This document discusses endophthalmitis, including:
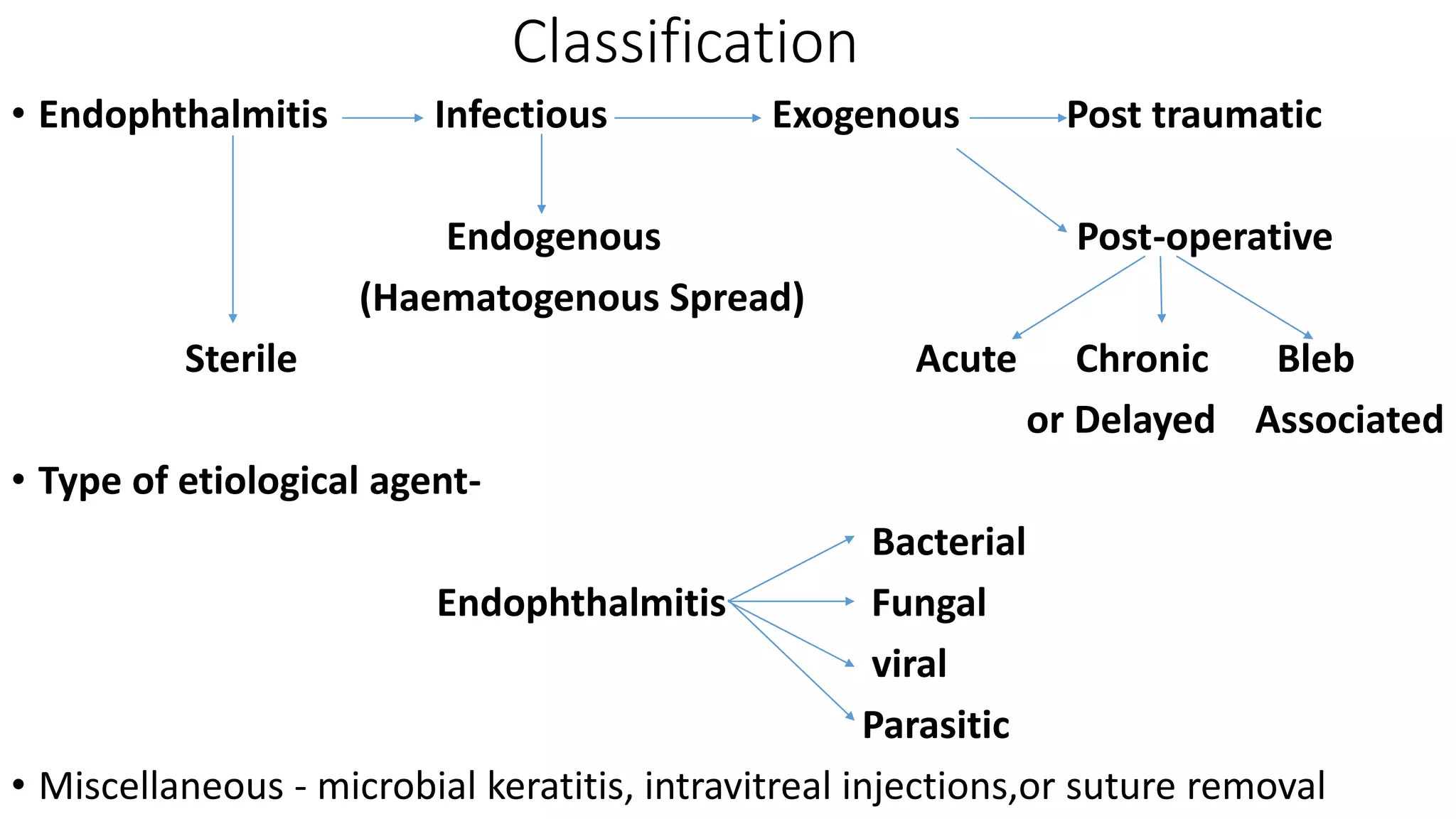
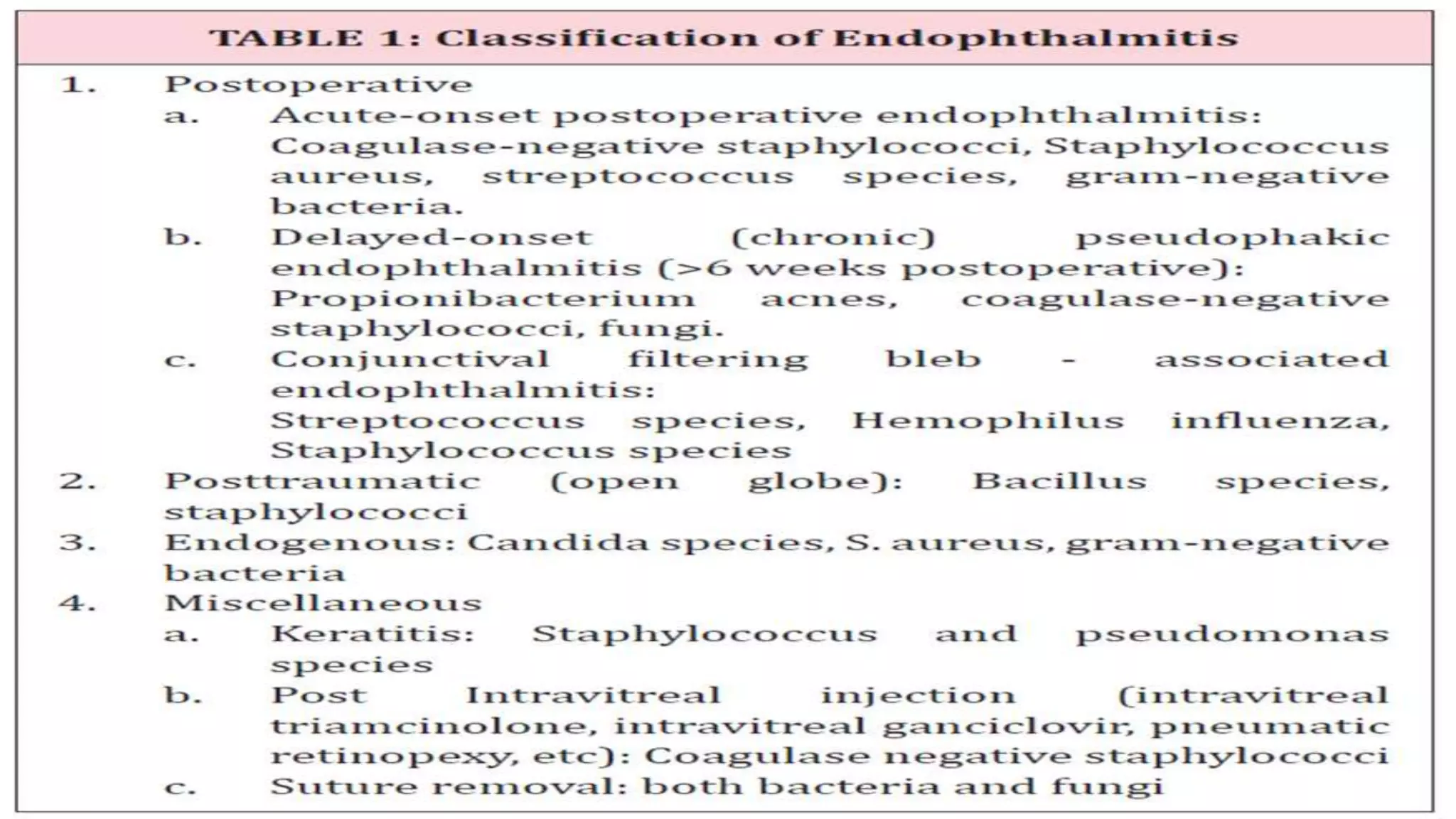
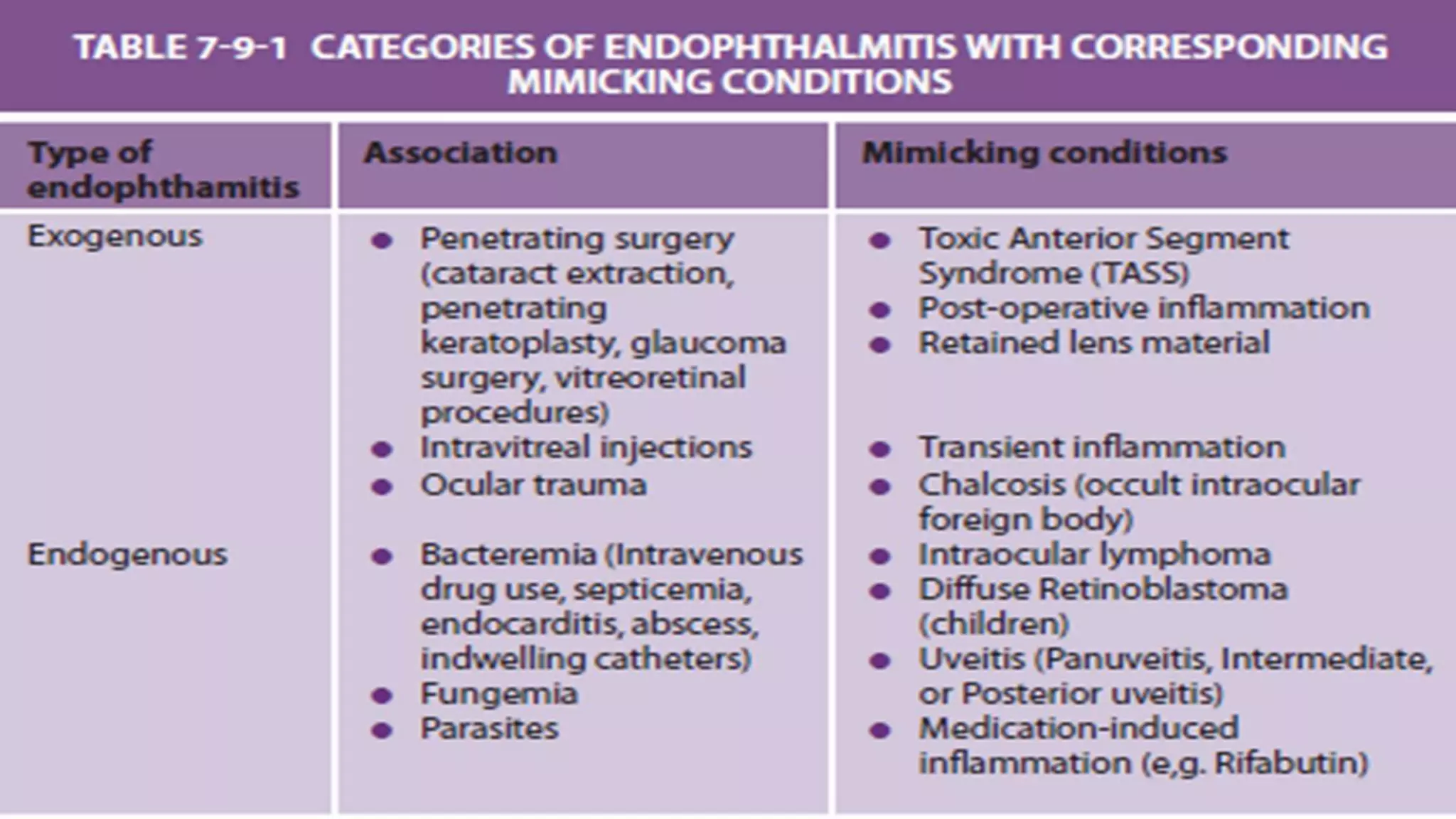
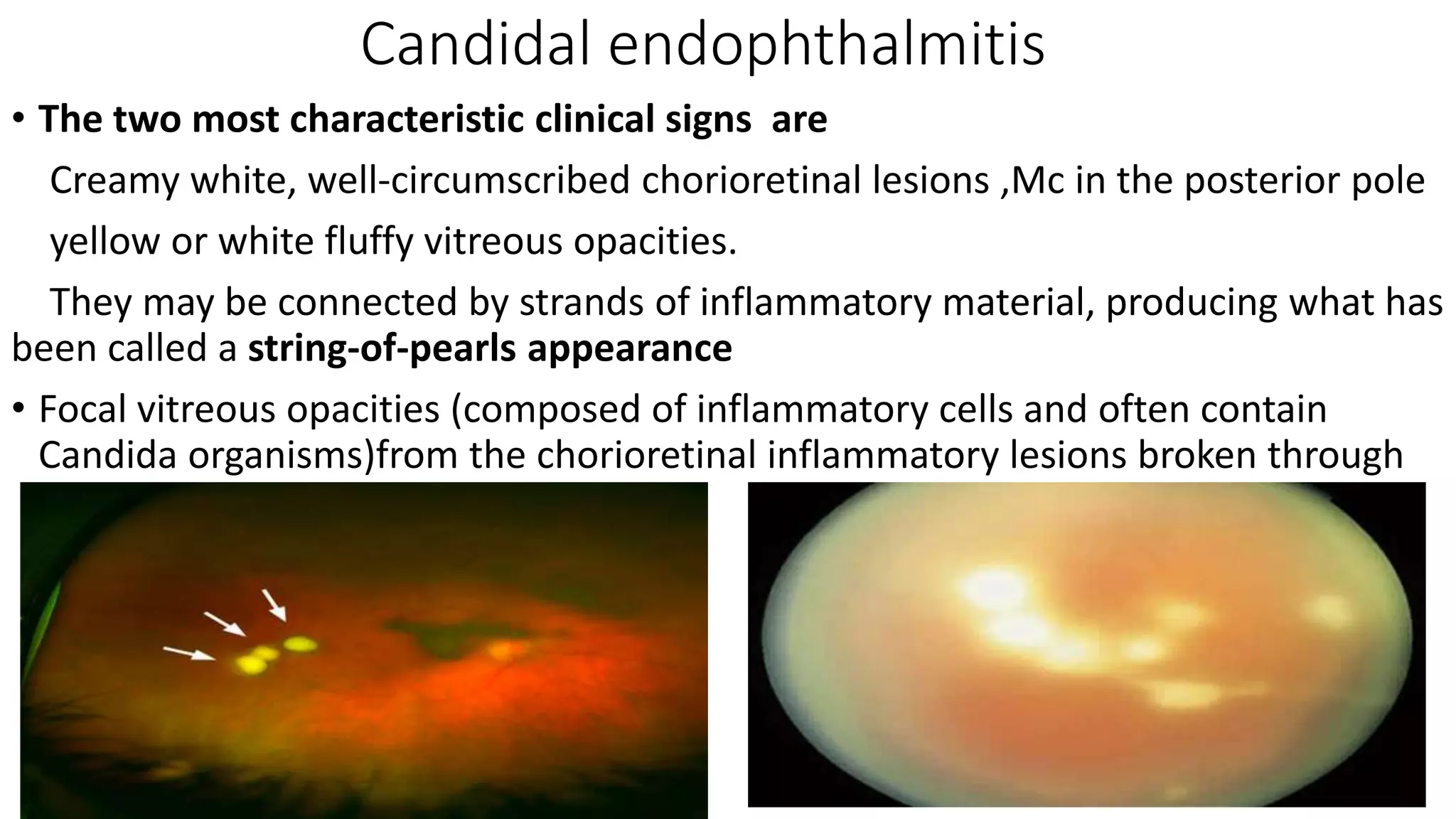
1) Endophthalmitis is an inflammatory condition of the inner eye structures caused by invading microorganisms. It can be classified based on infectivity, mode of entry, and type of causative agent.
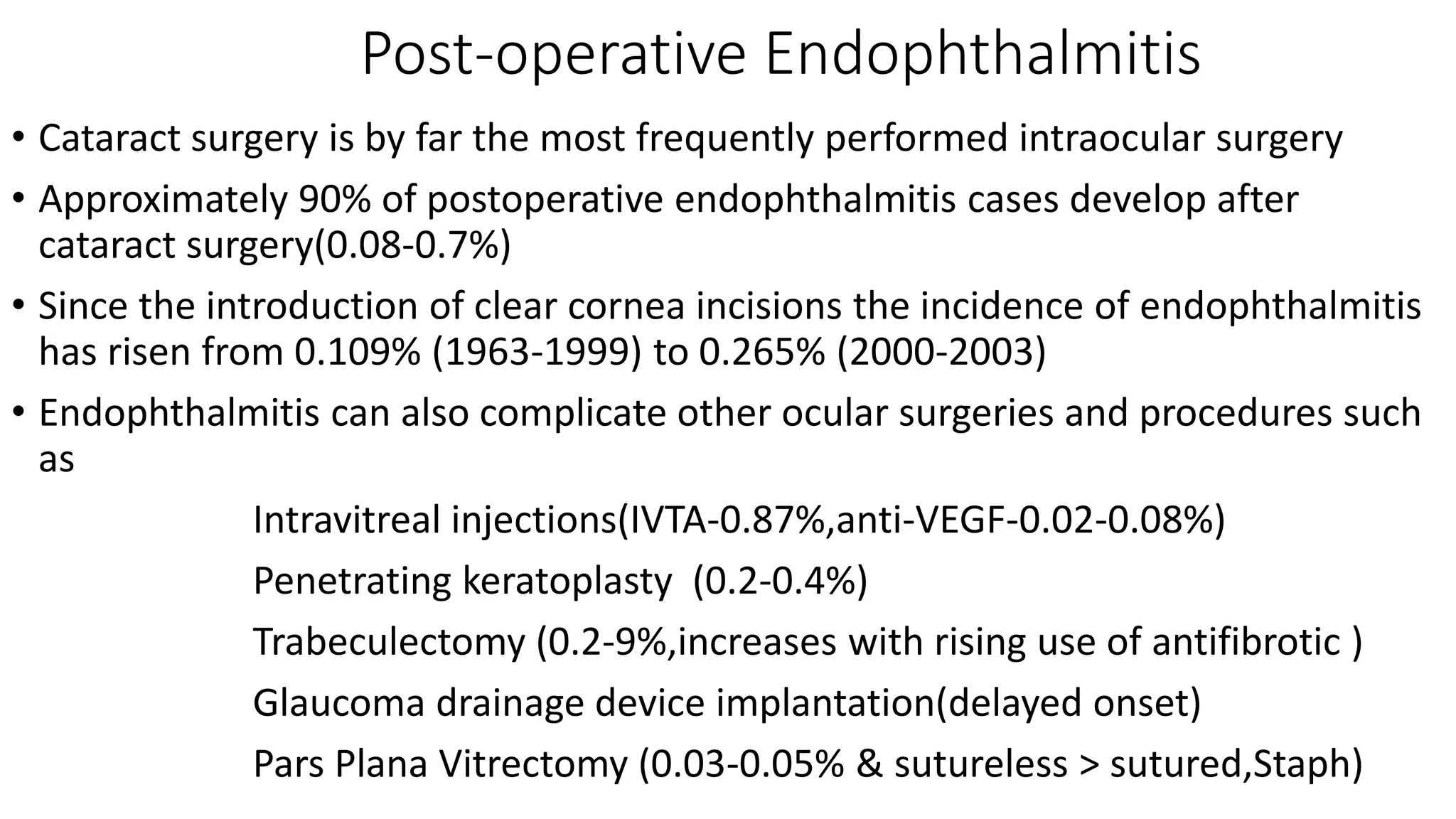
2) Common causes include bacteria like staphylococci and streptococci, fungi such as candida and aspergillus, and parasites. It can develop after ocular surgeries, trauma, or through hematogenous spread.
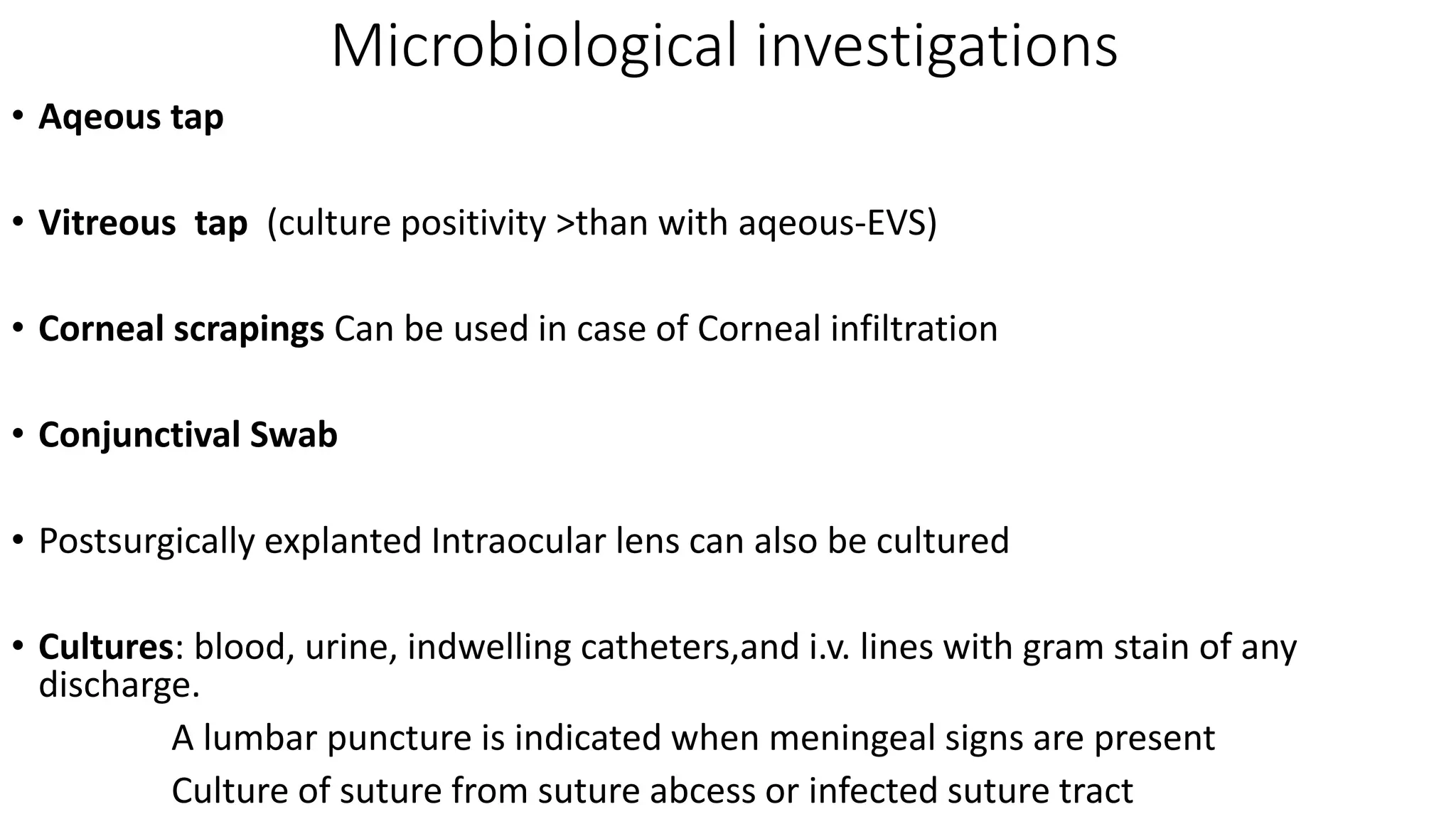
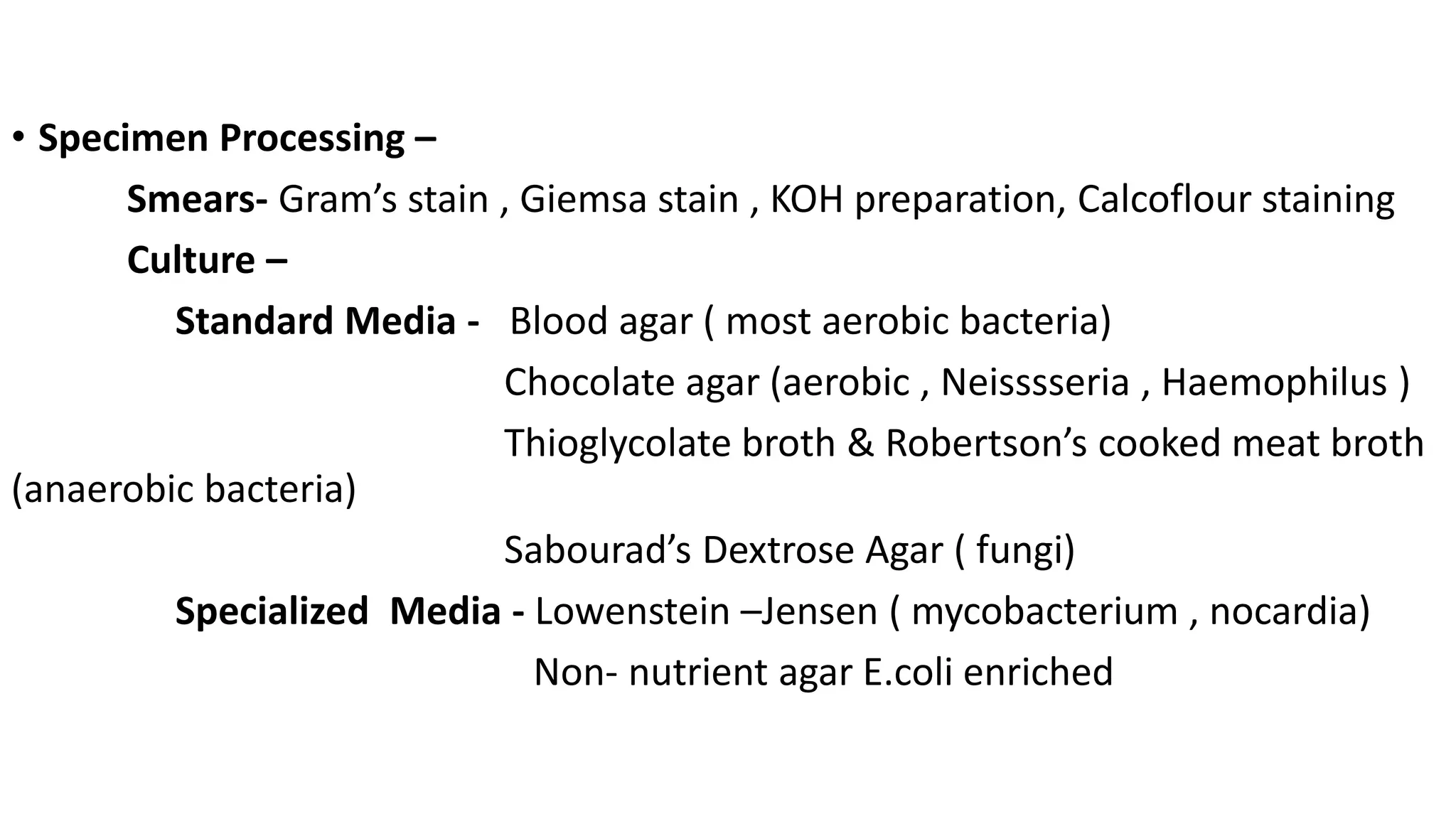
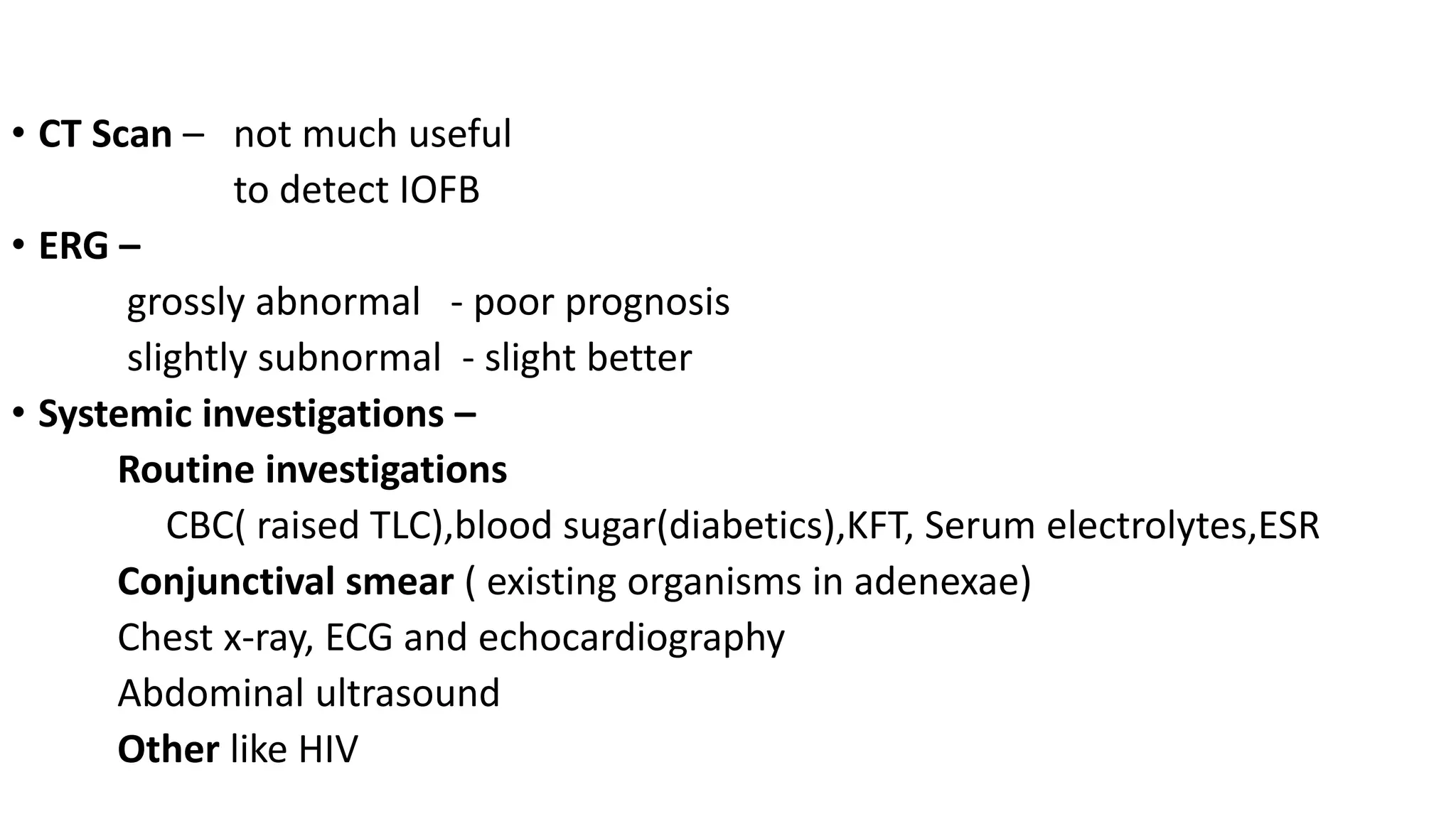
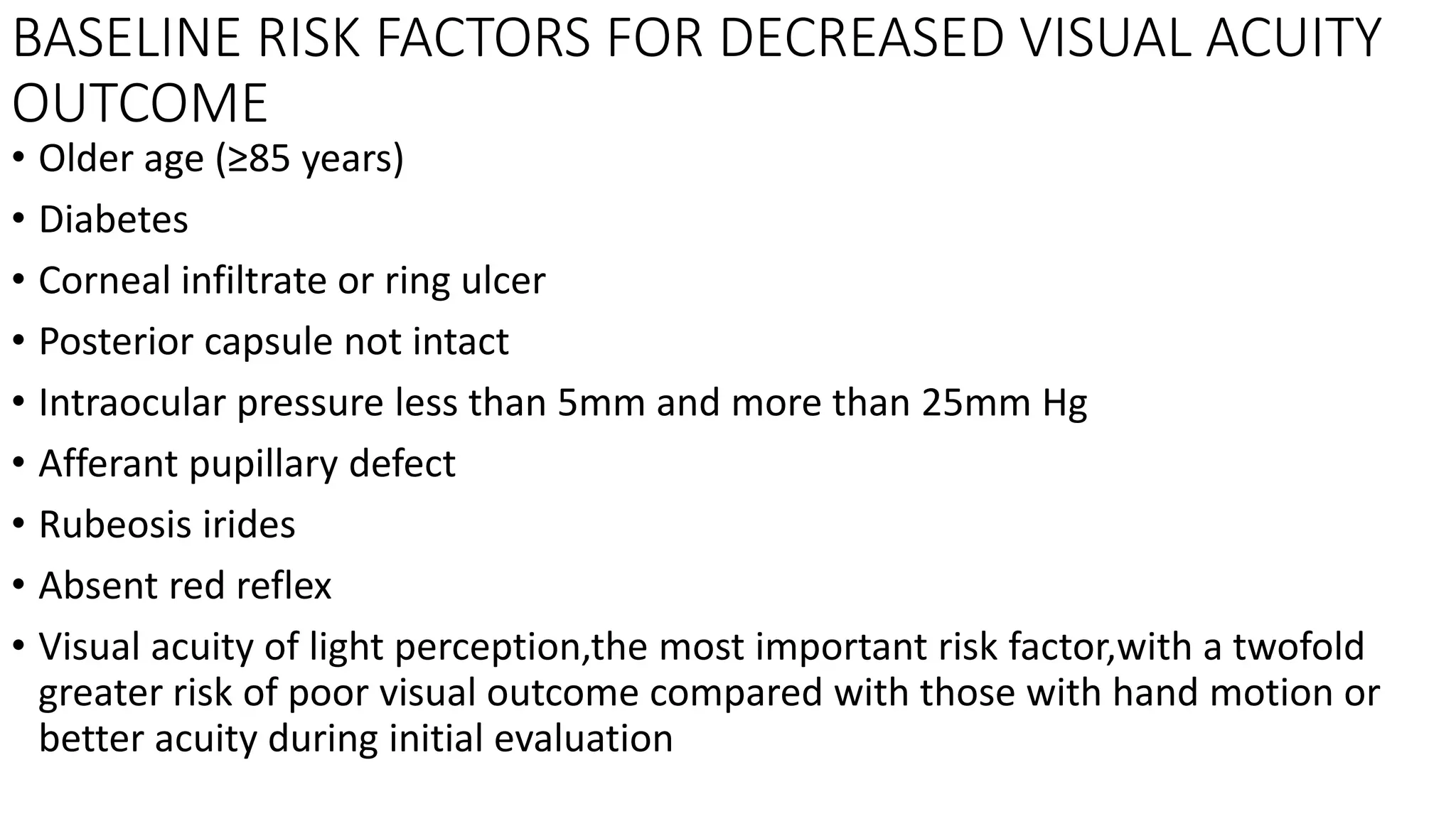
3) Diagnosis involves ophthalmic examination looking for signs of inflammation and infection. Microbiological testing through aqueous or vitreous taps can identify causative organisms. Prompt