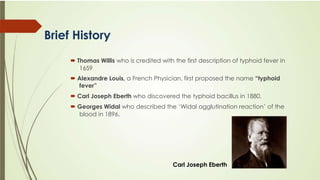
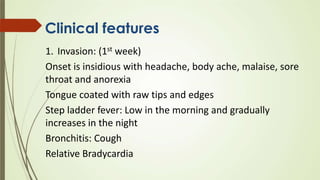
Typhoid fever is an infectious disease caused primarily by the bacterium Salmonella typhi, characterized by symptoms such as high fever, abdominal pain, and malaise, and predominantly occurs in areas with poor sanitation. The disease can be transmitted through contaminated food and water, with vaccination being a key prevention method. Treatment includes antibiotics and supportive care, though antibiotic resistance has become a significant concern.