This document discusses urine analysis including urine collection, 24 hour urine samples, specimen preservation, and urine examination. Key points include:
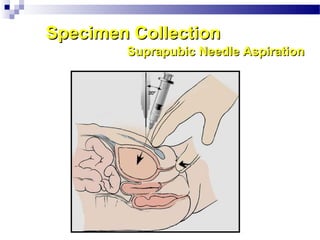
- Urine is formed in the kidneys and various samples can be collected including early morning, random, 24 hour, and catheterized samples.
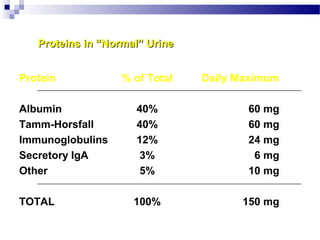
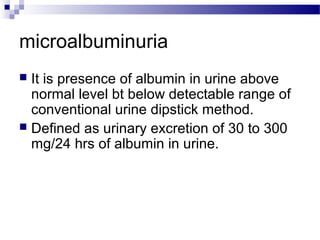
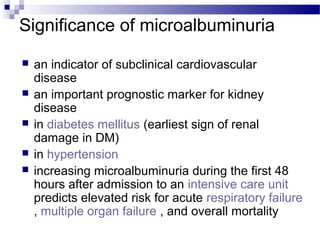
- 24 hour urine samples are used to quantitatively estimate proteins, hormones, microalbumin, and metabolites.
- Preservatives like HCl, toluene, and boric acid can be used but may interfere with tests. Samples should be examined within 1-2 hours.
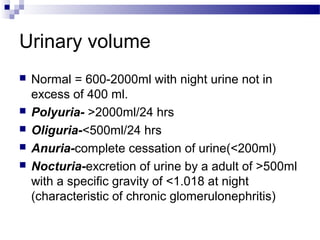
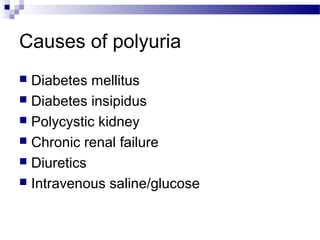
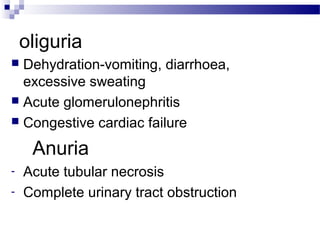
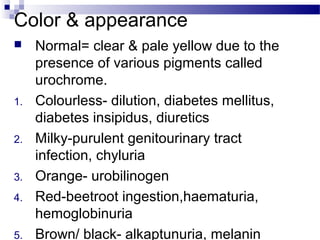
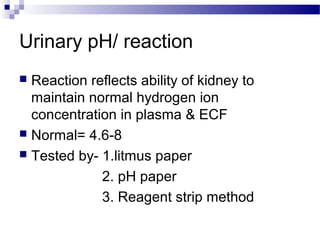
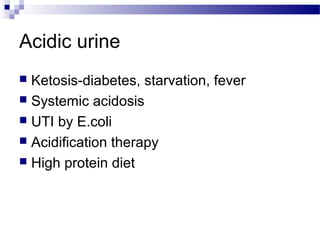
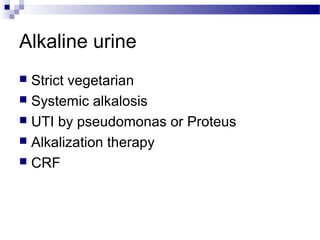
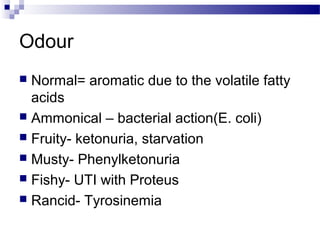
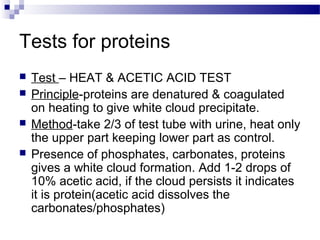
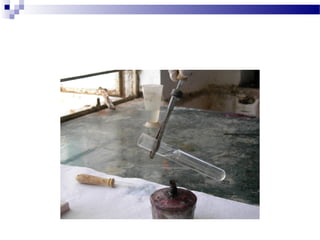
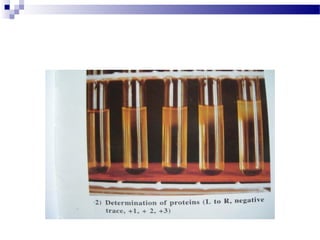
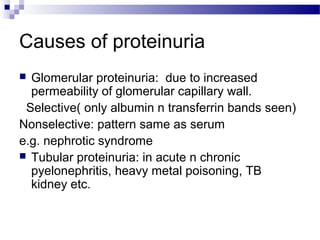
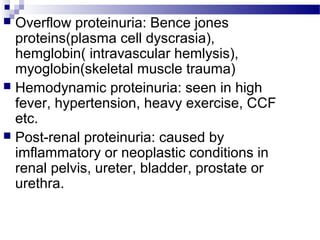
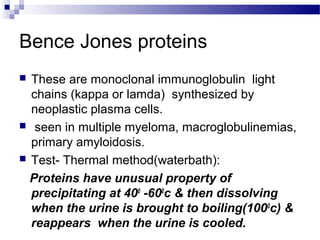
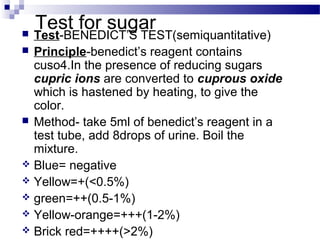
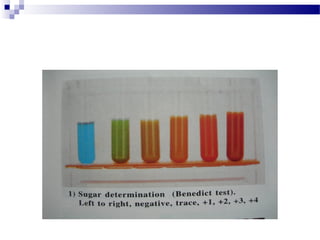
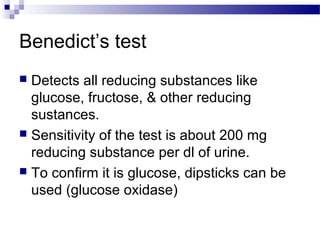
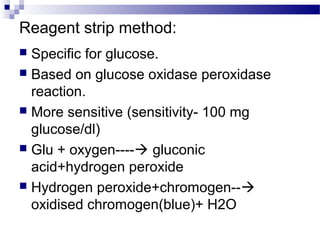
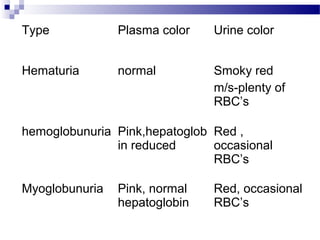
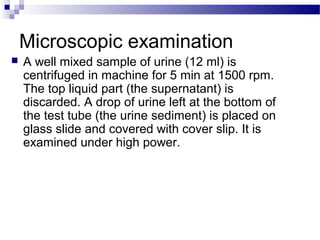
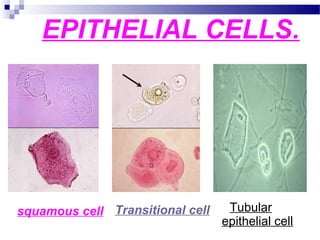
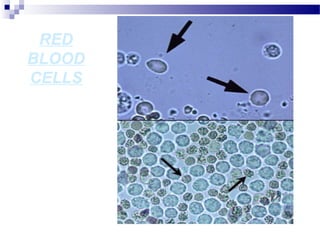
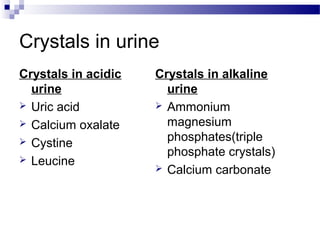
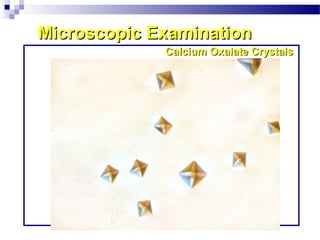
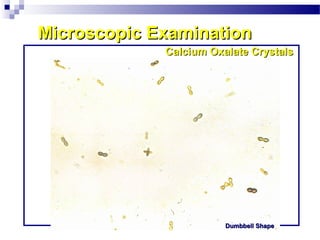
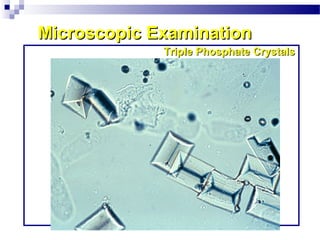
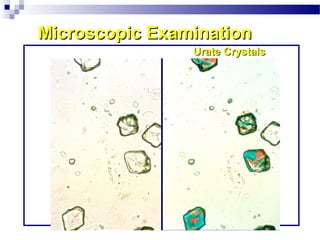
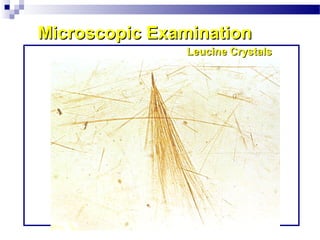
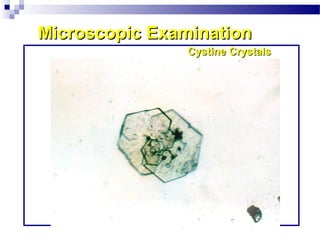
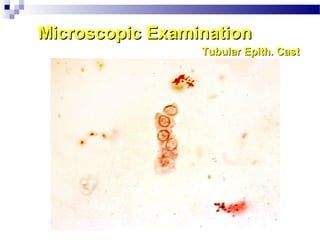
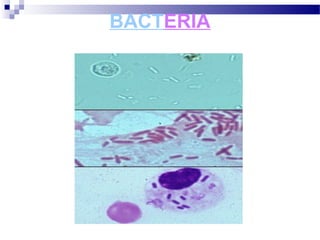
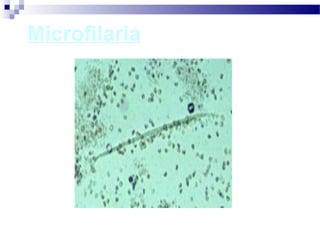
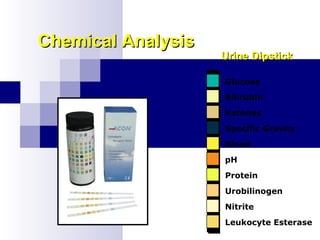
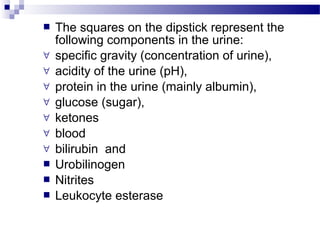
- Urine examination includes macroscopic tests of volume, color, odor, pH; microscopic tests; and chemical tests for proteins, sugars