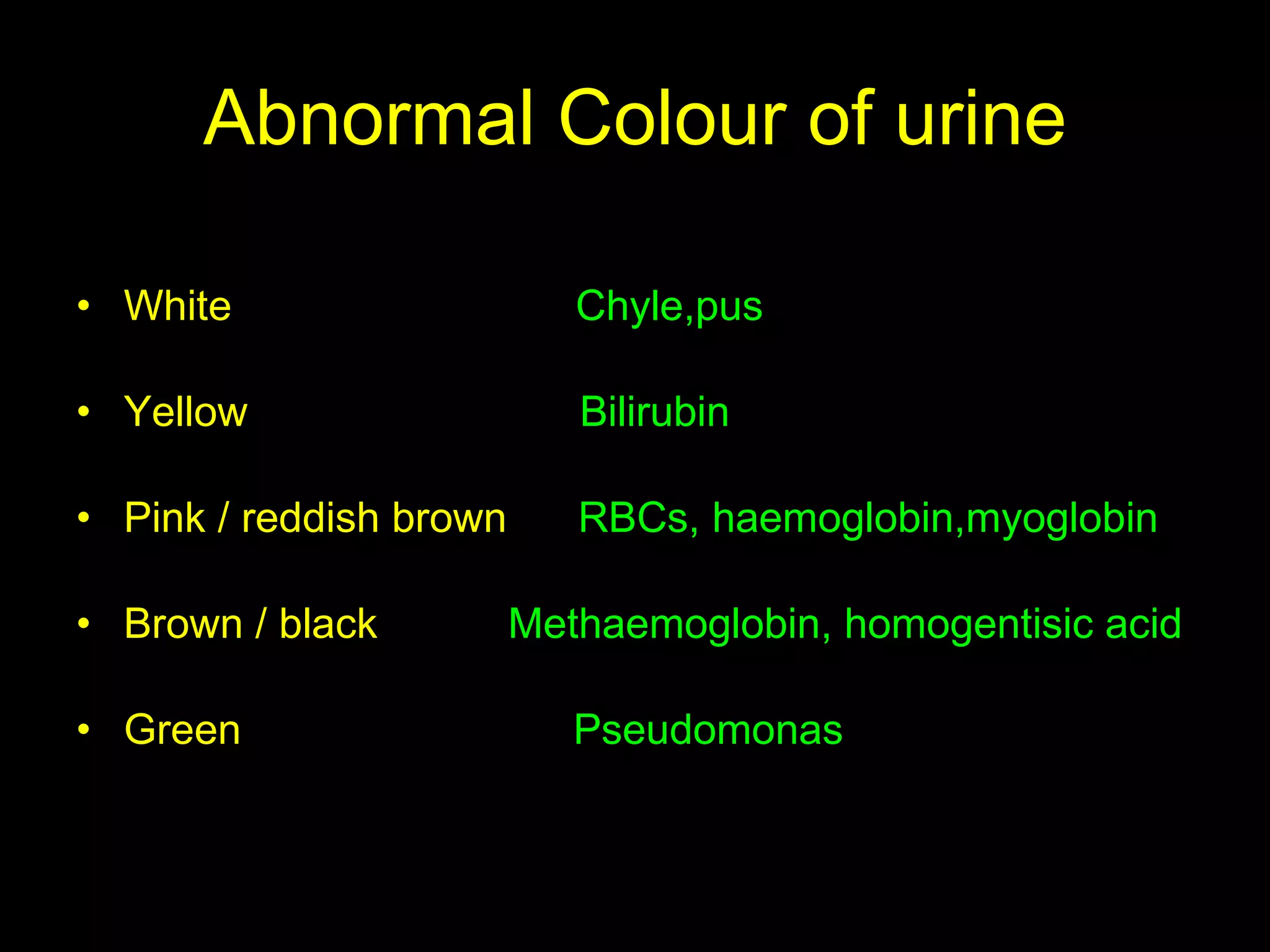
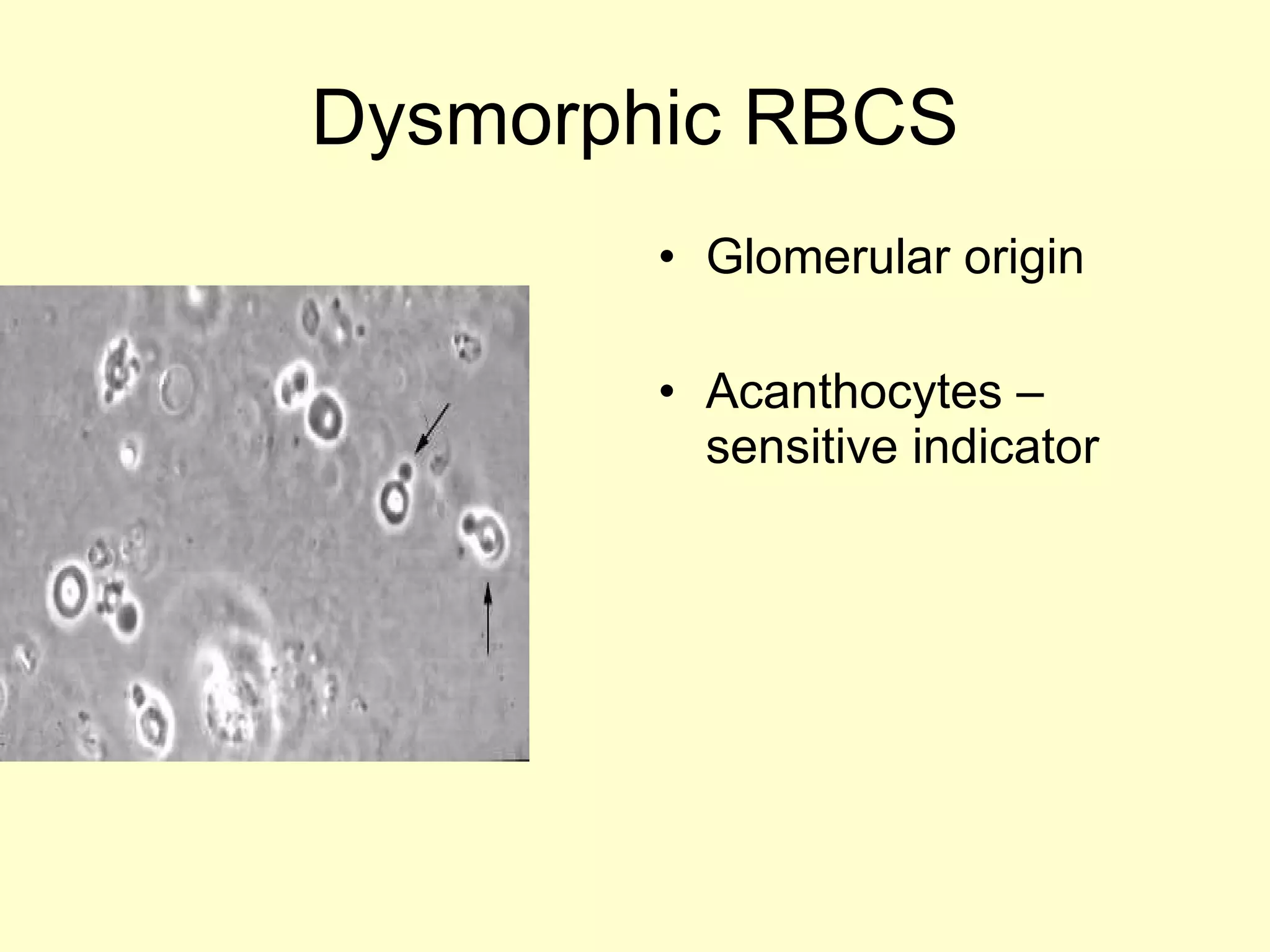
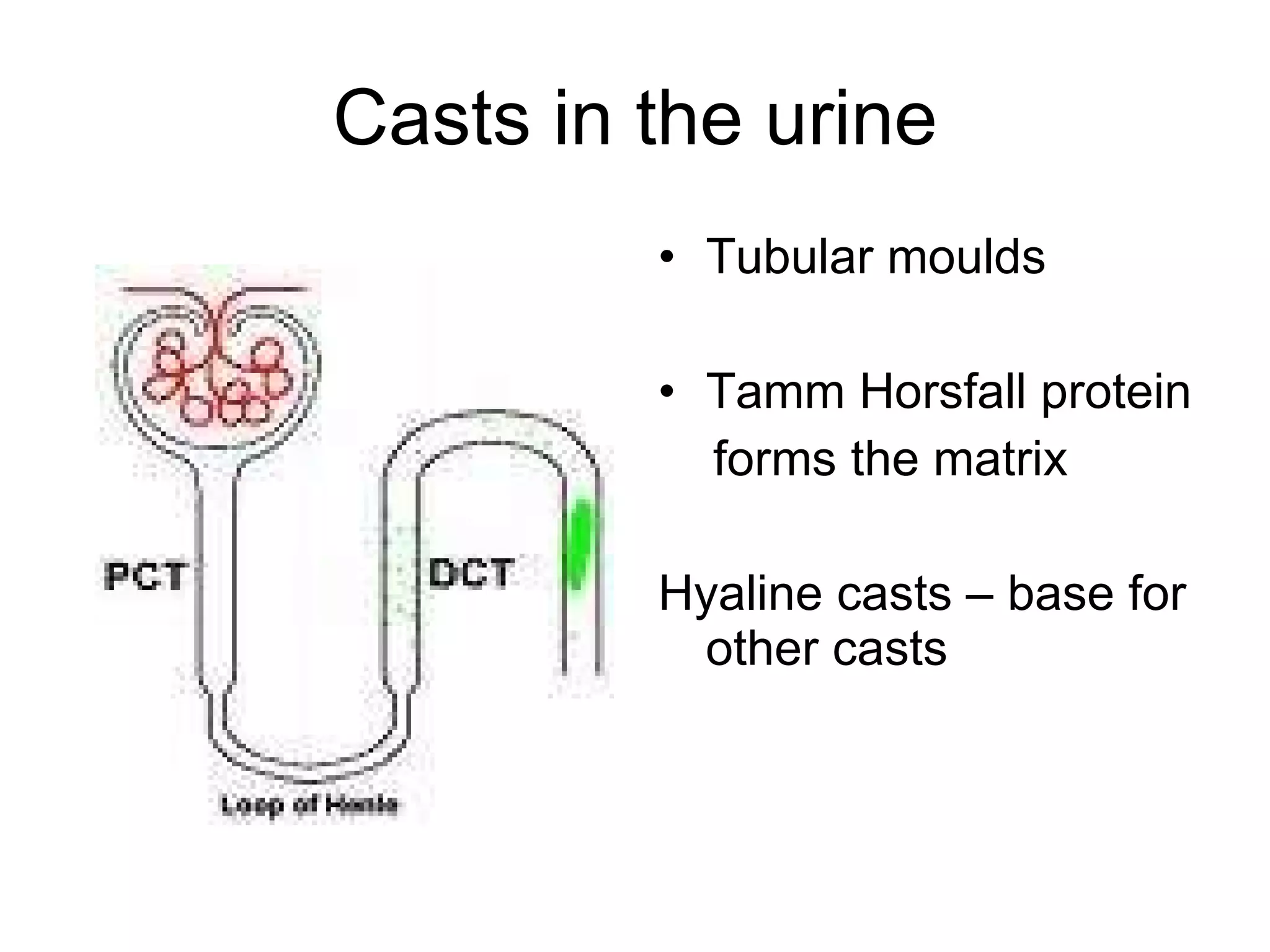
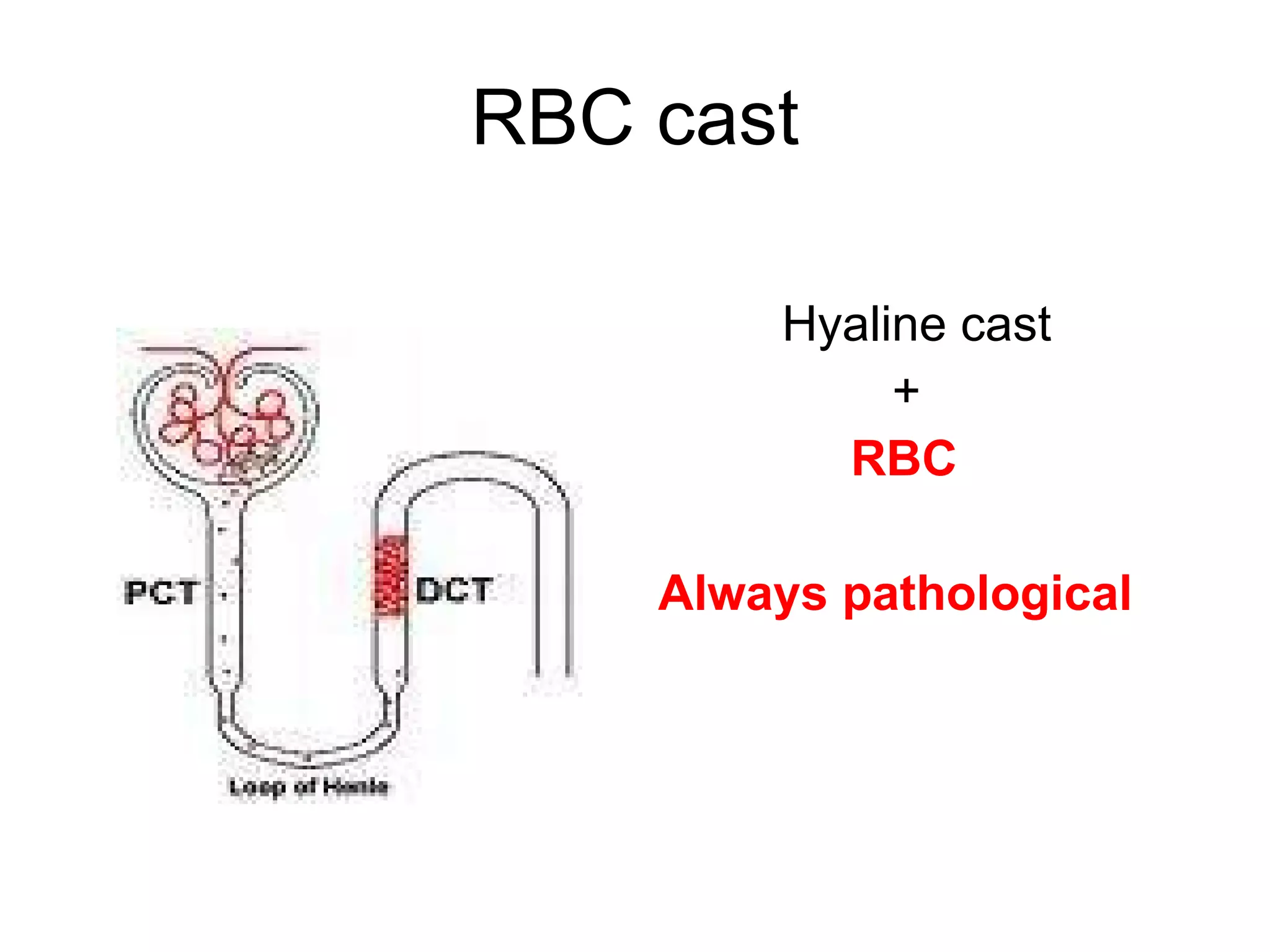
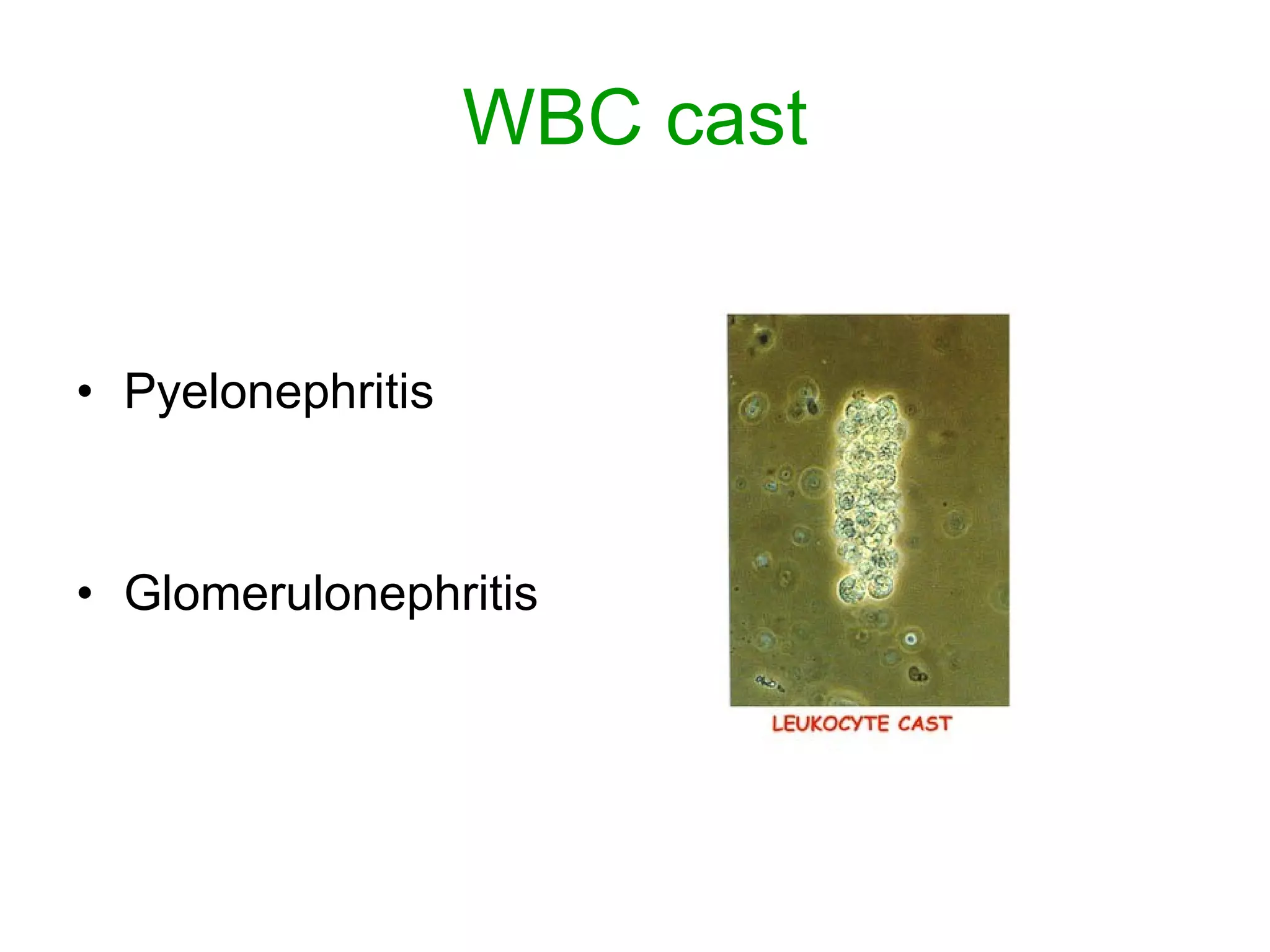
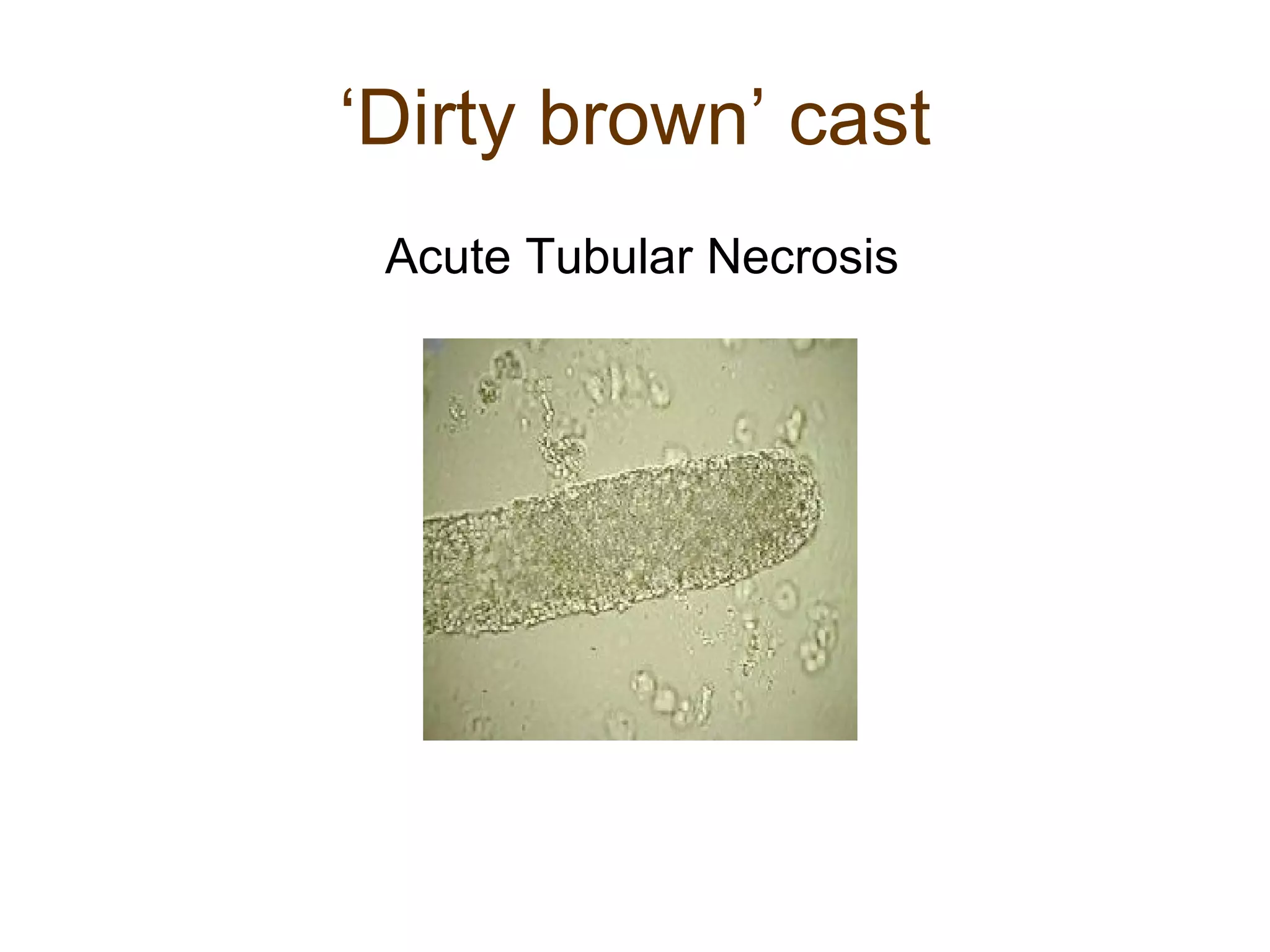
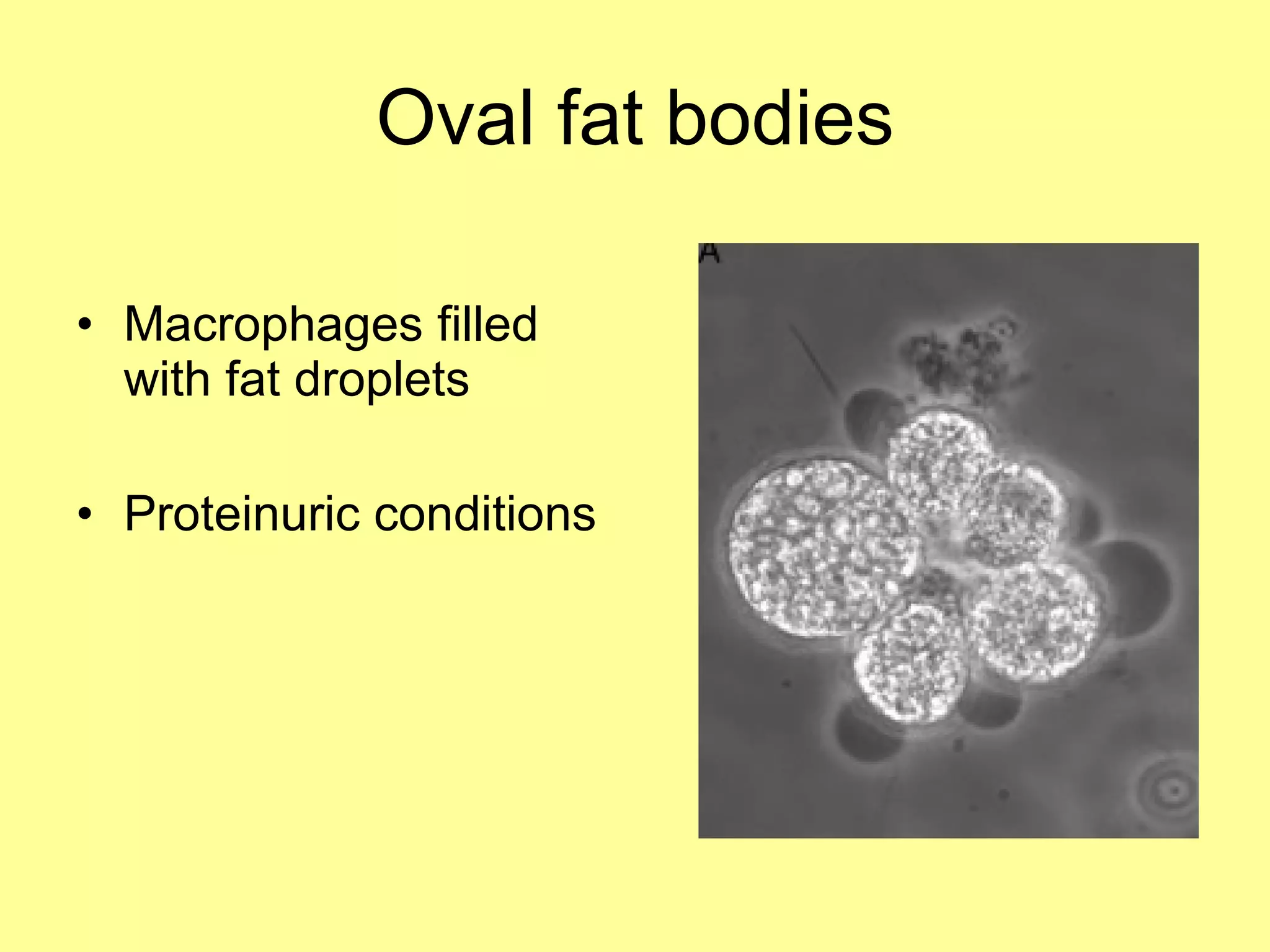
This document provides an overview of urinalysis, which is a key test in clinical nephrology. It describes the aims of urinalysis to examine the physical characteristics, chemical composition, cellular elements, and microorganisms in urine. It then explains how dipstick tests can assess various analytes like pH, protein, blood, and others. The document also covers urine microscopy to examine elements like erythrocytes, leukocytes, epithelial cells, casts, crystals, and microorganisms that can indicate underlying kidney conditions.