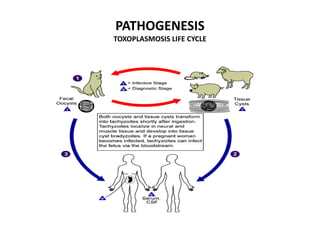
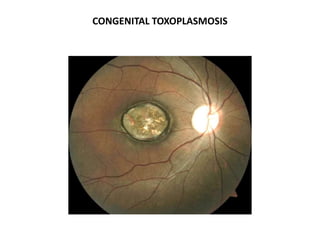
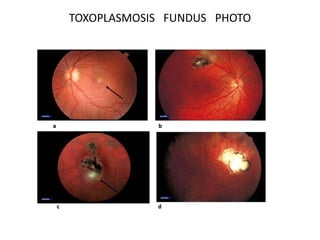
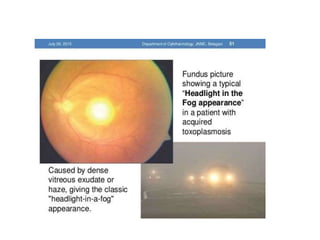
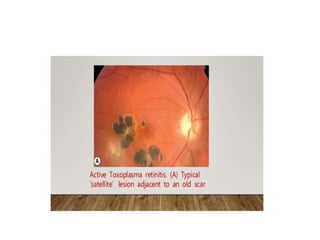
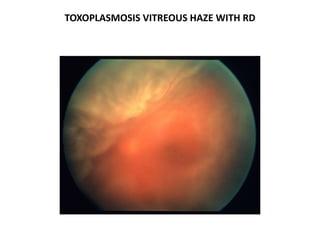
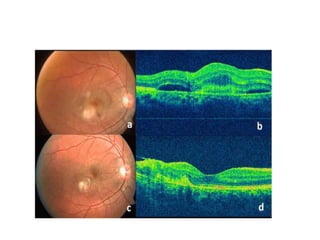
Toxoplasmosis is caused by the protozoan Toxoplasma gondii. It can cause congenital infection in fetuses if a woman is infected during pregnancy. Clinical features in infants may include chorioretinitis, hydrocephalus, or intracerebral calcifications. Ocular features include posterior uveitis, retinitis, or chorioretinitis. Diagnosis is usually based on clinical examination and serology. Treatment involves pyrimethamine, sulfadiazine, and prednisolone (triple therapy), along with folate supplementation to prevent side effects. Maintenance therapy may be used long-term in immunocompromised patients to prevent reactivation.