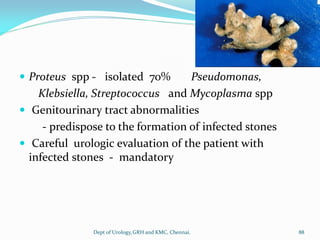
The document provides information about the Department of Urology at Govt Royapettah Hospital and Kilpauk Medical College in Chennai, India. It lists the professors and assistant professors in the department and provides details about the prevalence, clinical presentation, evaluation, management and treatment of kidney stones in children. It discusses various treatment options for kidney stones like conservative management, SWL, URS, PCNL and treatments for vesical calculi. It also describes complications related to different surgical procedures.