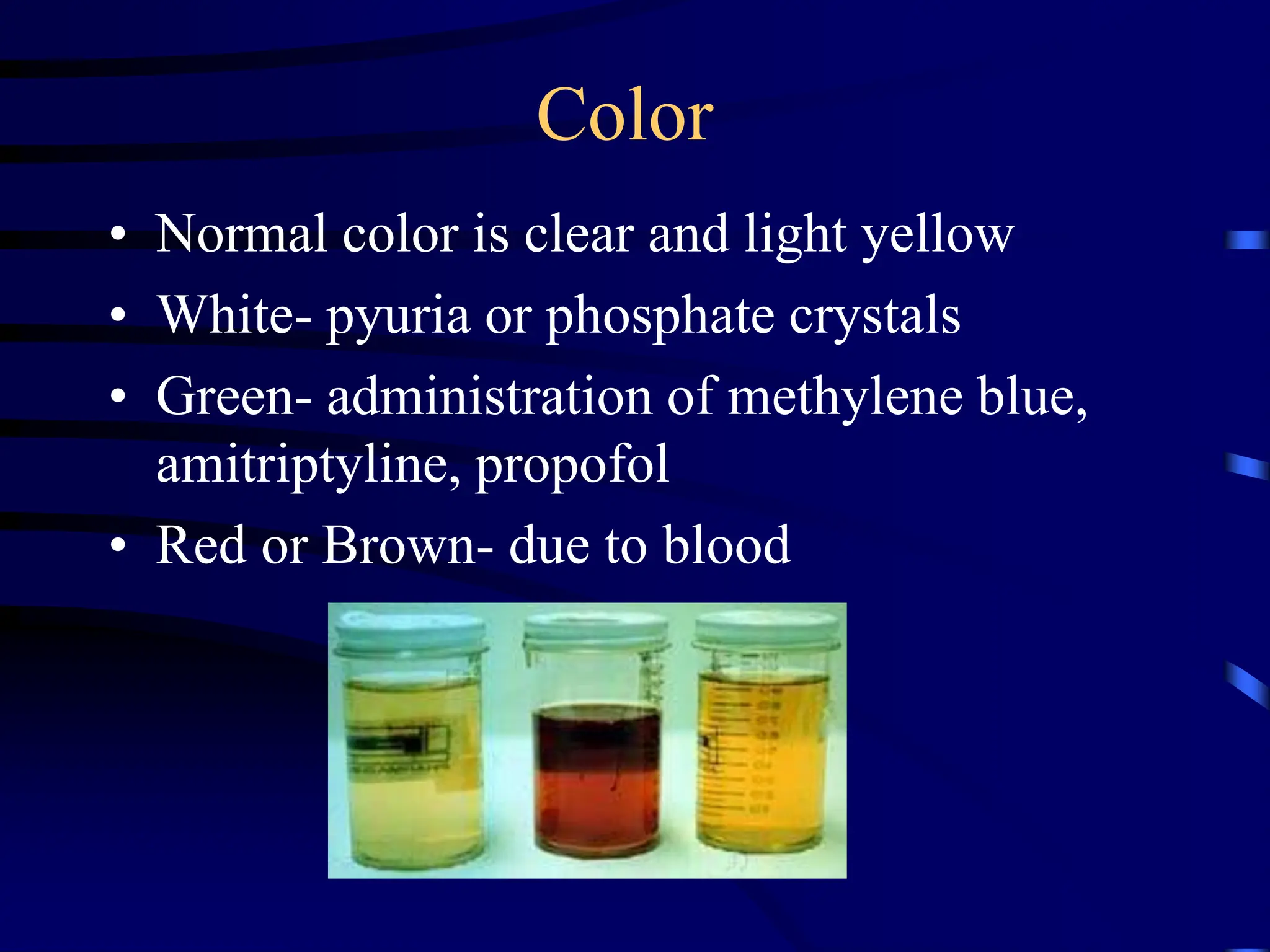
This document provides an overview of urinalysis including the normal appearance and clinical significance of various findings on a urine dipstick test and urine sediment examination. Key points include that urinalysis is a major noninvasive tool that can provide information about disease severity though not always a direct relationship, and specimens should be examined 30-60 minutes after voiding. Abnormal findings on urinalysis can indicate conditions like urinary tract infection, kidney disease, liver dysfunction, and diabetes.