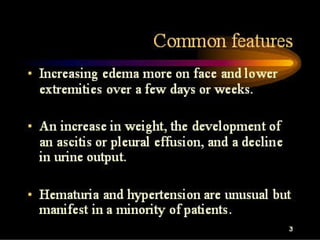
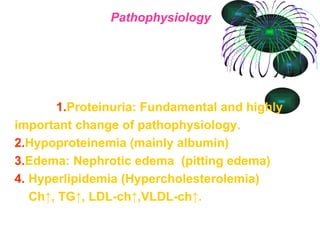
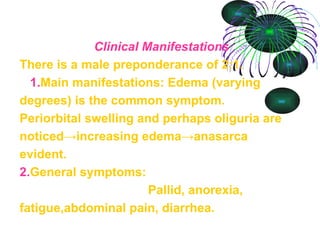
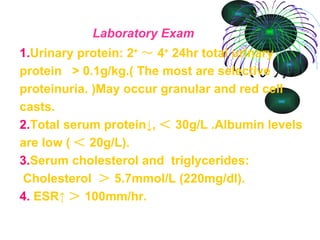
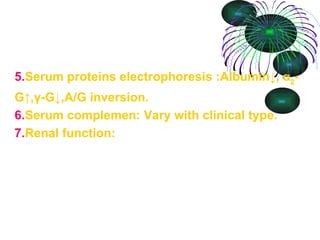
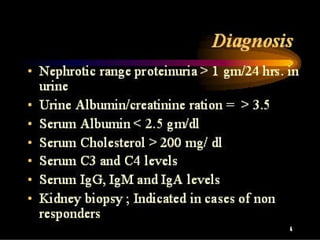
Nephrotic syndrome is characterized by proteinuria, low protein levels, edema, and high cholesterol. It is caused by increased permeability of the glomerular basement membrane, allowing protein to pass into the urine. Symptoms include edema, fatigue, and abdominal pain. Laboratory tests show protein in the urine, low serum protein and albumin levels, and elevated cholesterol. Treatment focuses on restricting salt and protein intake, using diuretics to control edema, and treating the underlying cause, often by using corticosteroids or other immunosuppressive drugs. The prognosis depends on the cause, with minimal change disease often responding well to treatment.

![General measures (supportive) Monitoring and maintaining euvolemia (the correct amount of fluid in the body): monitoring urine output, BP regularly fluid restrict to 1L diuretics (IV furosemide) Monitoring kidney function: do EUCs daily and calculating GFR Prevent and treat any complications [see below] Albumin infusions are generally not used because their effect lasts only transiently. Prophylactic anticoagulation may be appropriate in some circumstances. [4]](https://image.slidesharecdn.com/nephroticsyndrome-091201023028-phpapp01/85/Nephrotic-Syndrome-16-320.jpg)
![Specific treatment of underlying cause Immunosuppression for the glomerulonephritides ( corticosteroids [5] , ciclosporin ). Standard ISKDC regime for first episode: prednisolone -60 mg/m2/day in 3 divided doses for 4 weeks followed by 40 mg/m2/day in a single dose on every alternate day for 4 weeks. Relapses by prednisolone 2 mg/kg/day till urine becomes negative for protein. Then, 1.5 mg/kg/day for 4 weeks. Frequent relapses treated by: cyclophosphamide or nitrogen mustard or ciclosporin or levamisole . Achieving stricter blood glucose control if diabetic. Blood pressure control. ACE inhibitors are the drug of choice. Independent of their blood pressure lowering effect, they have been shown to decrease protein loss.](https://image.slidesharecdn.com/nephroticsyndrome-091201023028-phpapp01/85/Nephrotic-Syndrome-17-320.jpg)