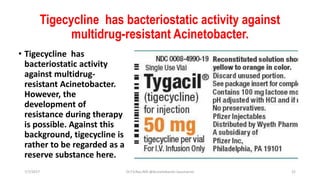
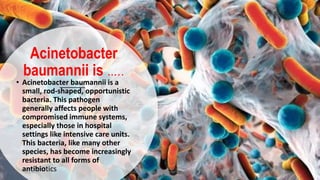
Acinetobacter baumannii is a bacteria that has become increasingly drug-resistant and causes a variety of infections, especially in hospital settings. It emerged as a significant pathogen among soldiers during the Iraq war. Identification requires specialized laboratory techniques, but molecular testing provides the most accurate identification. Treatment options are limited due to high resistance rates, but carbapenems and sulbactam are still used. Preventing transmission relies on good hand hygiene and environmental cleaning.





![Acinetobacter Baumannii therapy
• The agent of choice are carbapenems [imipenem
(ZIENAM), meropenem (MERONEM)] is recommended.
However, differences in sensitivity may exist with respect
to the two substances, ie with proven sensitivity to
imipenem may not be automatically inferred on sensitivity
to meropenem and vice versa. As a further treatment
option has recently become doripenem are available.
However, the frequency of resistance to carbapenems in
recent years has increased significantly worldwide.
7/7/2017 Dr.T.V.Rao MD @Acinetobacter baumannii 20](https://image.slidesharecdn.com/acinetobacterbaumannii-170707144430/85/Acinetobacter-baumannii-an-update-20-320.jpg)