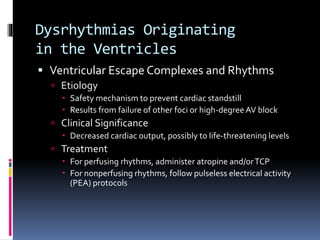
This document discusses various dysrhythmias originating in the ventricles, including ventricular escape complexes/rhythms, accelerated idioventricular rhythm, premature ventricular contractions, ventricular tachycardia, torsades de pointes, ventricular fibrillation, asystole, and artificial pacemaker rhythm. For each dysrhythmia, the etiology, clinical significance, and treatment approach are summarized.