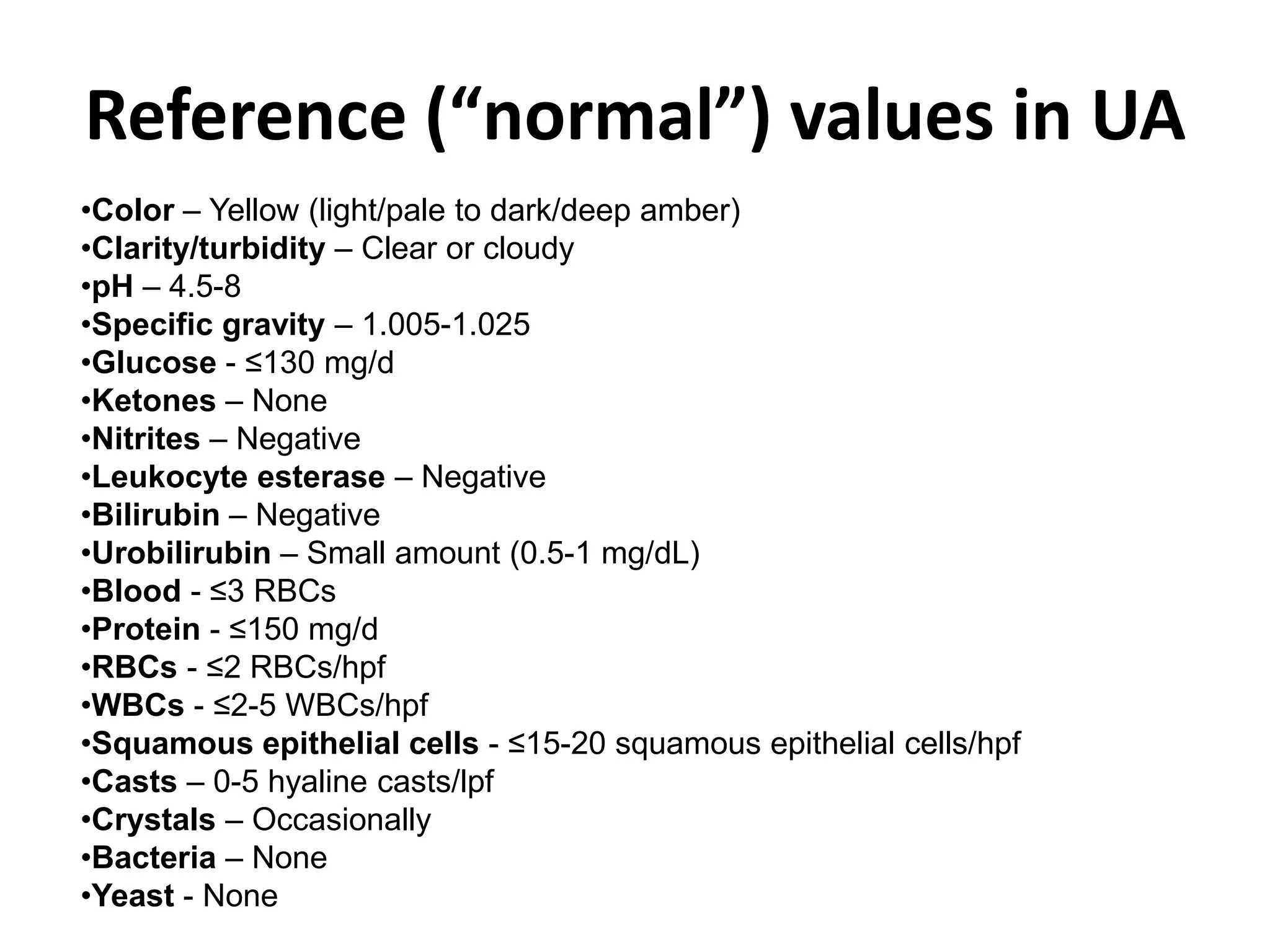
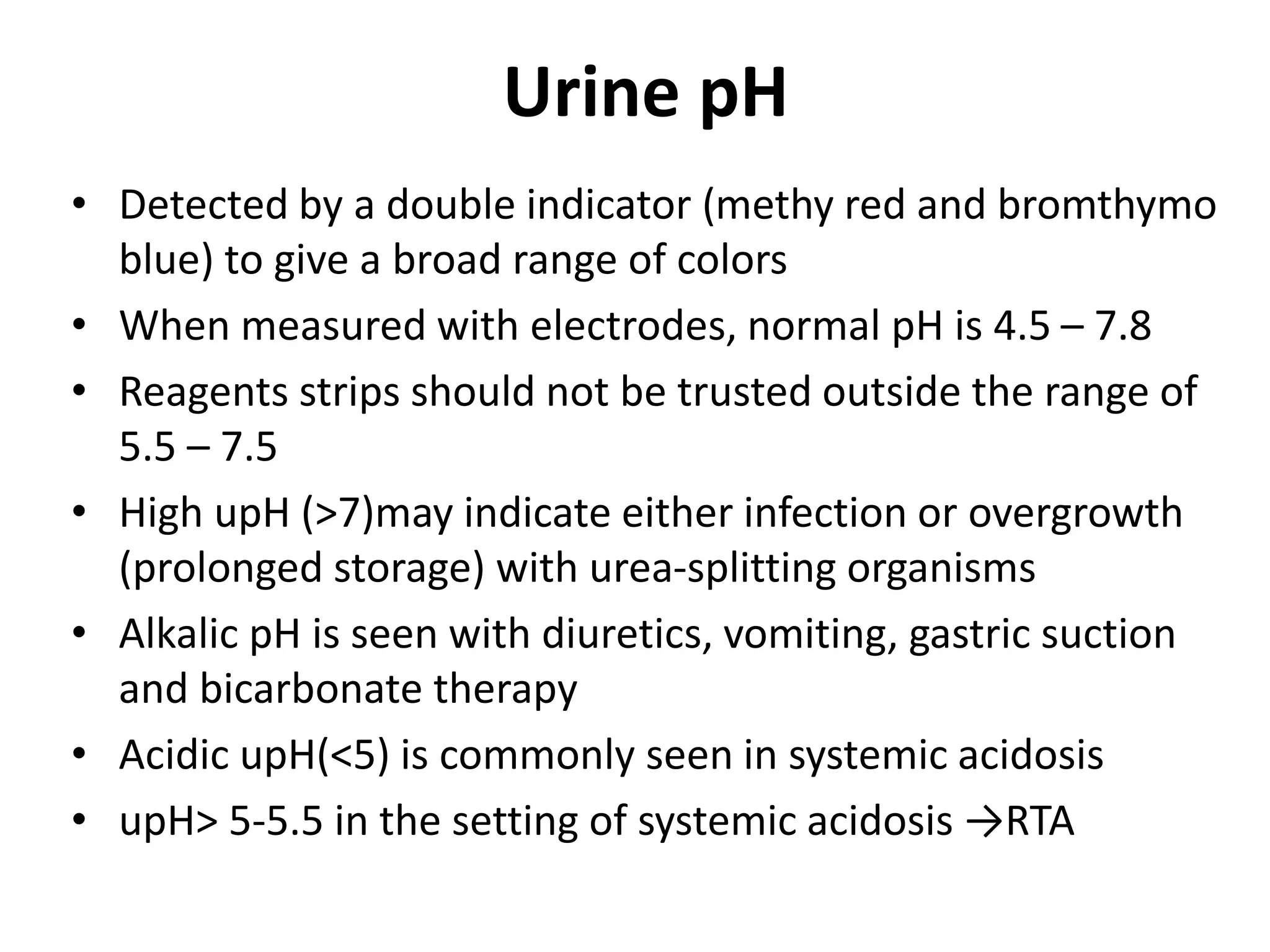
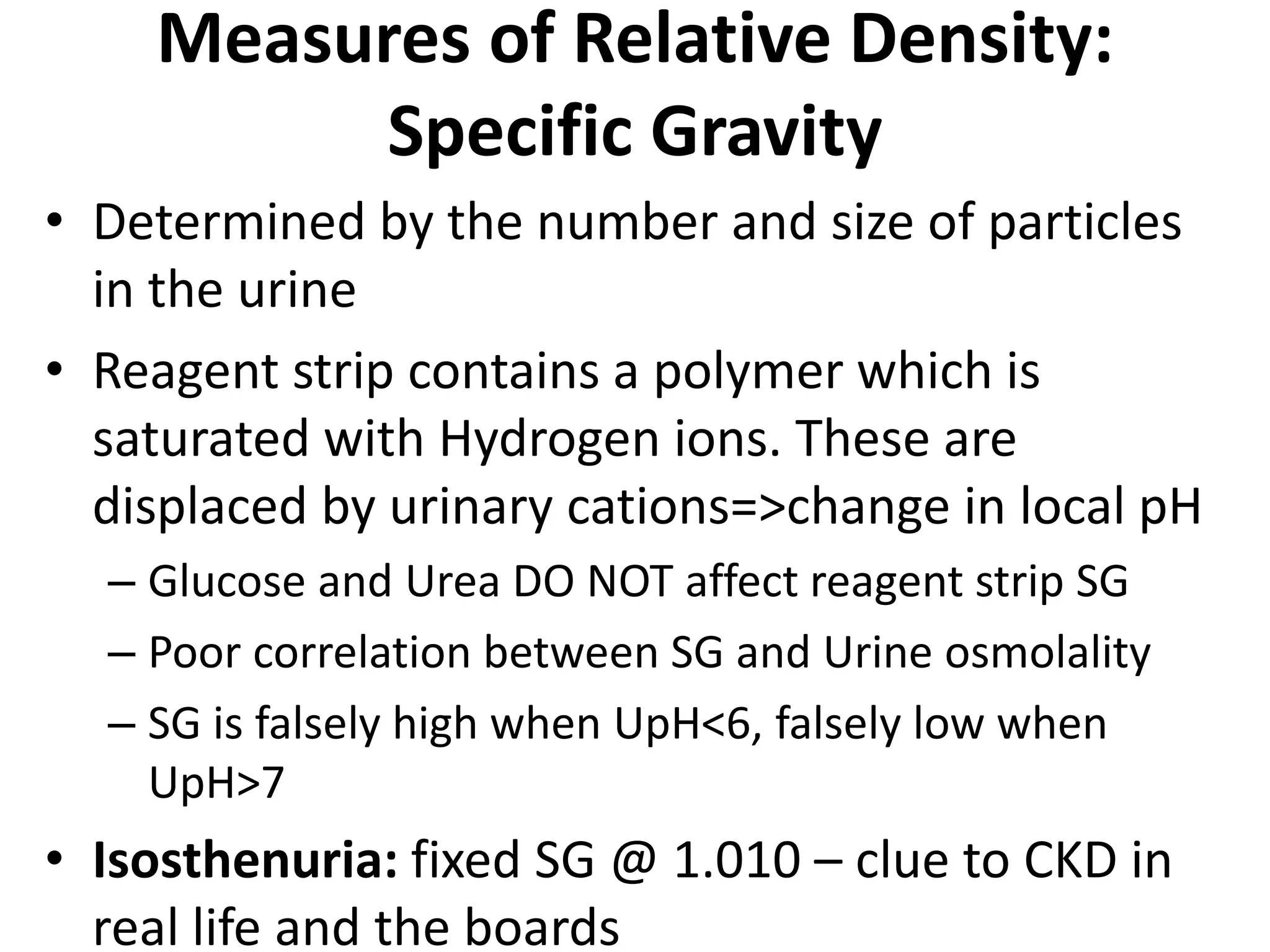
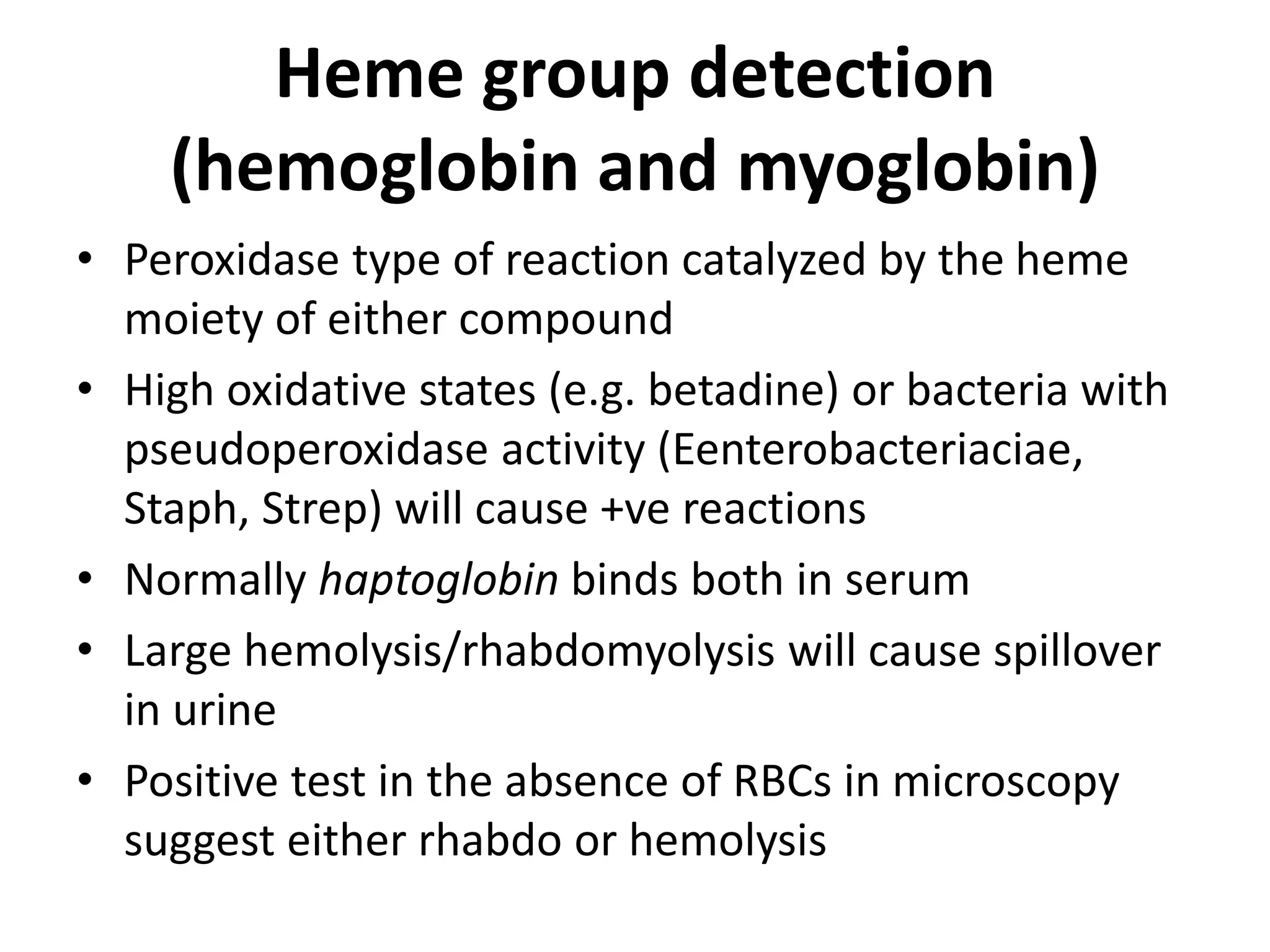
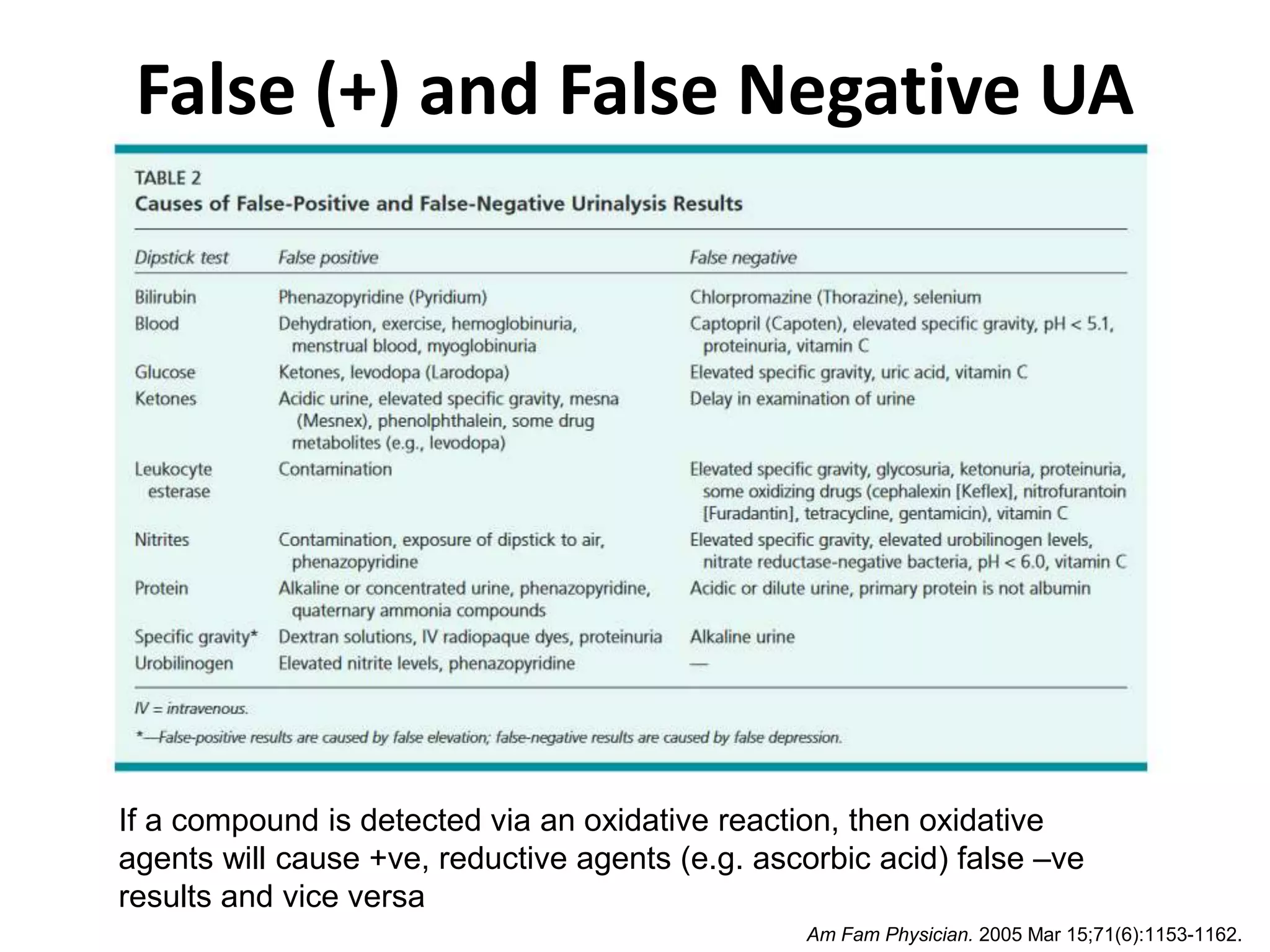
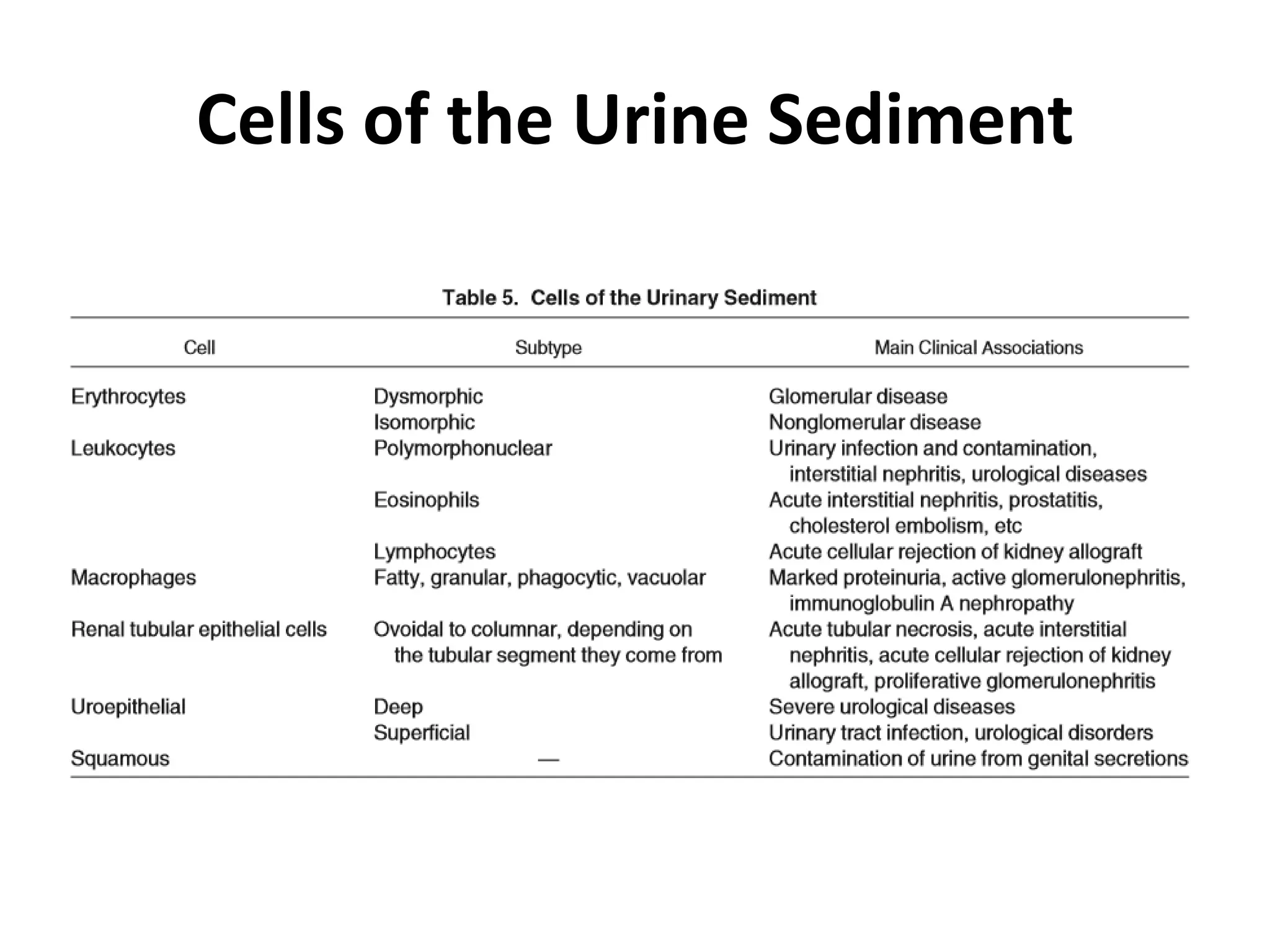
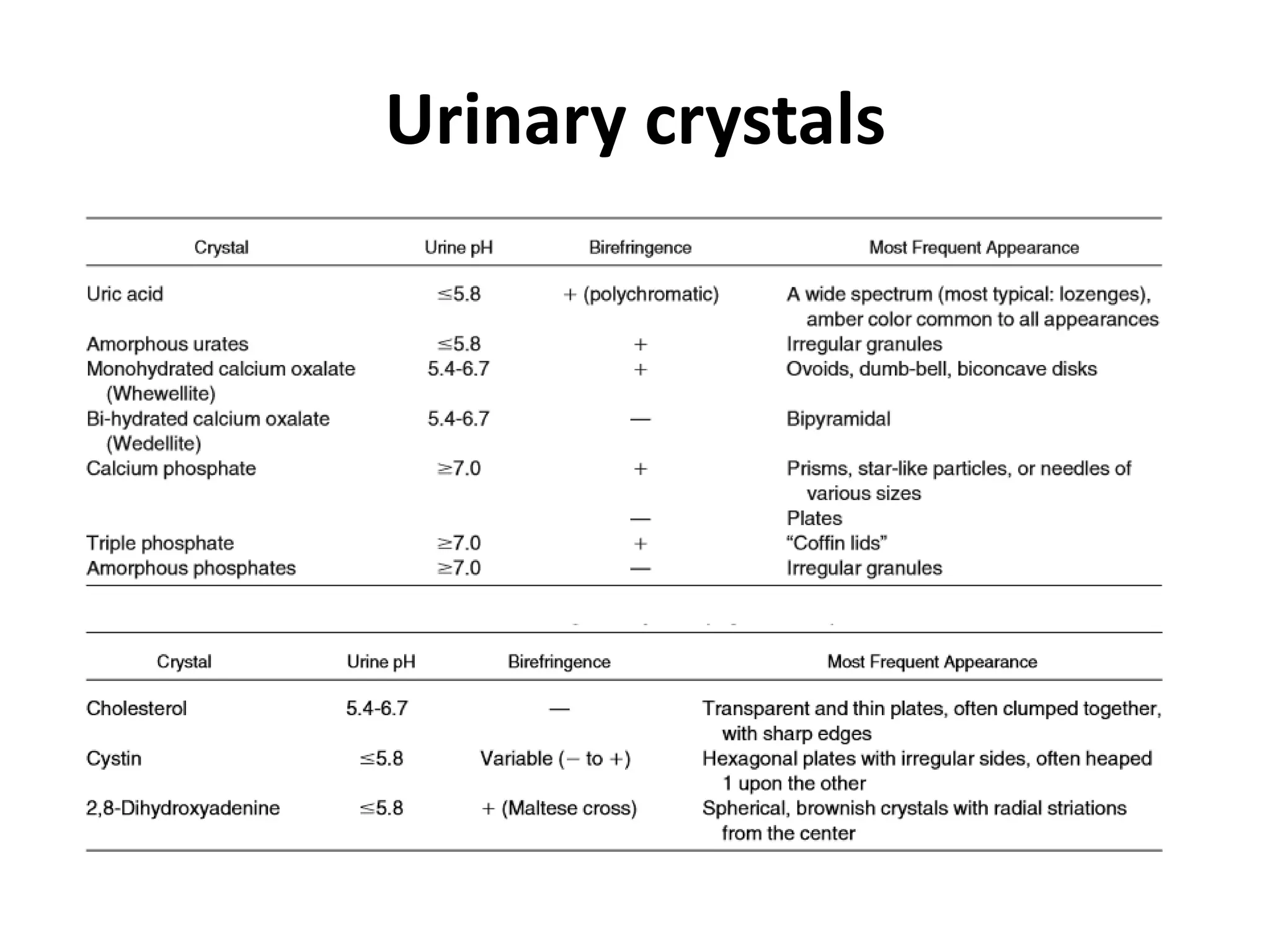
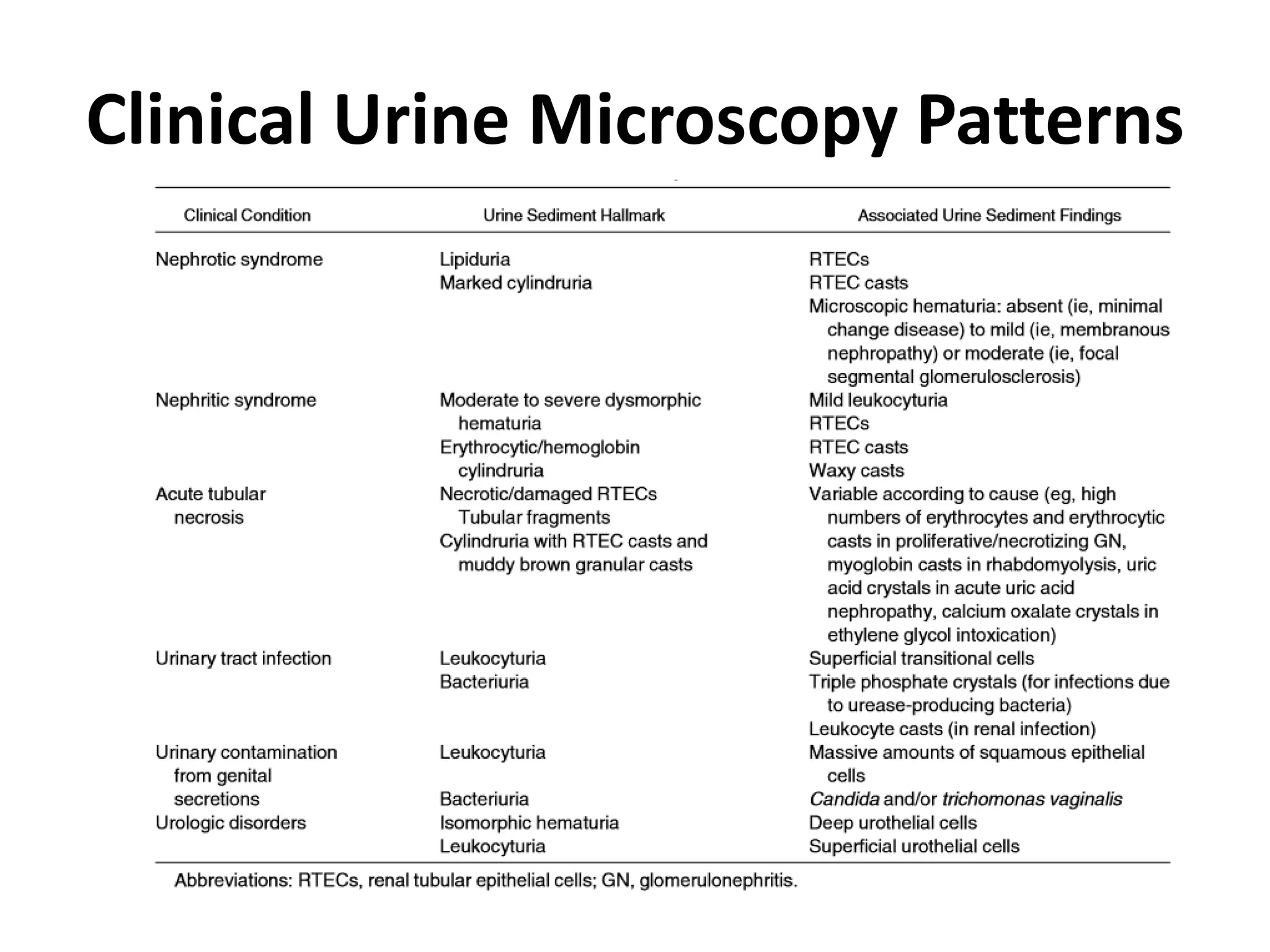
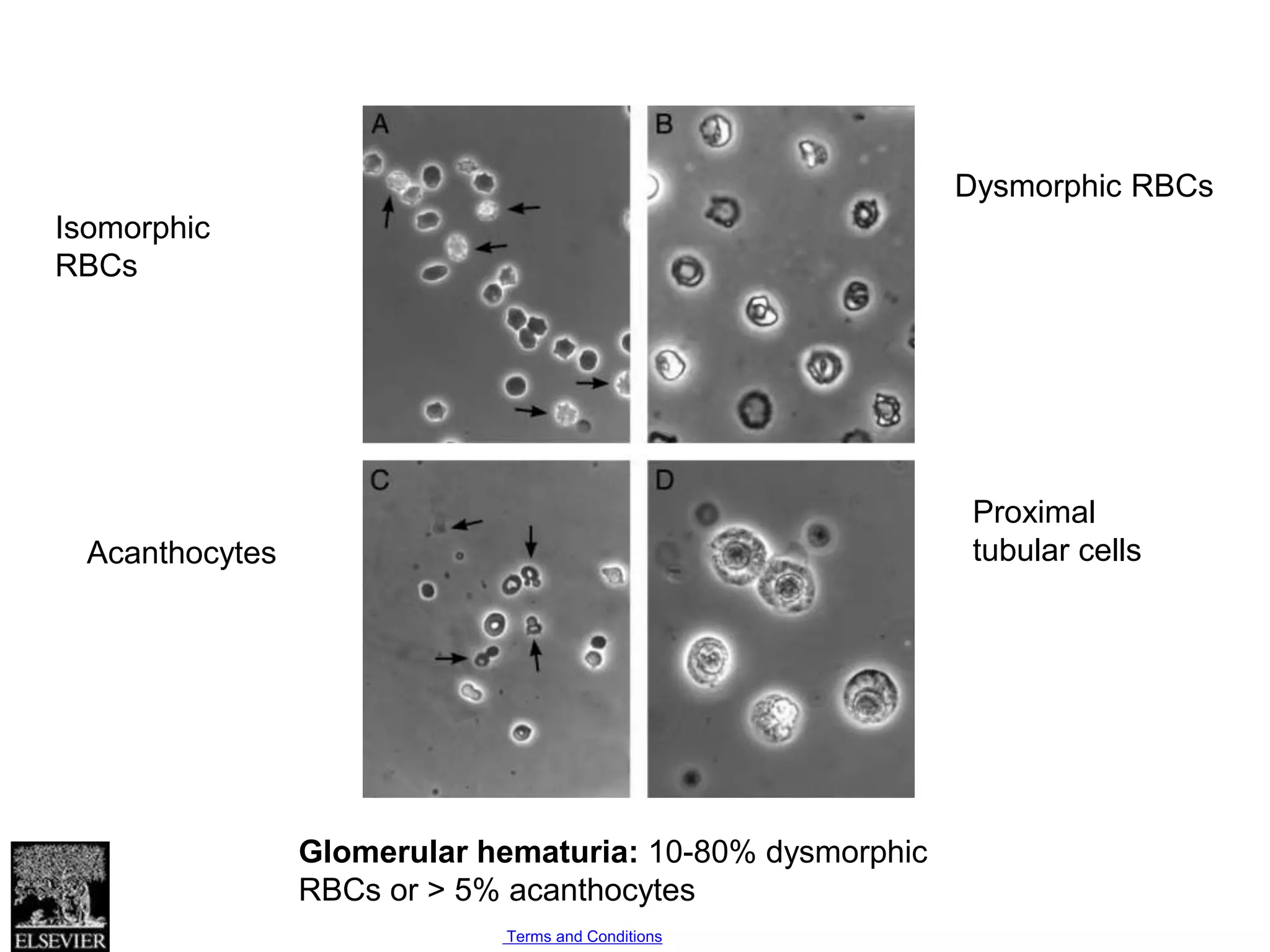
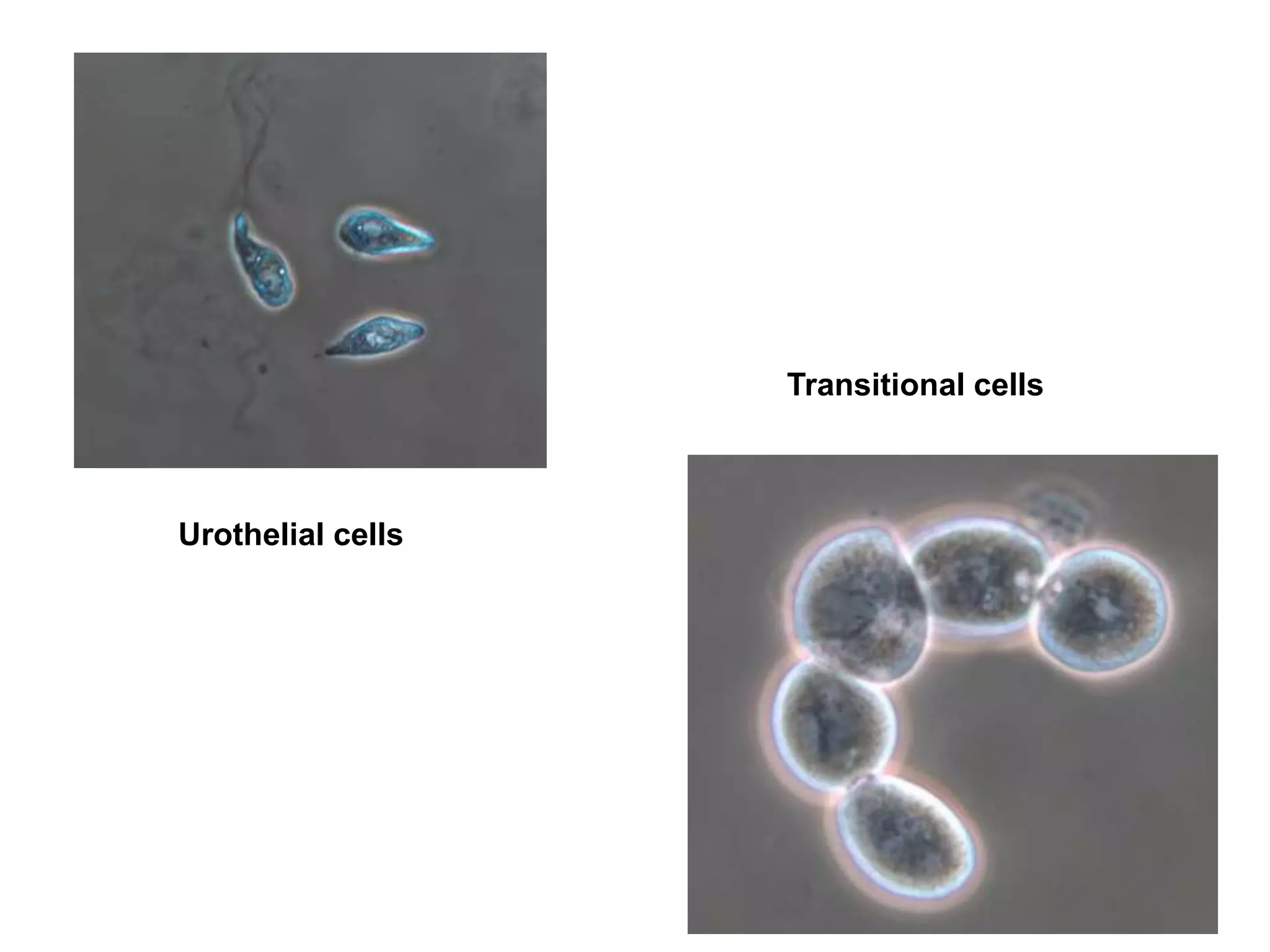
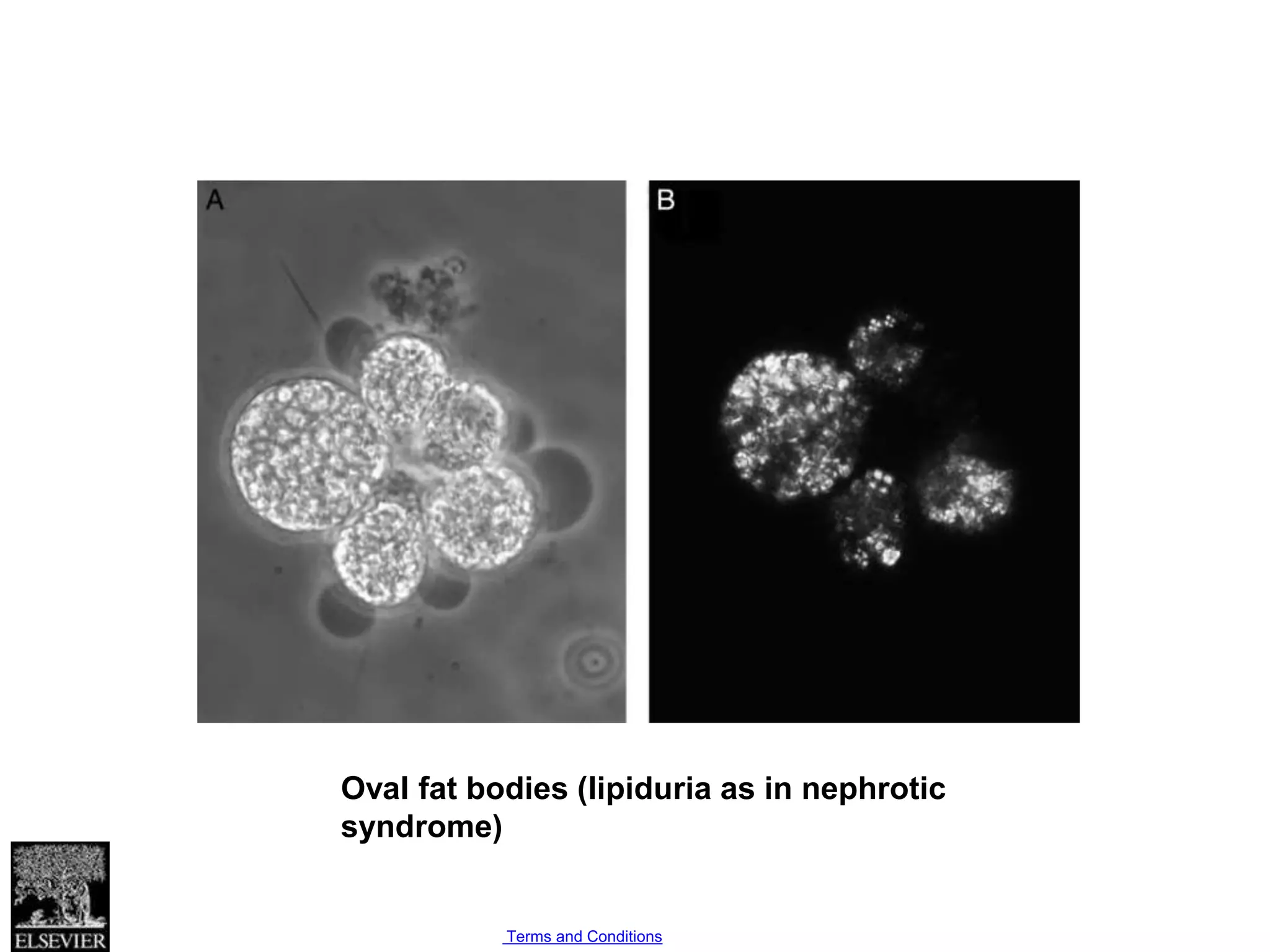
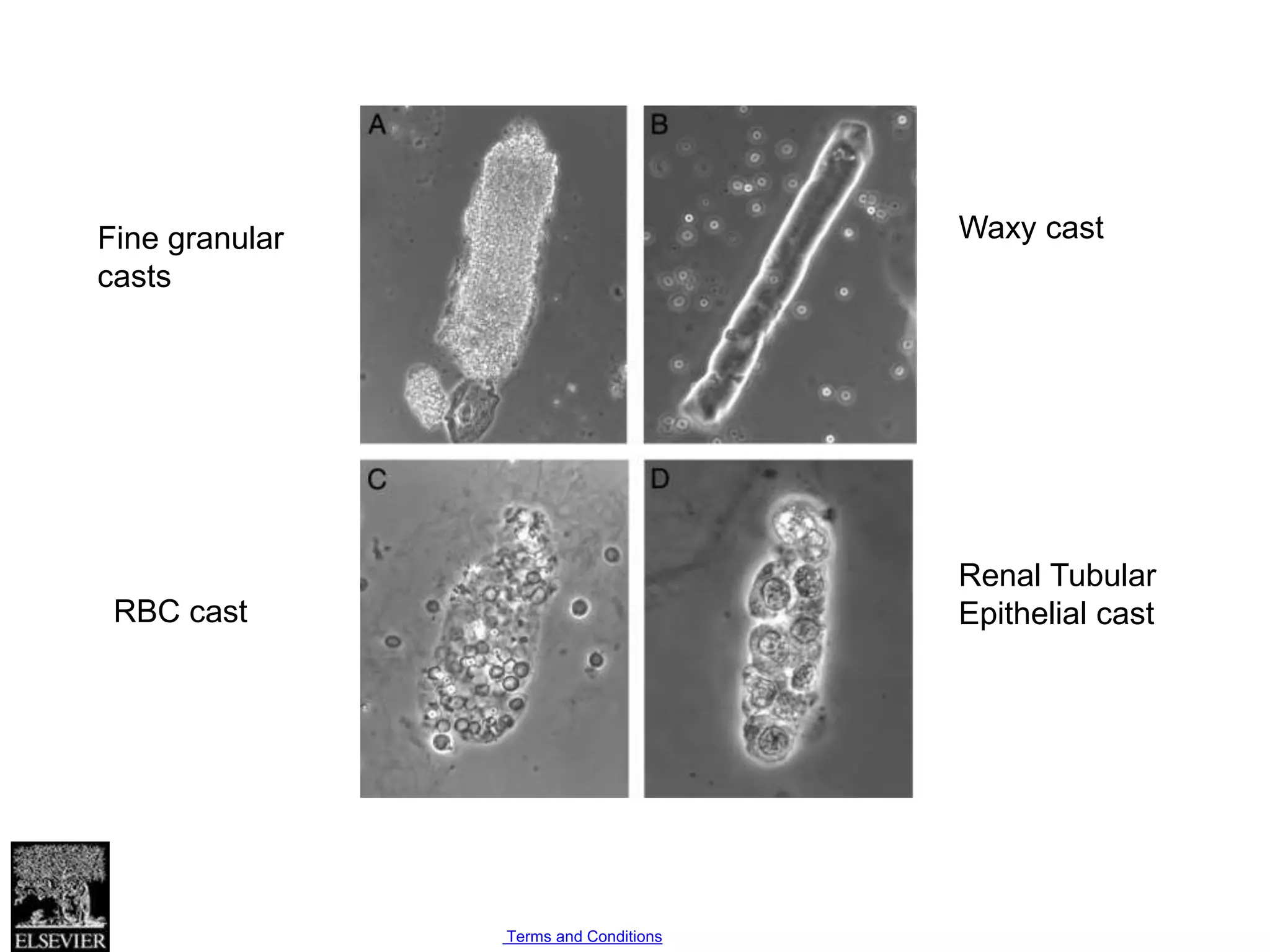
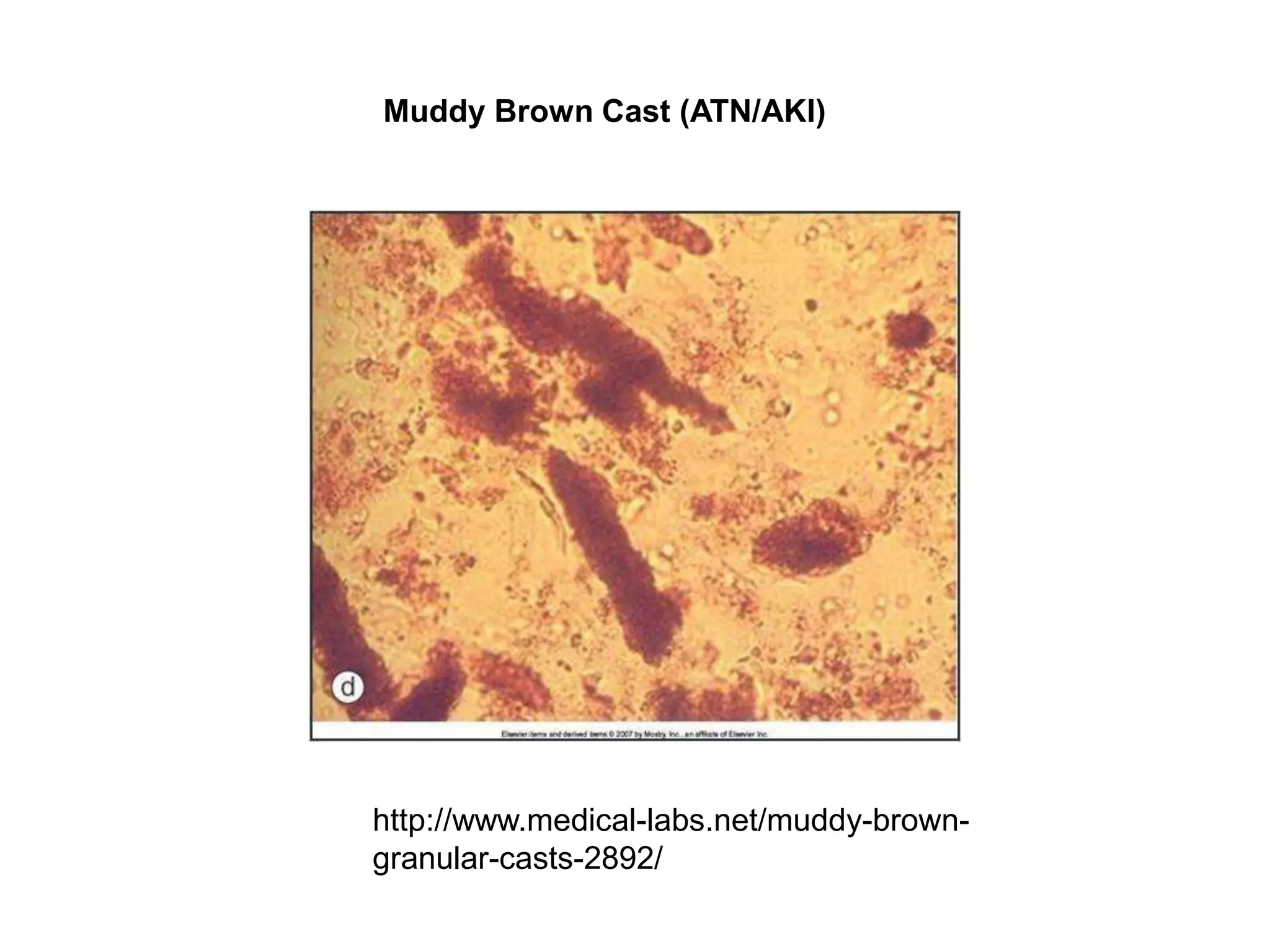
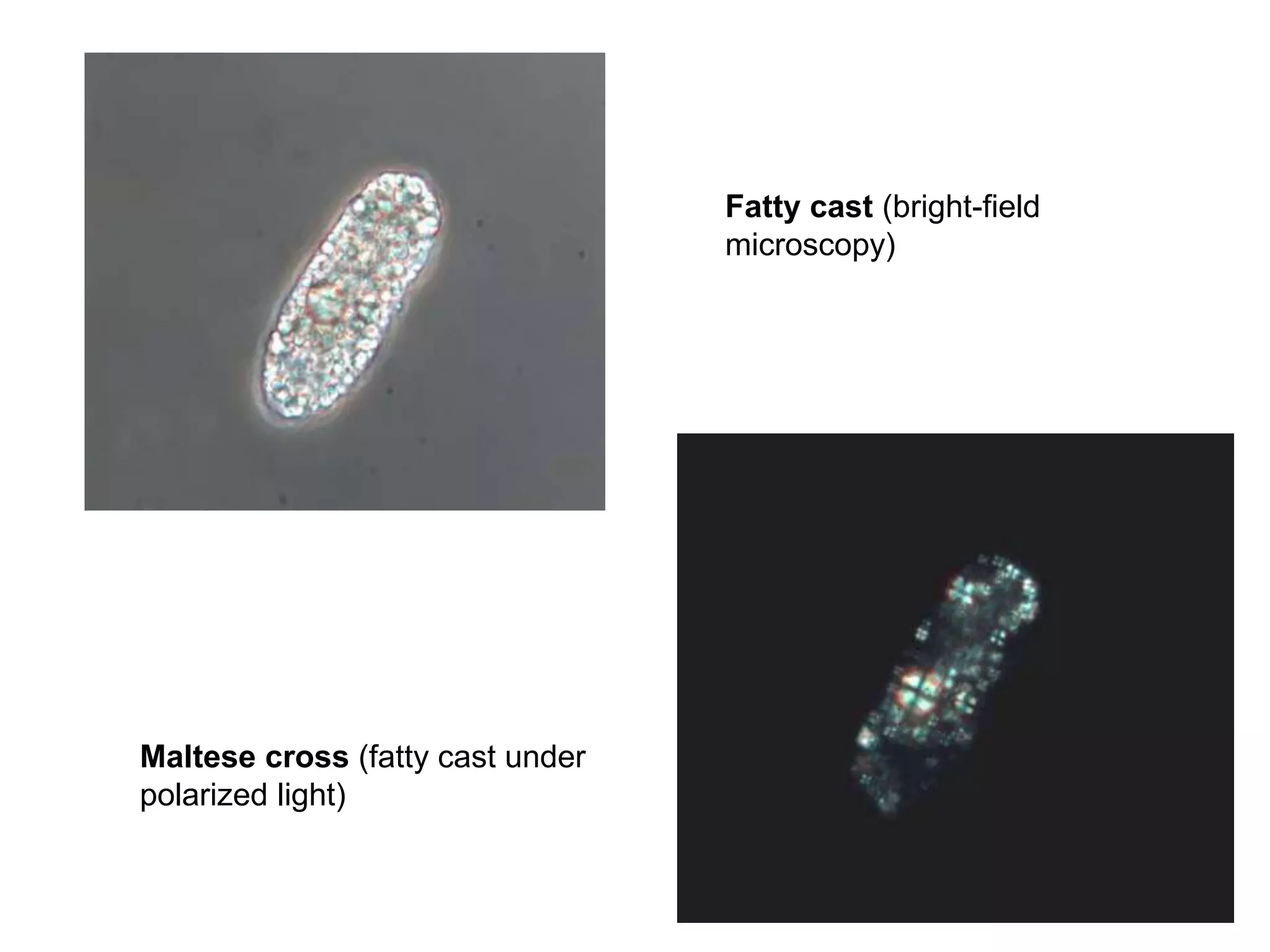
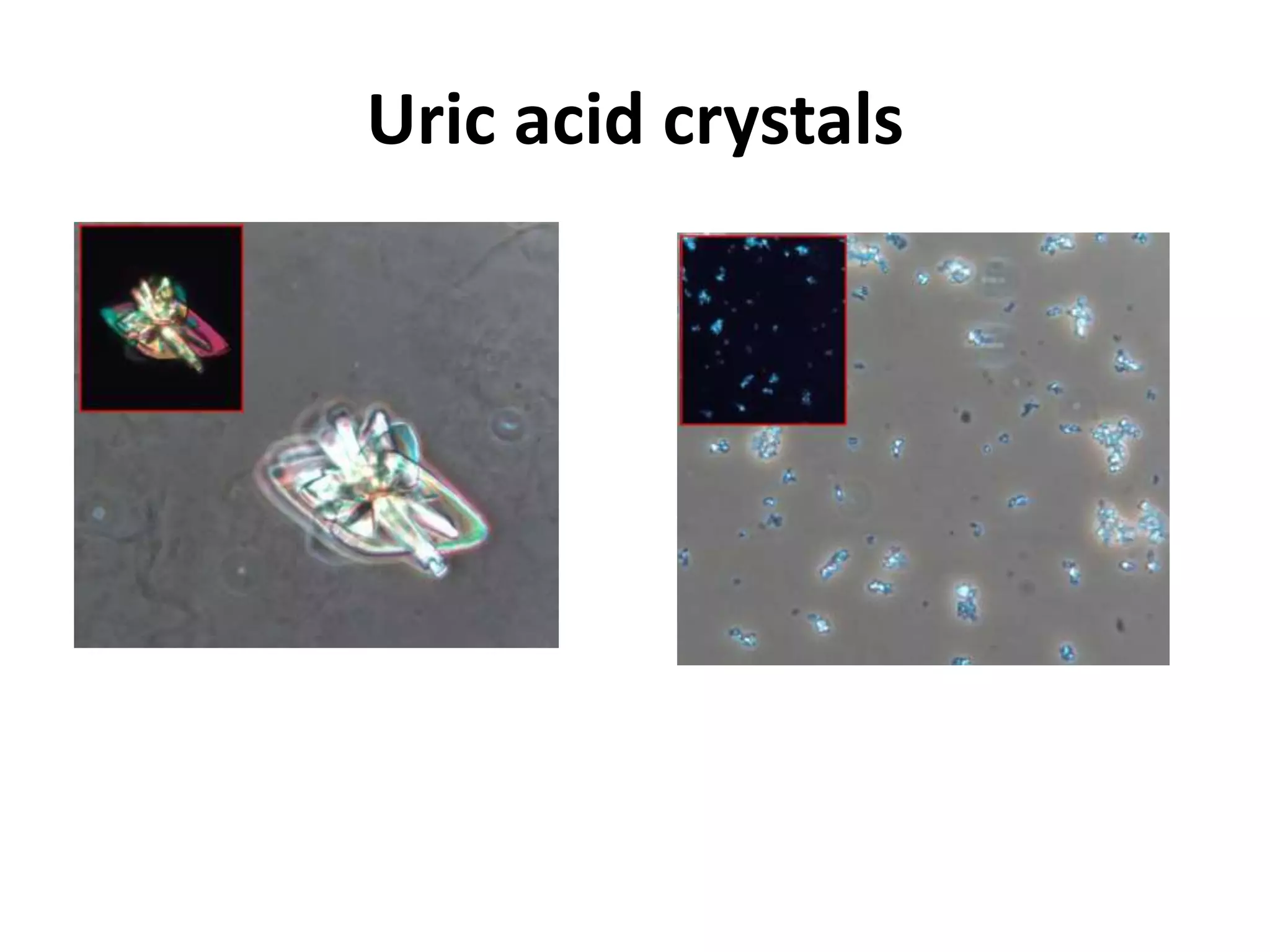
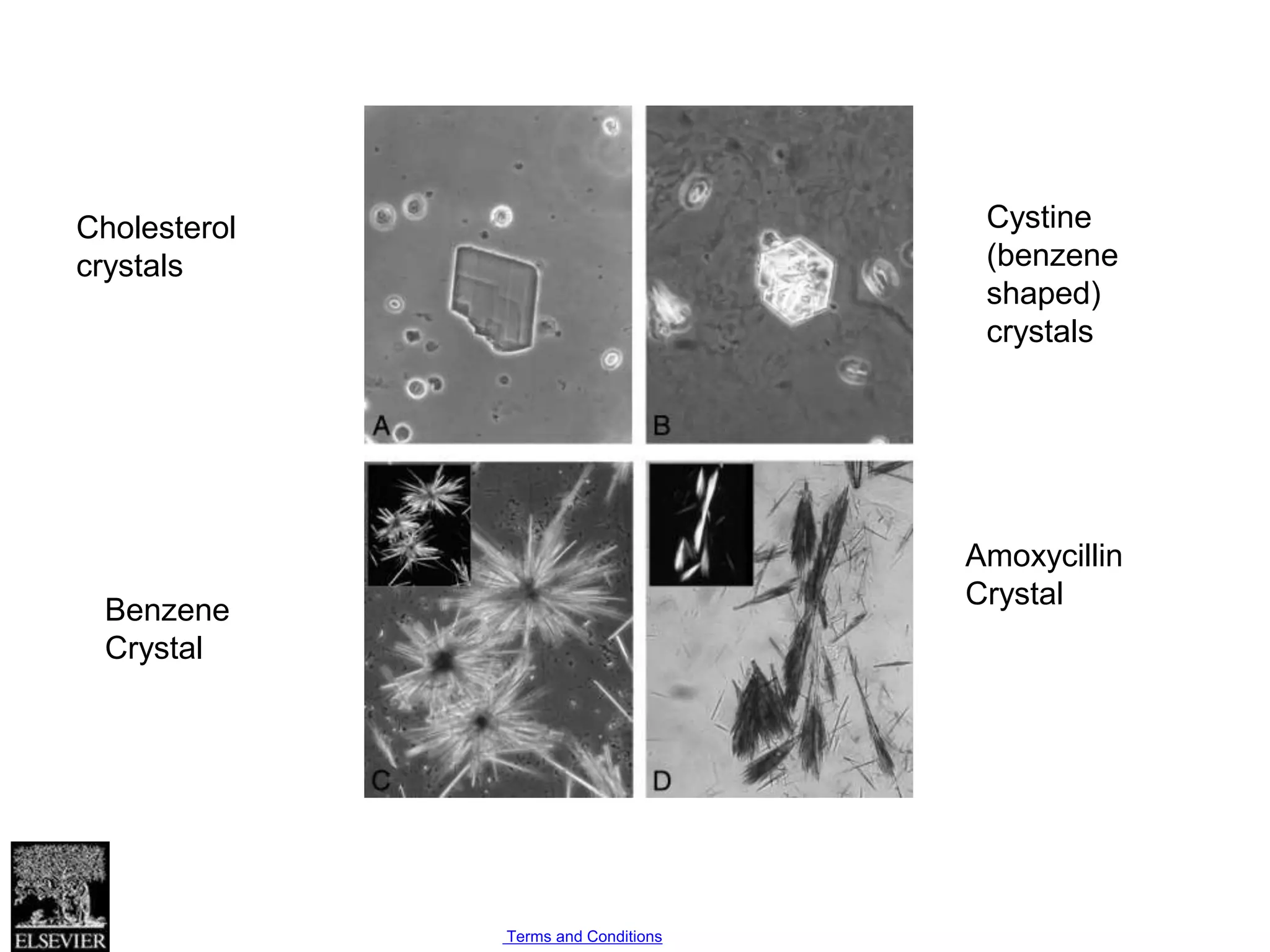
This document provides an overview of urinalysis, including reference values for various analytes, explanations of urine characteristics like color and odor, and descriptions of cells and casts that may be observed in urine microscopy. Key points include normal ranges for urine specific gravity, pH, glucose, proteins, and blood; how urine analyte tests work; causes of abnormal urine colors and odors; and clinical associations of different urine microscopy findings like types of casts and crystals. The goal of urinalysis is to screen for urinary tract infections and kidney diseases.