This document discusses urinalysis and urinary sediment examination. It provides details on:
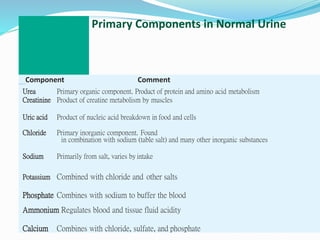
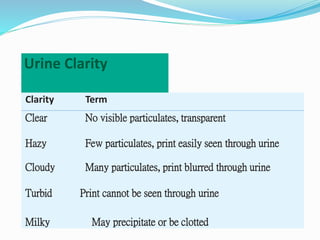
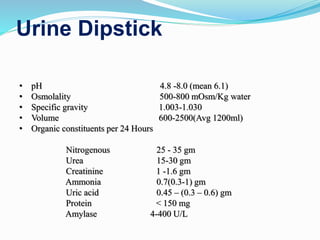
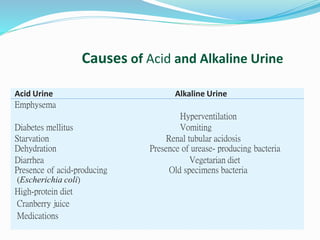
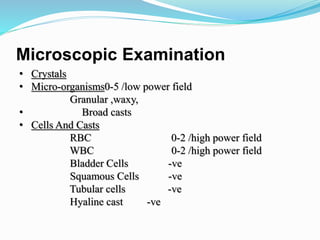
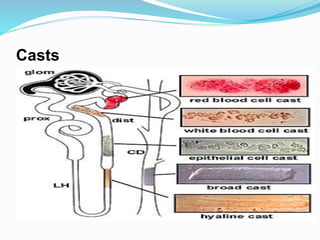
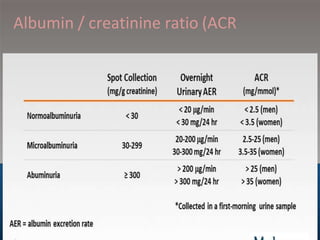
1. The components evaluated in urinalysis including gross evaluation, dipstick analysis, and microscopic examination of urine sediment.
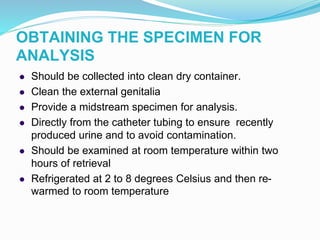
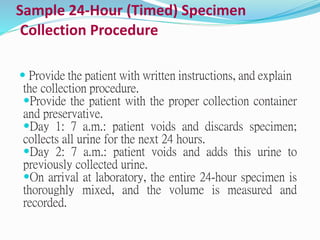
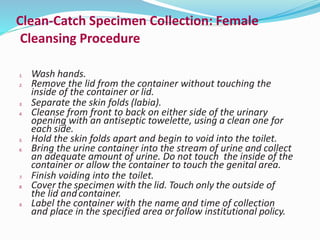
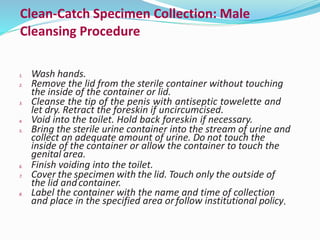
2. Procedures for proper collection and handling of urine samples.
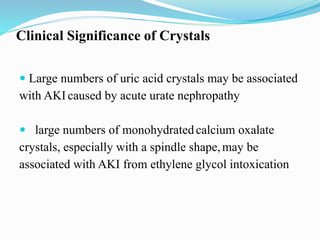
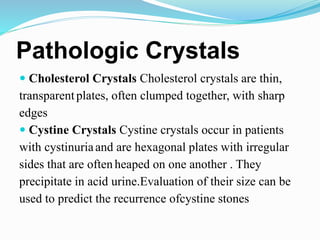
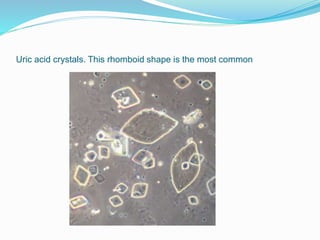
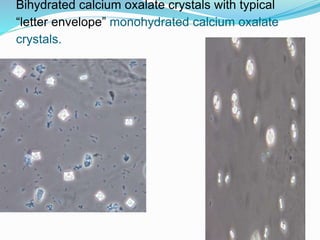
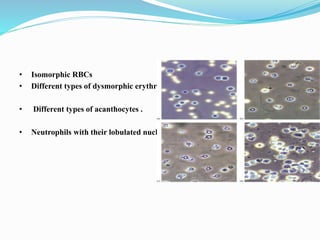
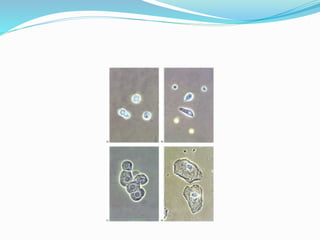
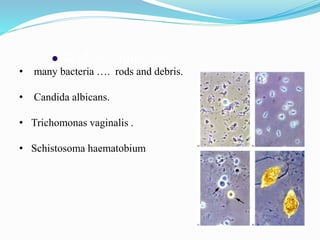
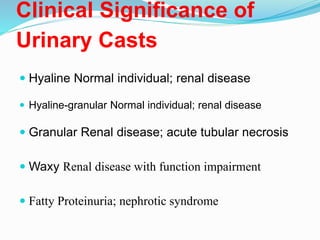
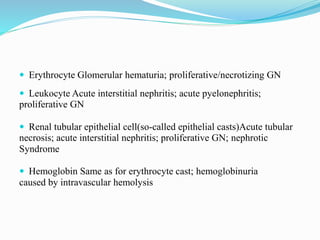
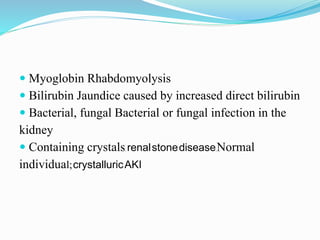
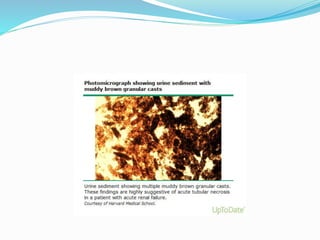
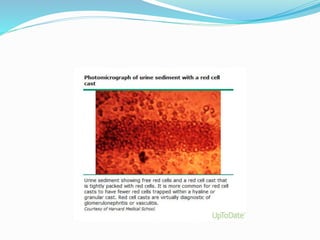
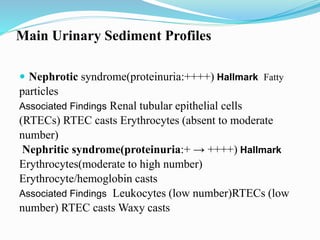
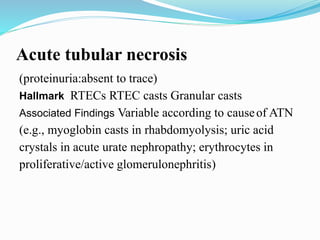
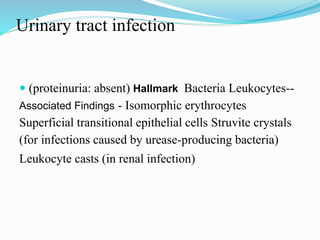
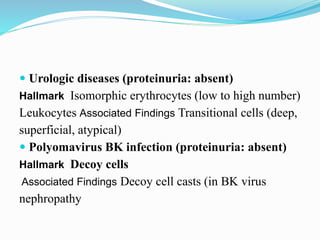
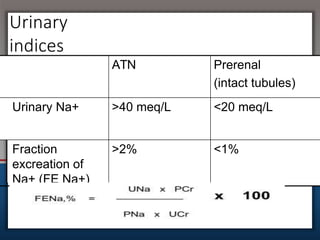
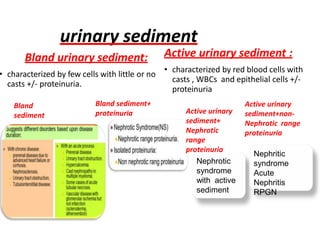
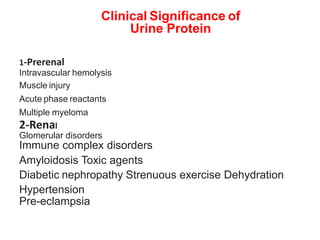
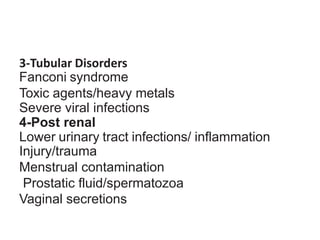
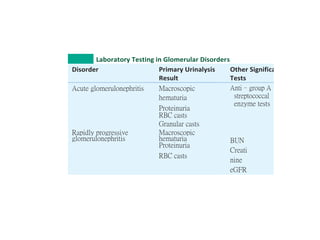
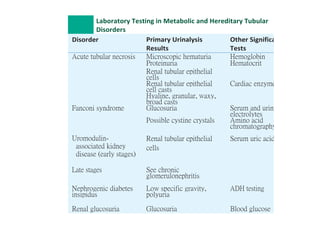
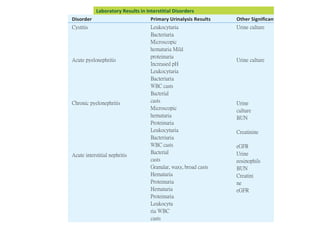
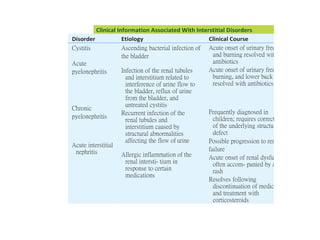
3. The clinical significance of findings from urinary sediment examination such as crystals, cells, casts, and microorganisms.
4. Common urinary sediment profiles associated with kidney diseases including nephrotic syndrome, nephritic syndrome, acute tubular necrosis, and urinary tract infections.