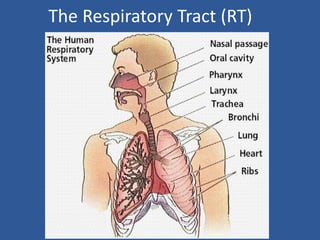
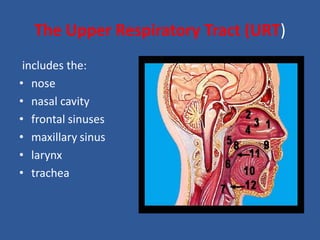
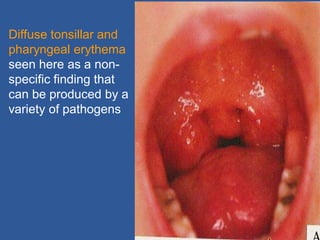
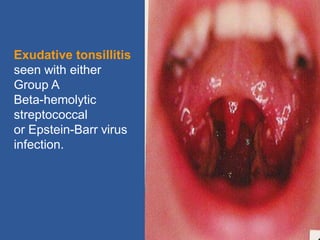
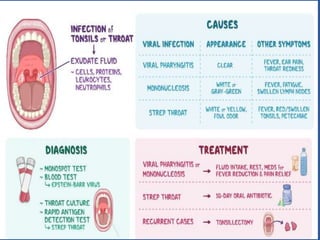
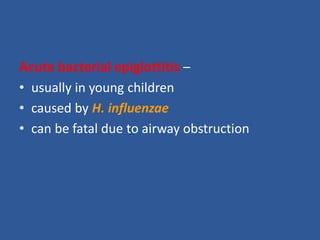
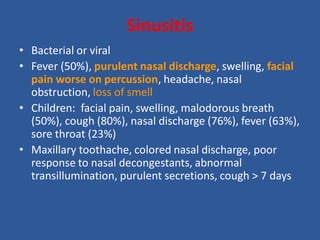
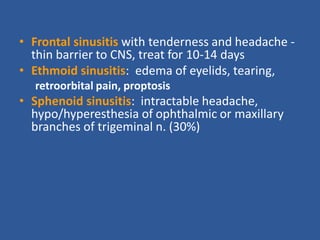
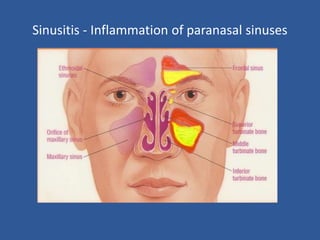
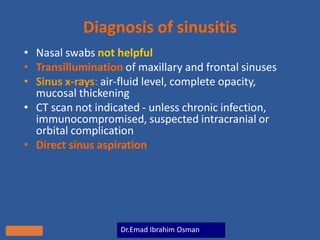
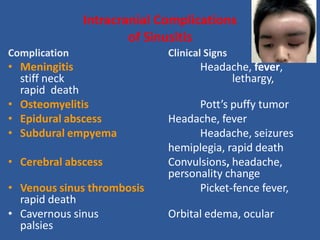
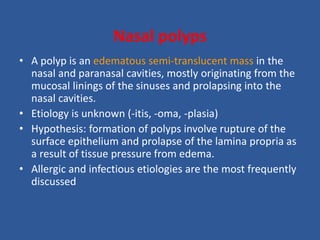
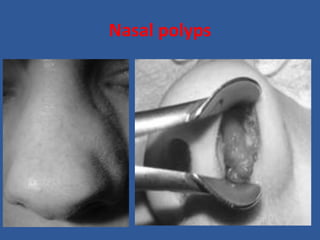
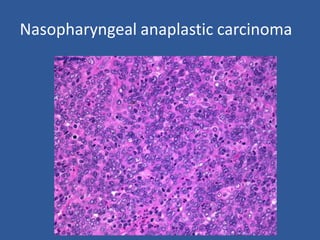
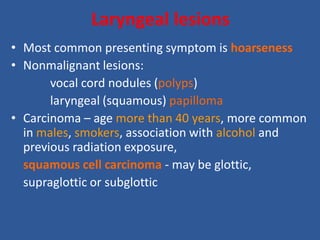
This document provides an overview of upper respiratory tract pathologies, including infections, lesions, and tumors. It discusses common conditions such as the common cold, acute pharyngitis, and sinusitis, along with their causes, symptoms, and potential complications. Additionally, it covers nasopharyngeal carcinoma and laryngeal lesions, highlighting their epidemiology, pathology, and clinical significance.