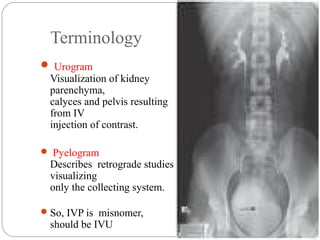
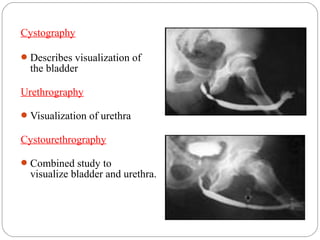
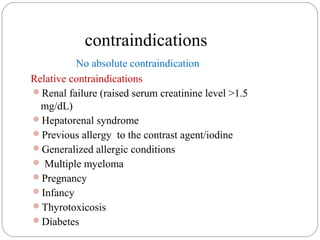
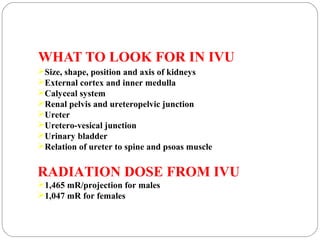
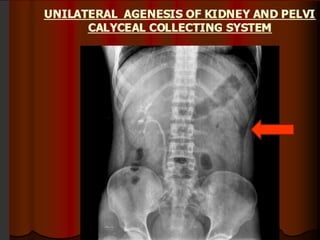
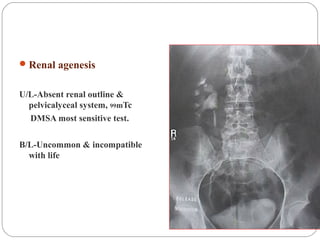
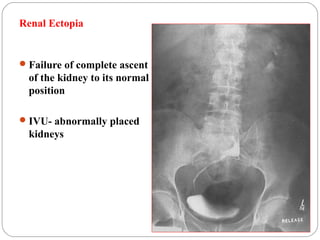
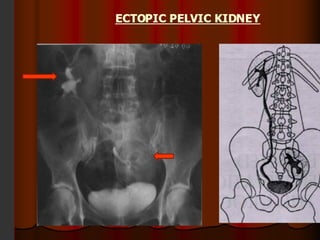
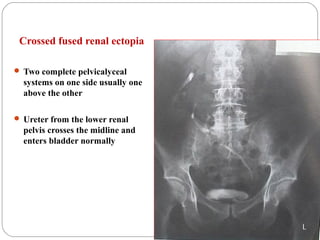
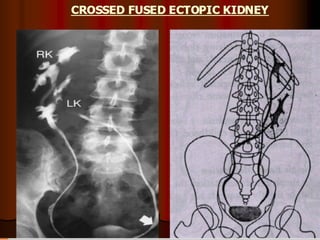
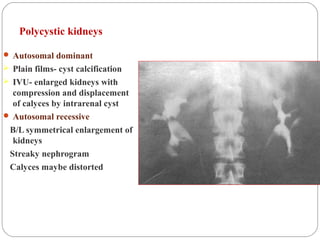
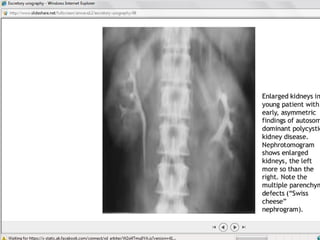
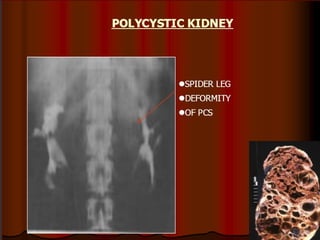
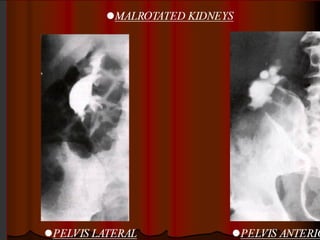
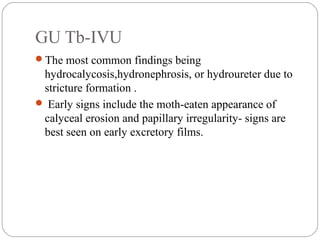
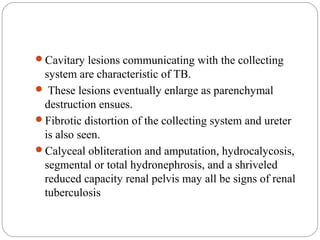
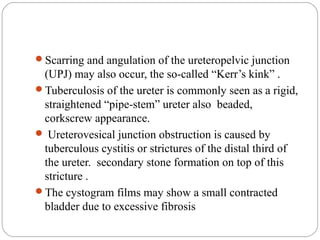
The document discusses intravenous urography (IVU), including its definition, history, indications, contraindications, technique, and what to look for in the images. Some key points:
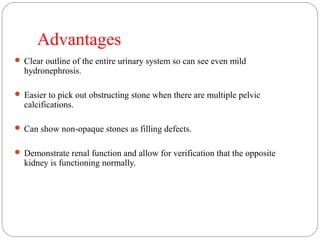
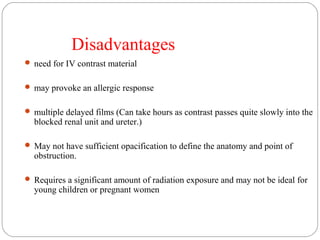
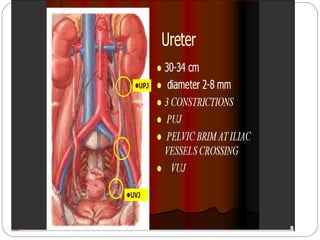
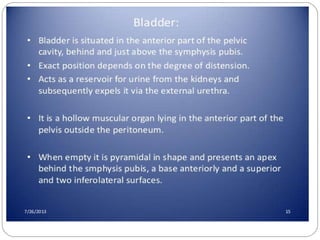
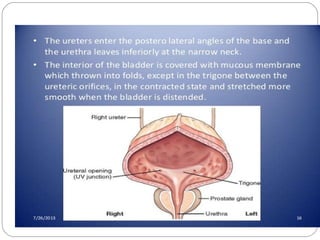
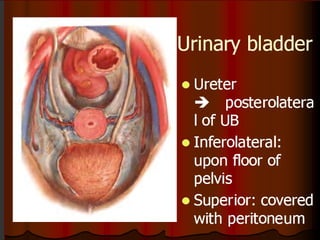
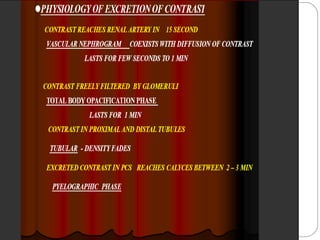
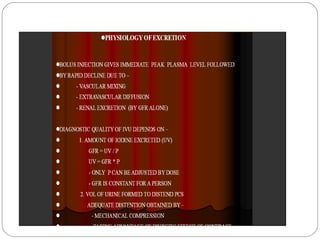
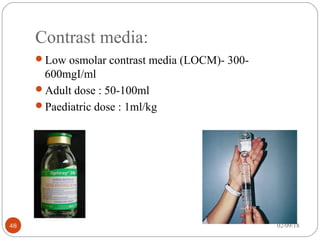
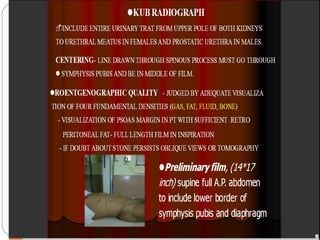
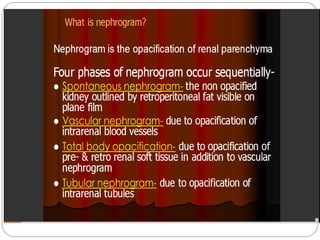
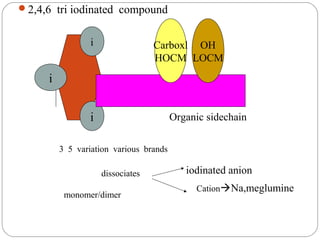
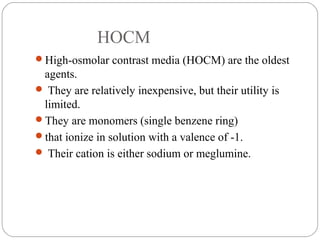
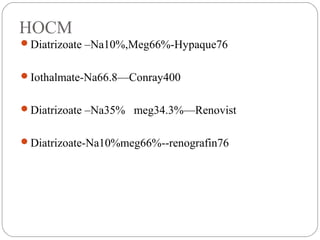
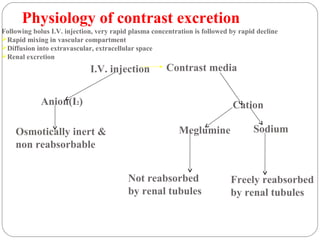
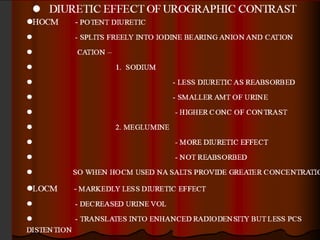
- IVU involves injecting contrast media intravenously and imaging the urinary tract, allowing visualization of the kidneys, ureters, and bladder.
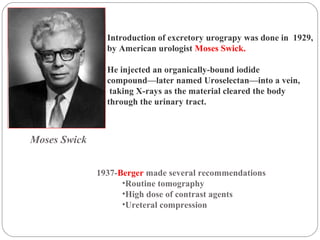
- It was introduced in 1929 but use has declined with the rise of CT, ultrasound and MRI. However, it remains useful for visualizing the pelvicalyceal system.
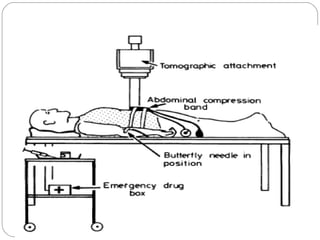
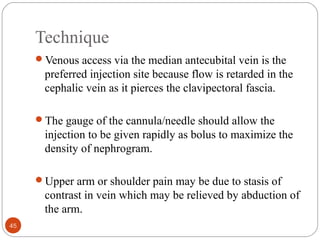
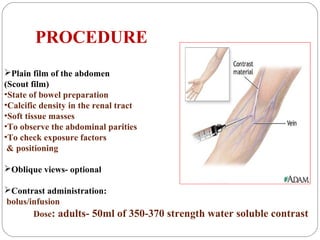
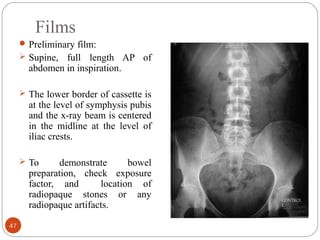
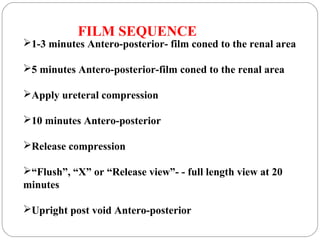
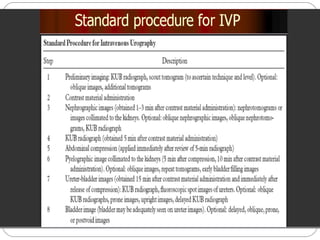
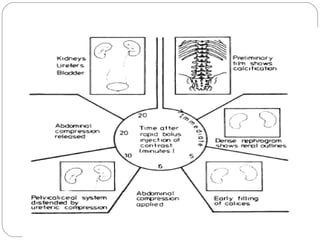
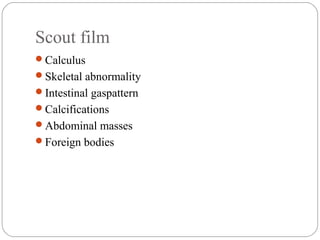
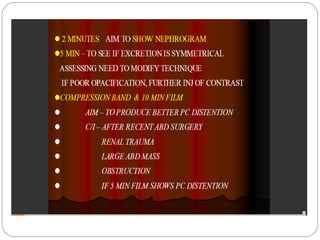
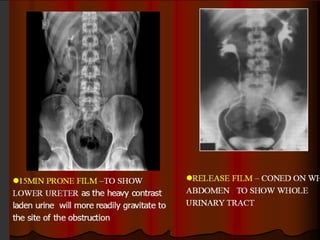
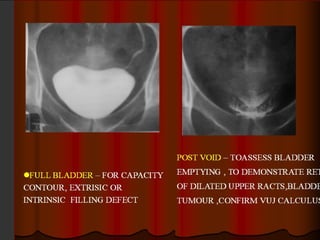
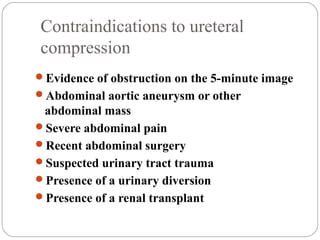
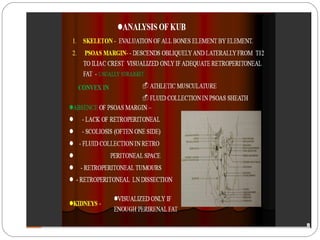
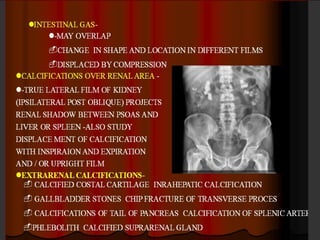
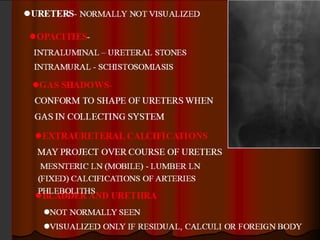
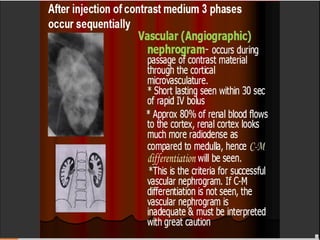
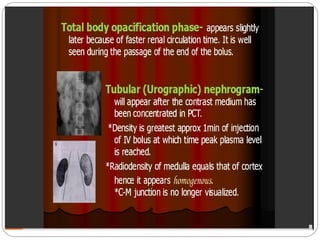
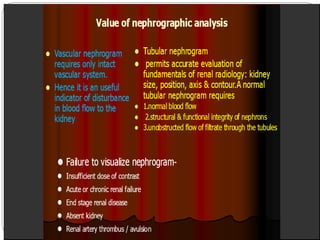
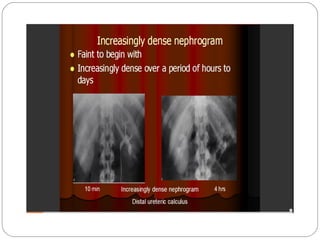
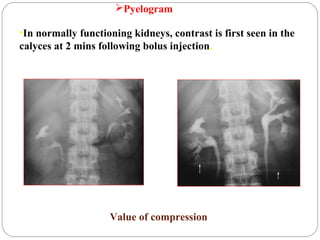
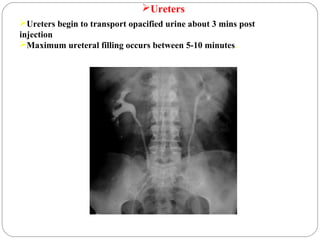
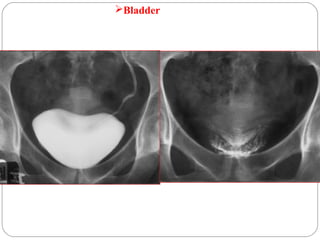
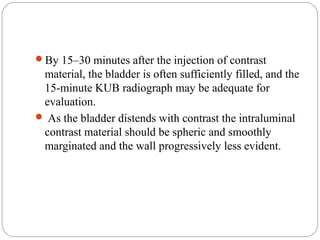
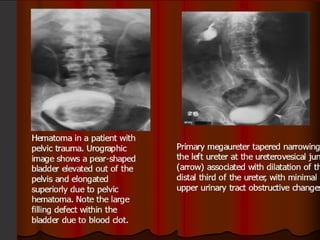
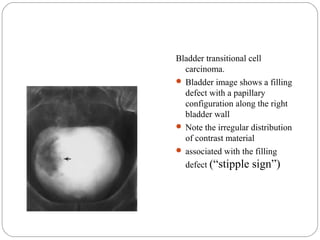
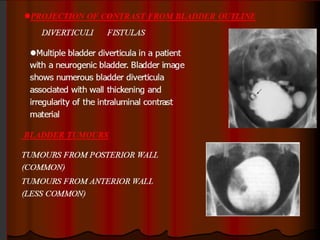
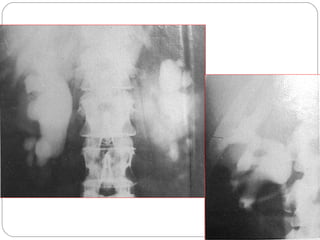
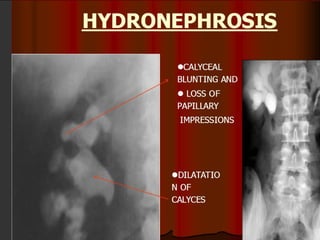
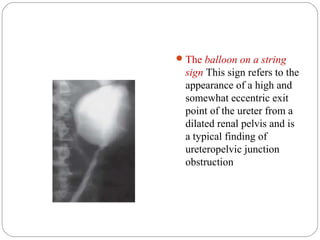
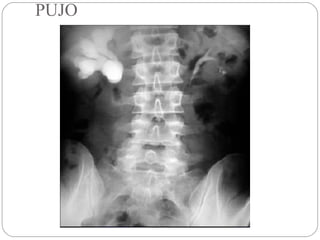
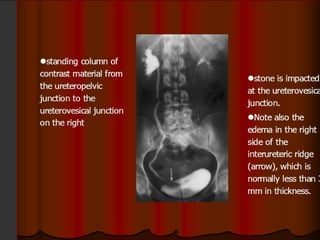
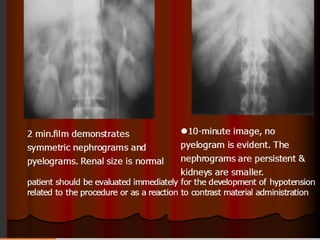
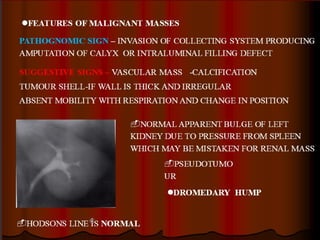
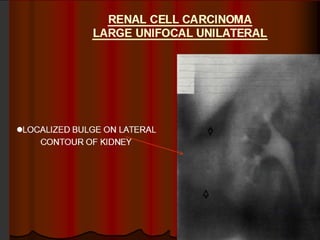
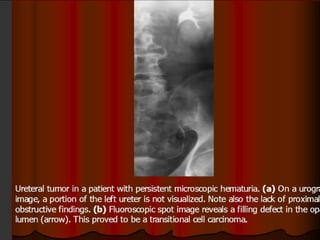
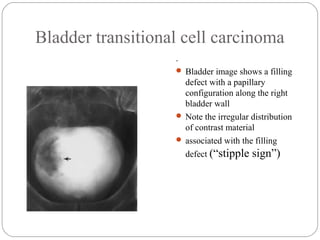
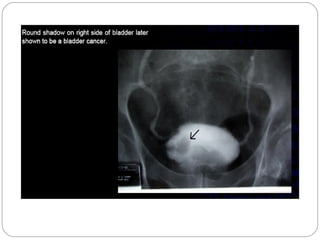
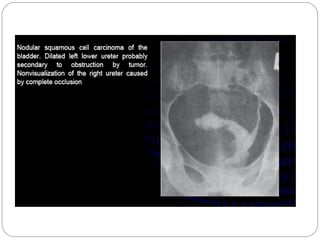
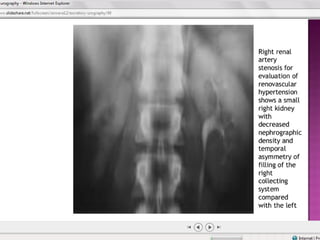
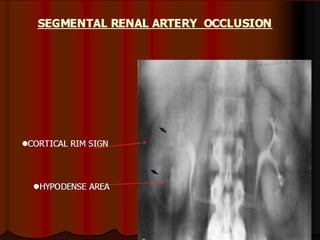
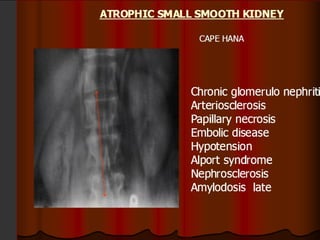
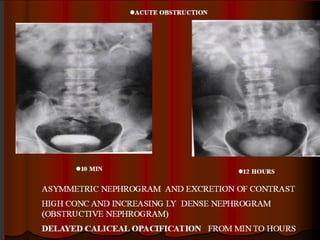
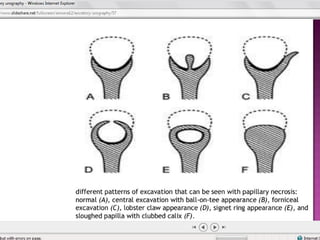
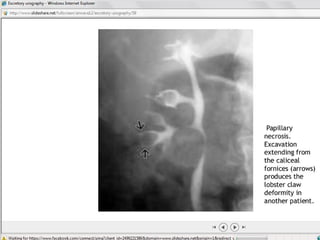
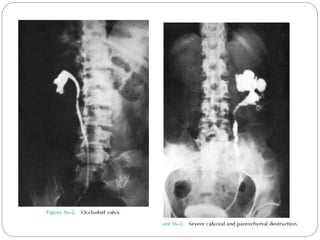
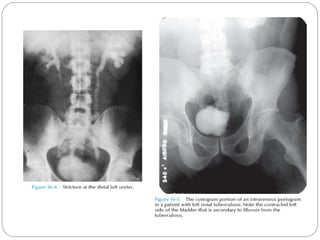
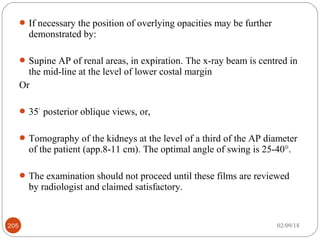
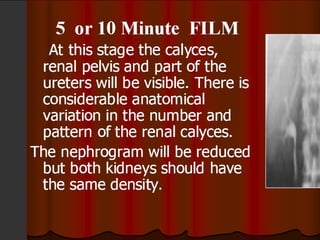
- The procedure involves obtaining baseline images, injecting contrast, then timed imaging as the contrast passes through the urinary system, sometimes using compression. Findings are assessed for