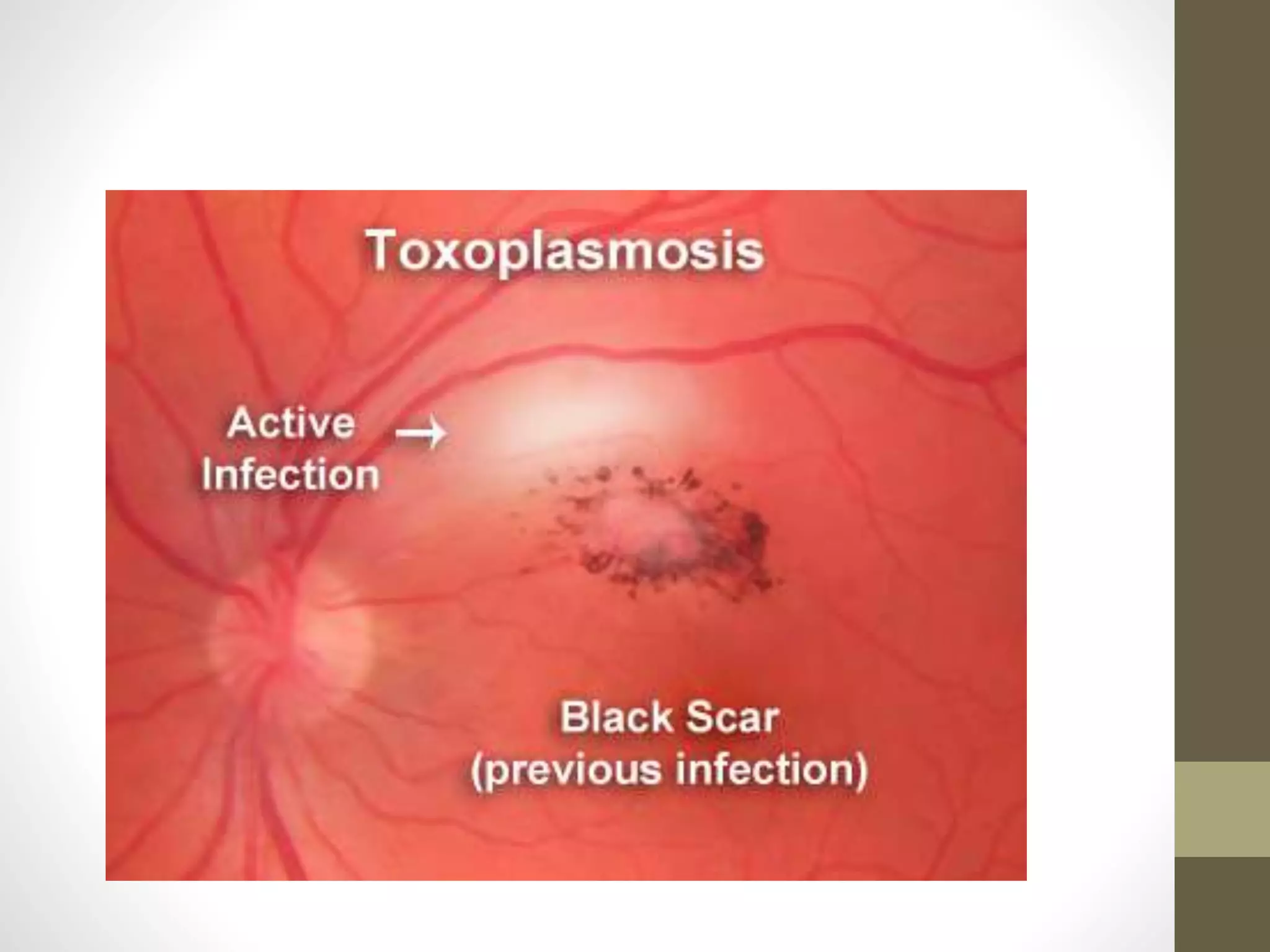
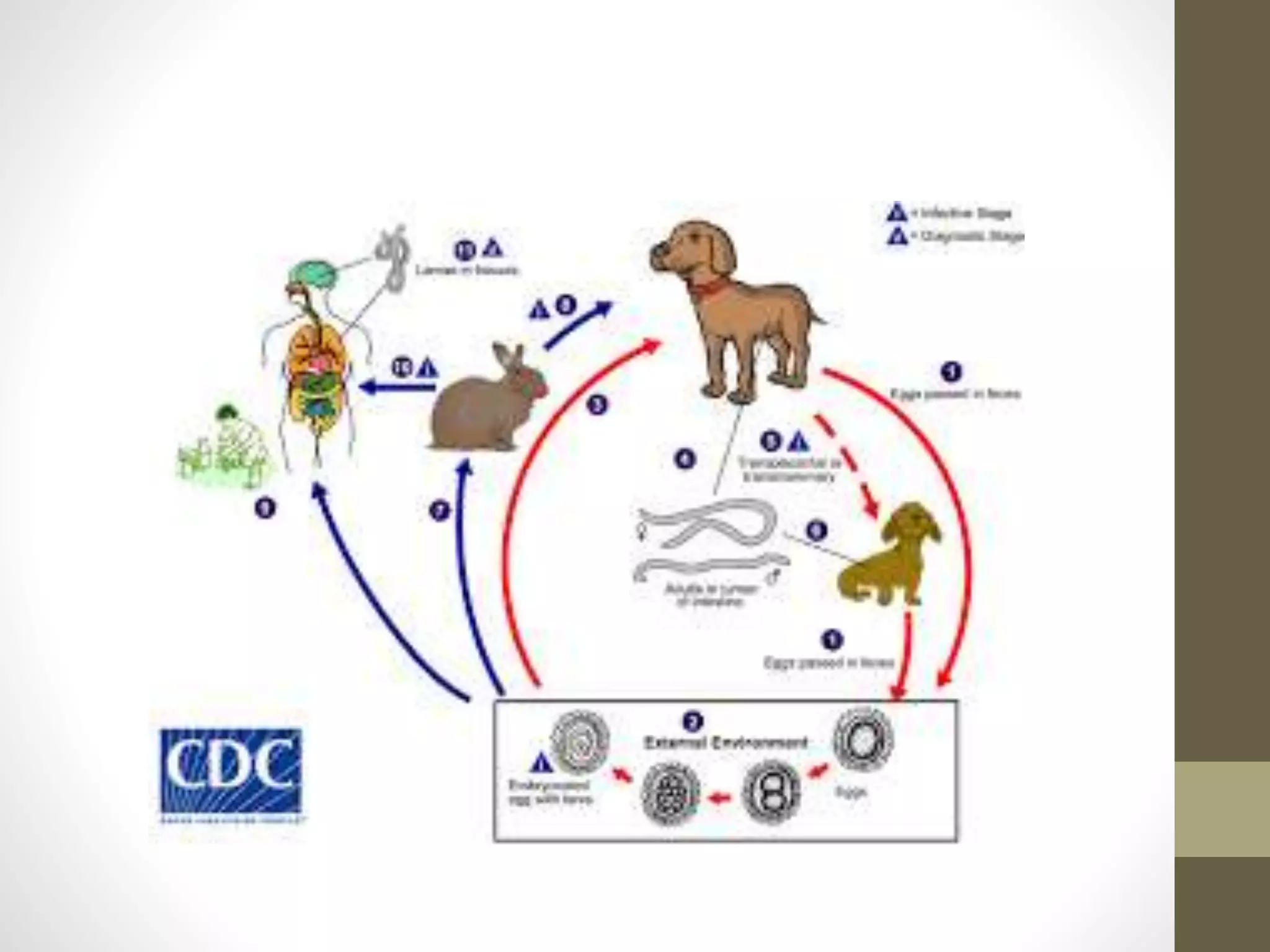
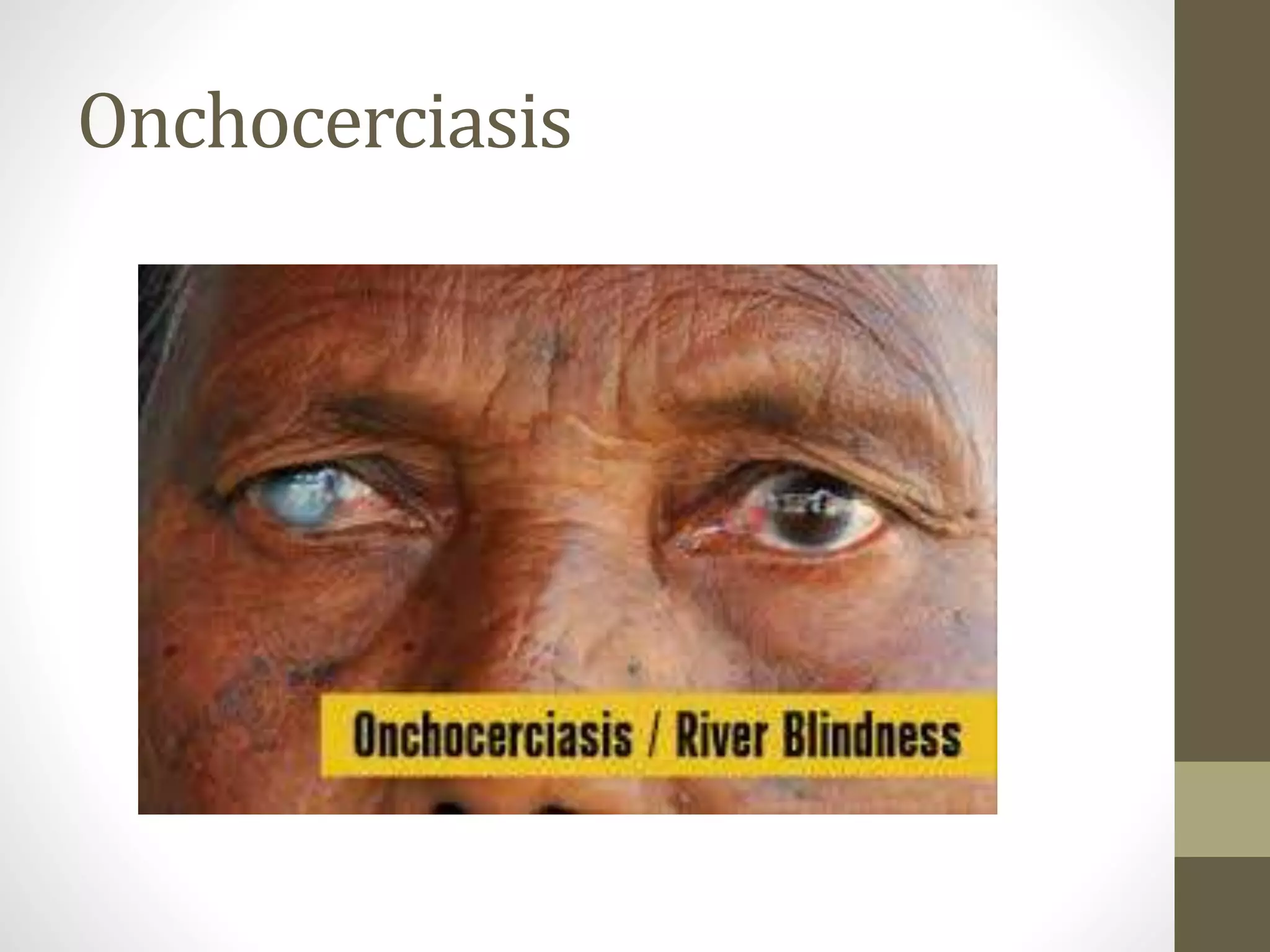
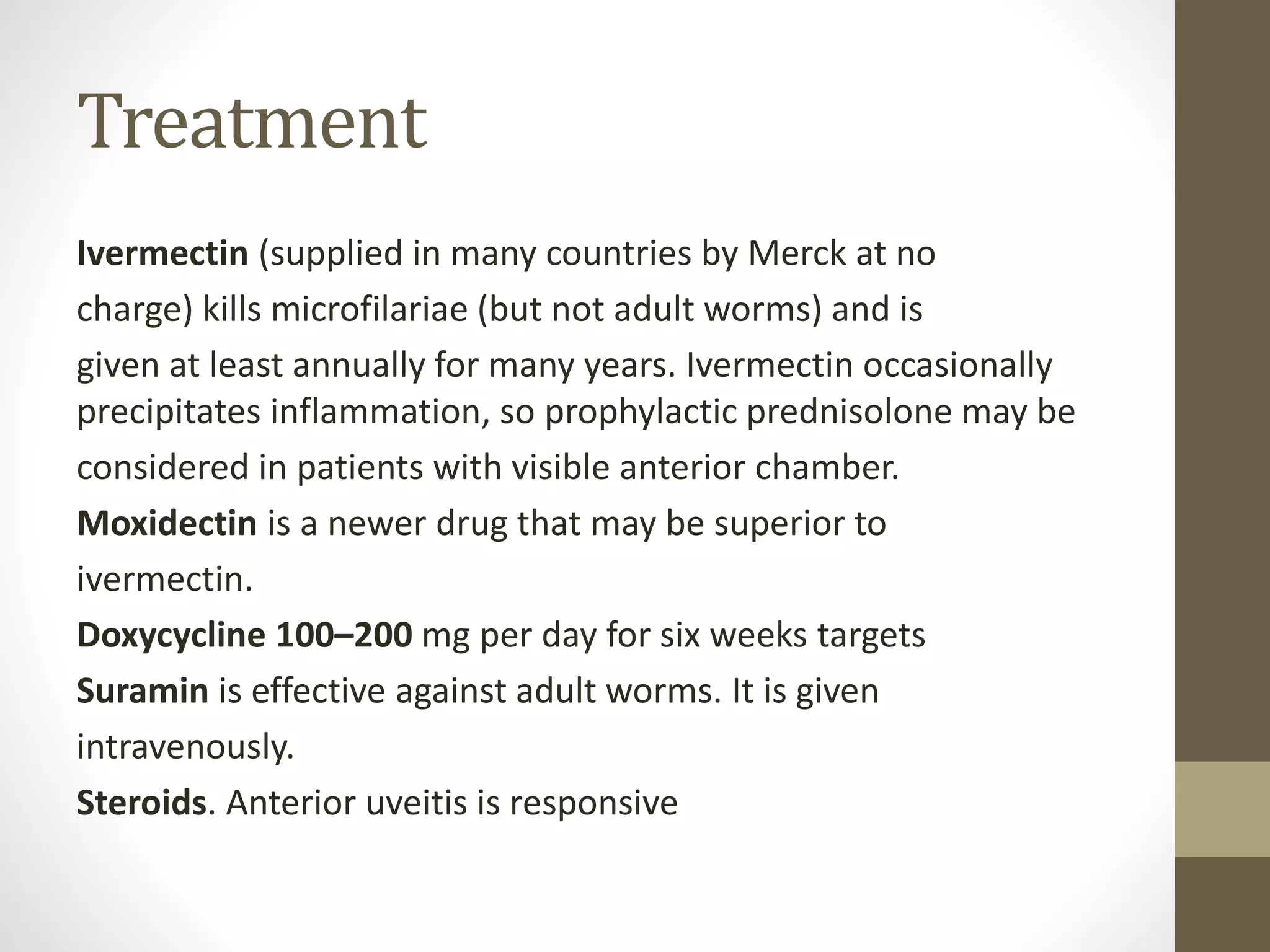
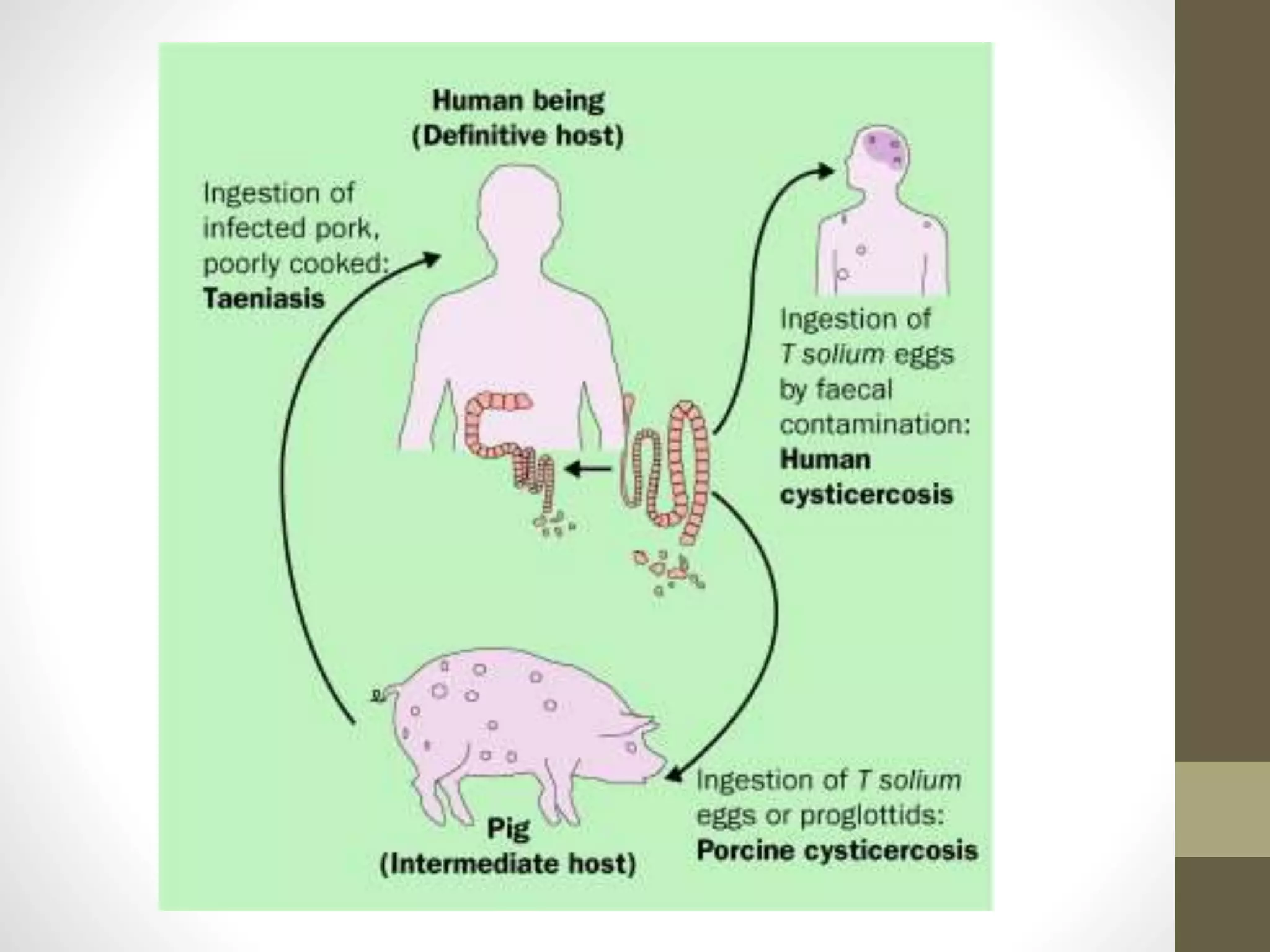
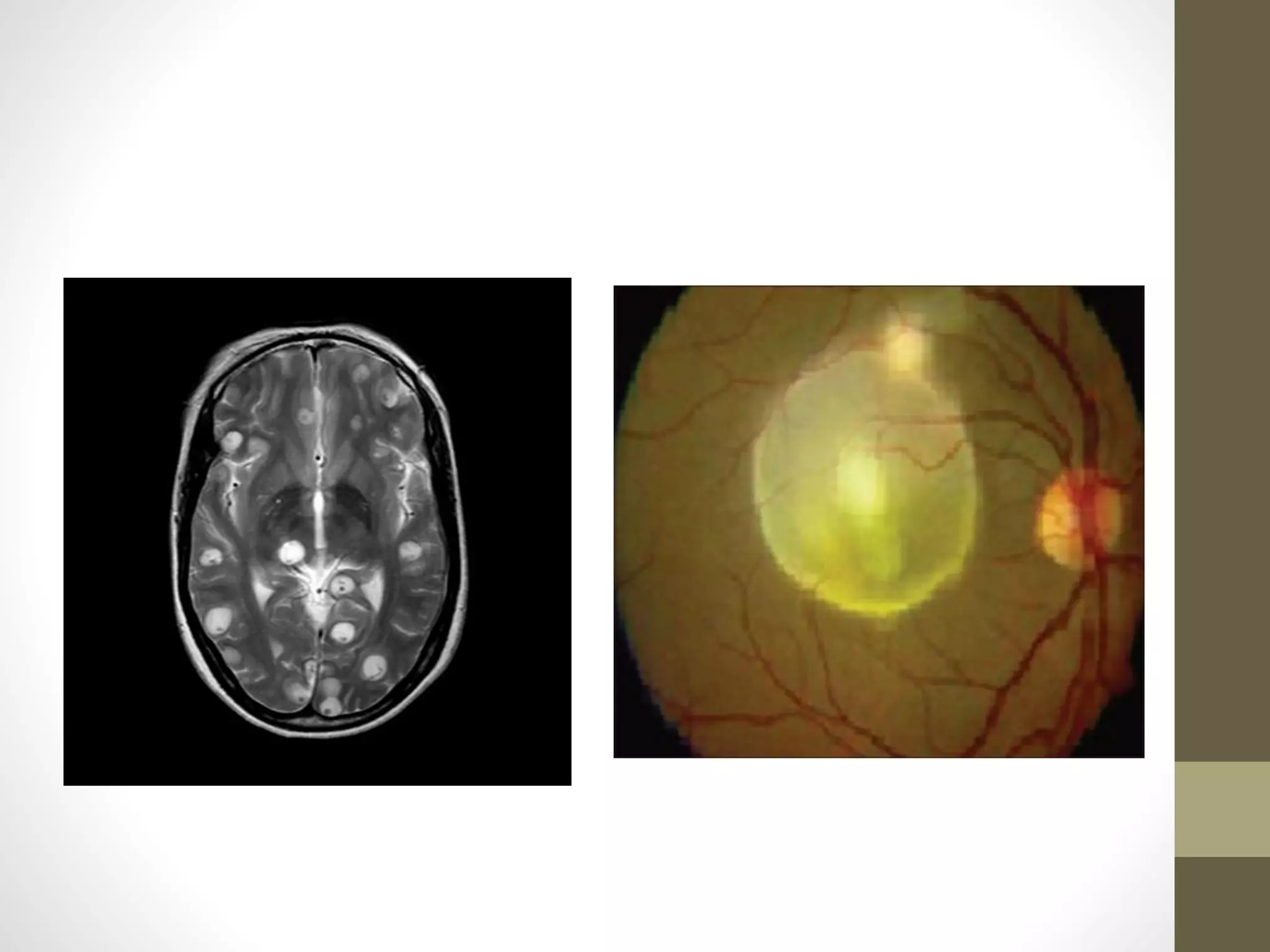
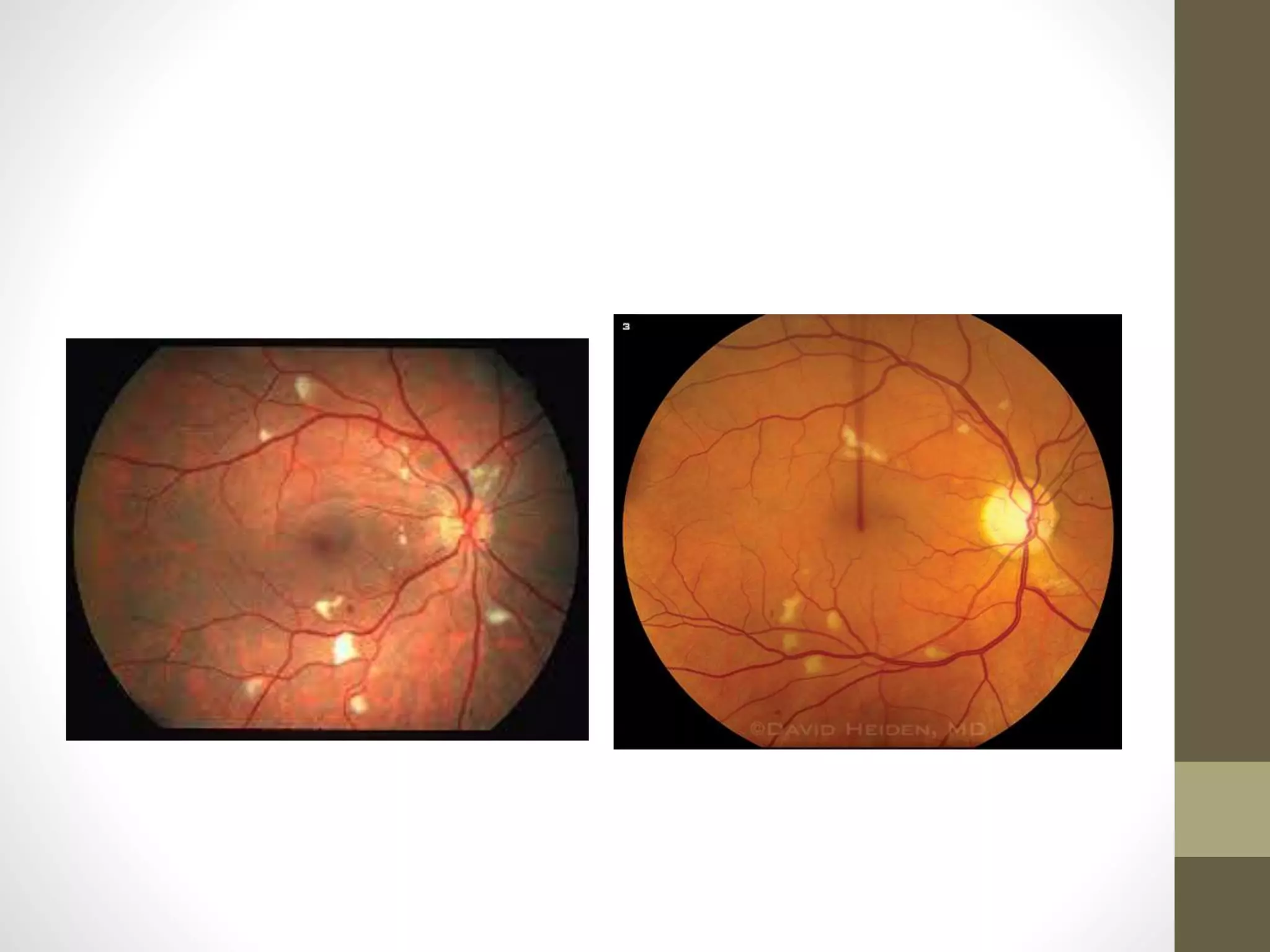
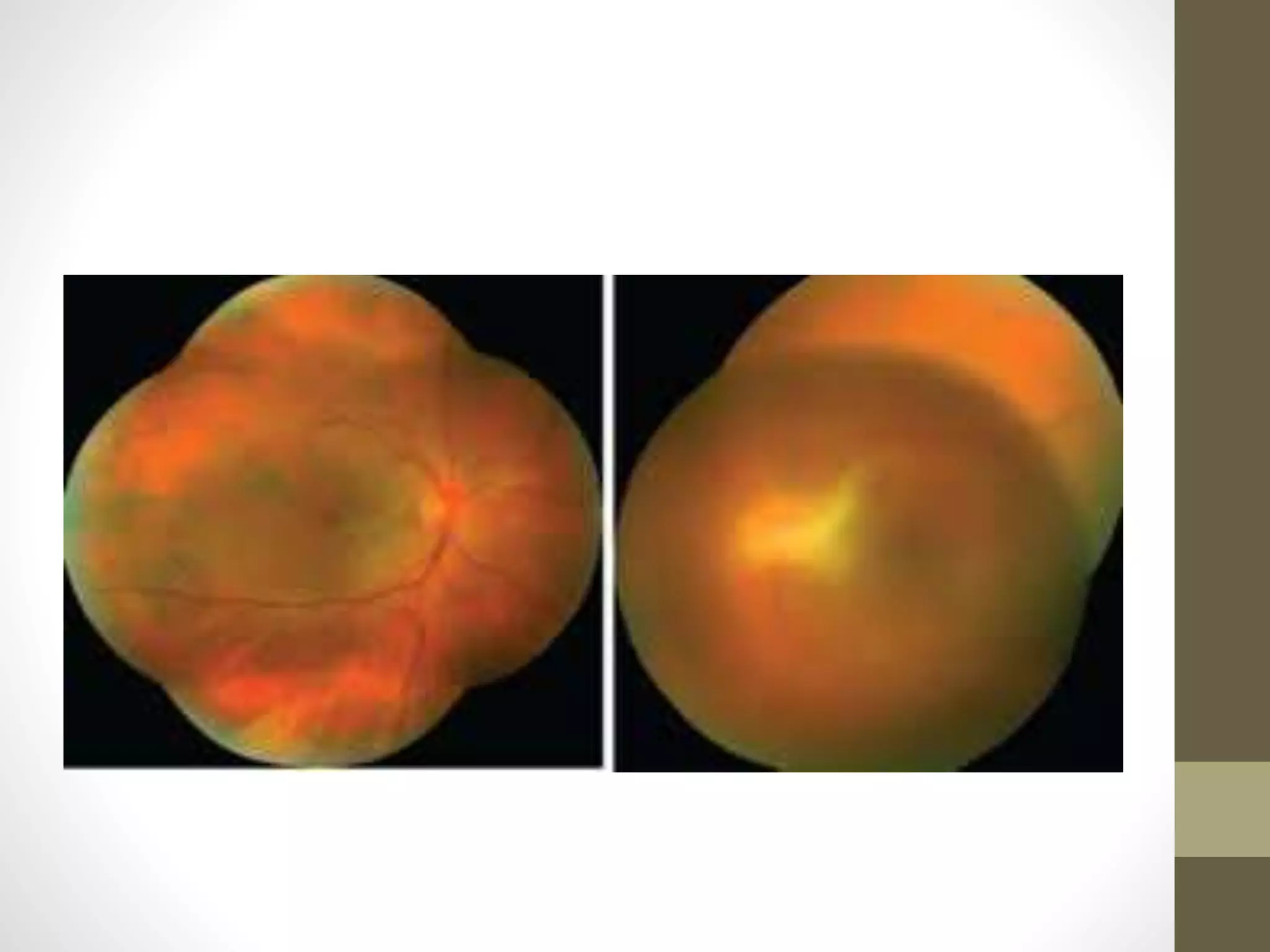
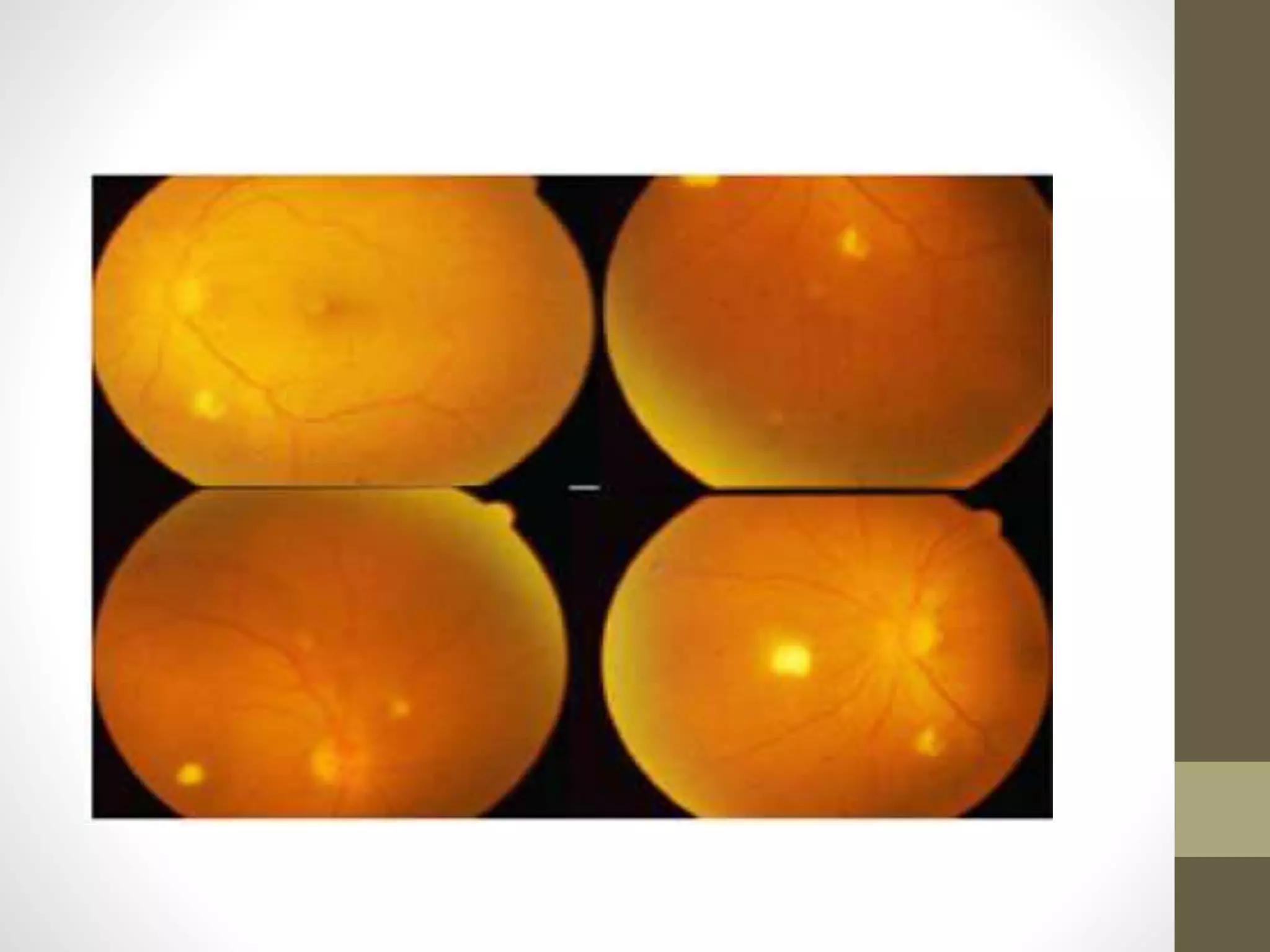
The document provides an extensive overview of various types of parasitic uveitis, including toxoplasmosis, toxocariasis, onchocerciasis, and cysticercosis, detailing their causes, symptoms, ocular features, and treatment options. Toxoplasmosis is highlighted as a significant cause of posterior uveitis with various treatment regimens mentioned, including the use of steroids and anti-toxoplasma agents. Other conditions like viral uveitis related to HIV infection and cytomegalovirus are also discussed, emphasizing the importance of understanding the systemic and ocular implications of these infections.