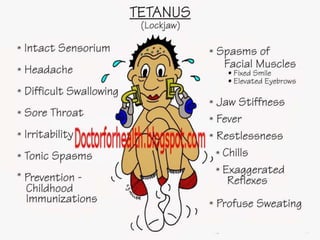
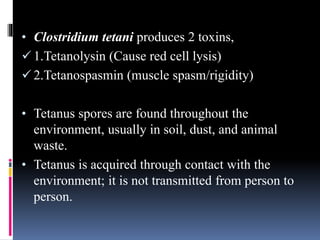
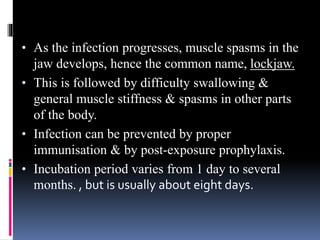
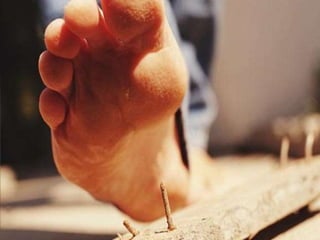
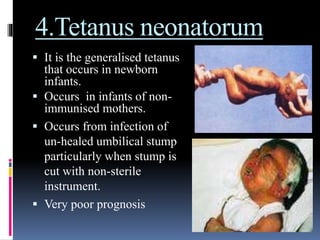
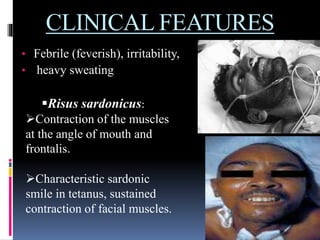
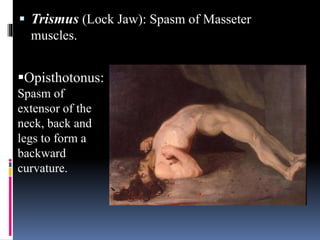
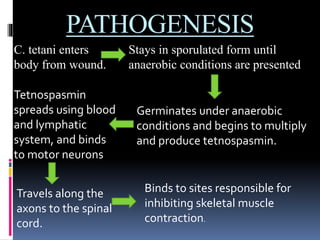
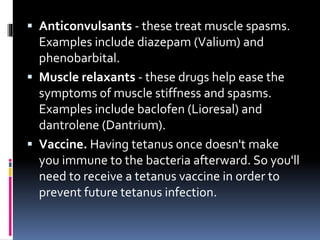
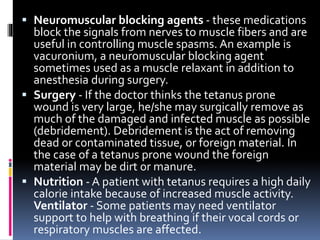
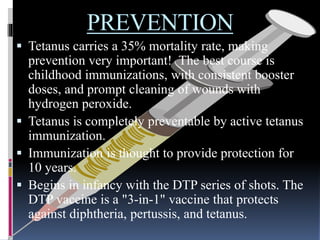
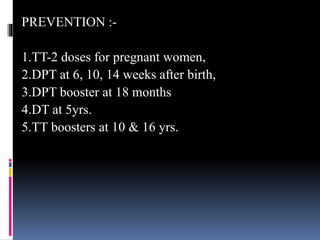
Tetanus is caused by Clostridium tetani bacteria entering the body through wounds. It produces a toxin that causes painful muscle spasms. Symptoms include lockjaw, back arching, and muscle stiffness. Treatment focuses on wound cleaning, antibiotics, muscle relaxants, and preventing complications until the toxin dissipates. Tetanus can be fatal if not properly treated. Vaccination provides the best prevention against this infectious disease.