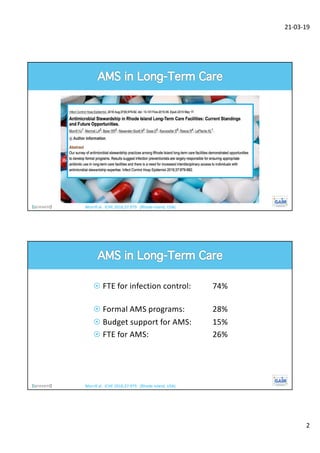
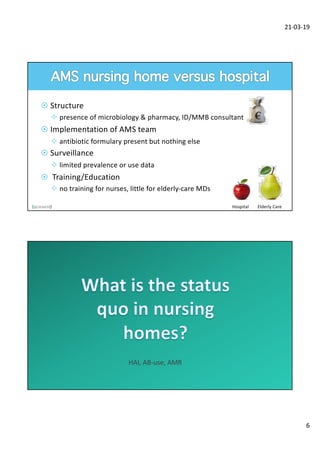
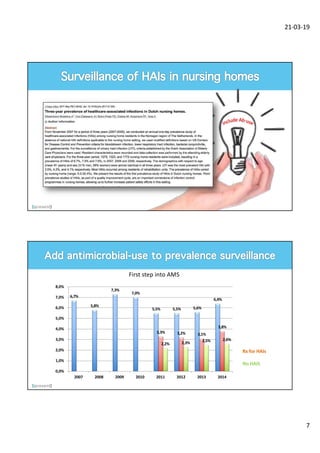
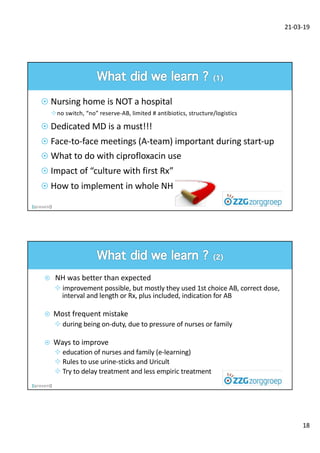
This document summarizes work done to implement antibiotic stewardship (AMS) programs in nursing homes in the Netherlands. It finds that while AMS is established in hospitals, it is unknown in nursing homes. It discusses adapting hospital AMS guidelines for nursing homes and the unique needs of nursing homes, including limited resources and staff training. It also reports on establishing an AMS team, monitoring antibiotic use data, providing education to nurses and families, and finding room for improvement, particularly around urinary tract infections. The overall inappropriate antibiotic use for UTIs in nursing homes was found to be 32%.