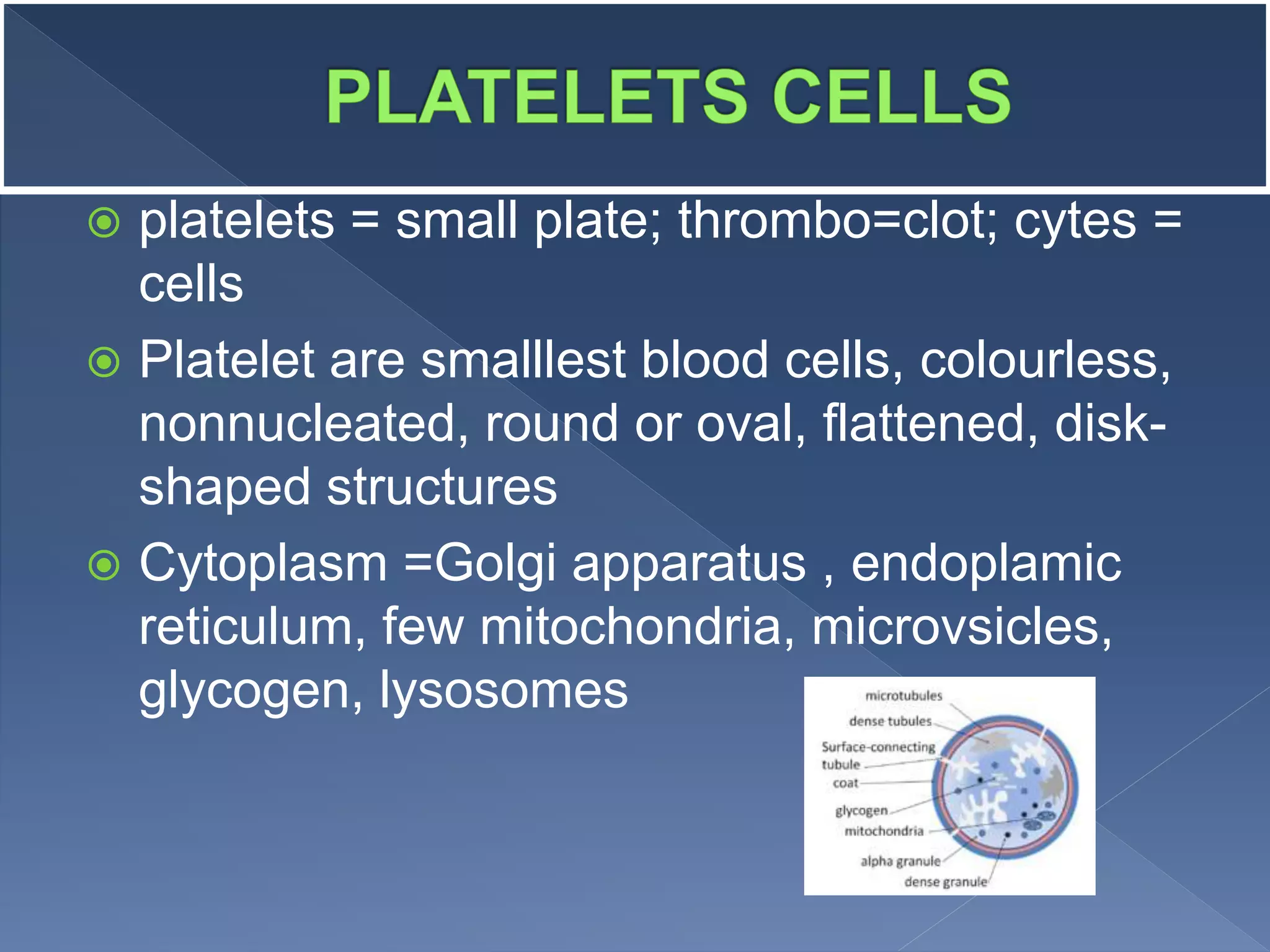
Platelets are cell fragments produced by megakaryocytes in the bone marrow that help the body form blood clots to stop bleeding. They have no nucleus and an average lifespan of 8-9 days. Platelets attach to damaged blood vessel walls and release chemicals that attract more platelets to form a hemostatic plug to stop bleeding. Low platelet counts can cause excessive bleeding while high counts have few symptoms. Platelet counts are regulated by thrombopoietin and can be affected by disease, medications, and lifestyle factors.