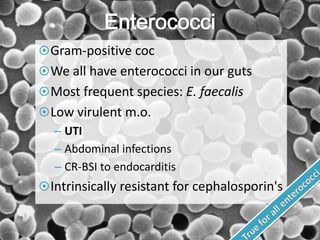
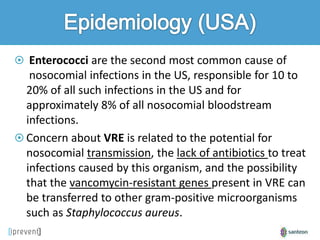
This document discusses Enterococcus faecium and vancomycin-resistant Enterococcus (VRE). It notes that E. faecium is becoming more prevalent than E. faecalis in nosocomial infections. VRE can transmit between patients in healthcare settings and there is concern about a lack of antibiotic options to treat VRE infections. Controlling VRE outbreaks requires strict infection control measures like contact isolation, hand hygiene, and thorough environmental cleaning. Antibiotic use, especially broad-spectrum antibiotics, is an important factor in the selection and transmission of VRE.