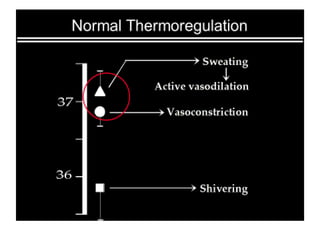
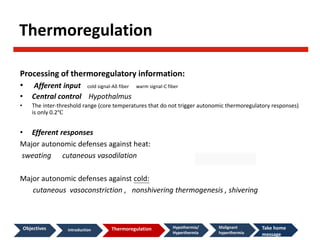
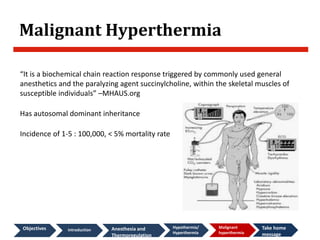
This document discusses temperature regulation and its implications for anesthesia. It begins by introducing concepts like hypothermia, hyperthermia, and methods of measuring core body temperature. It then explains how anesthesia disrupts the body's natural thermoregulation processes, causing patients to become poikilothermic (temperature dependent on environment). Under anesthesia, core temperature declines in three phases - an initial rapid redistribution phase, followed by a slow linear reduction phase, and finally reaching a thermal plateau. The document also discusses complications of unintentional hypothermia, as well as malignant hyperthermia which is an acute, potentially fatal reaction to certain anesthetic gases and succinylcholine in susceptible individuals.