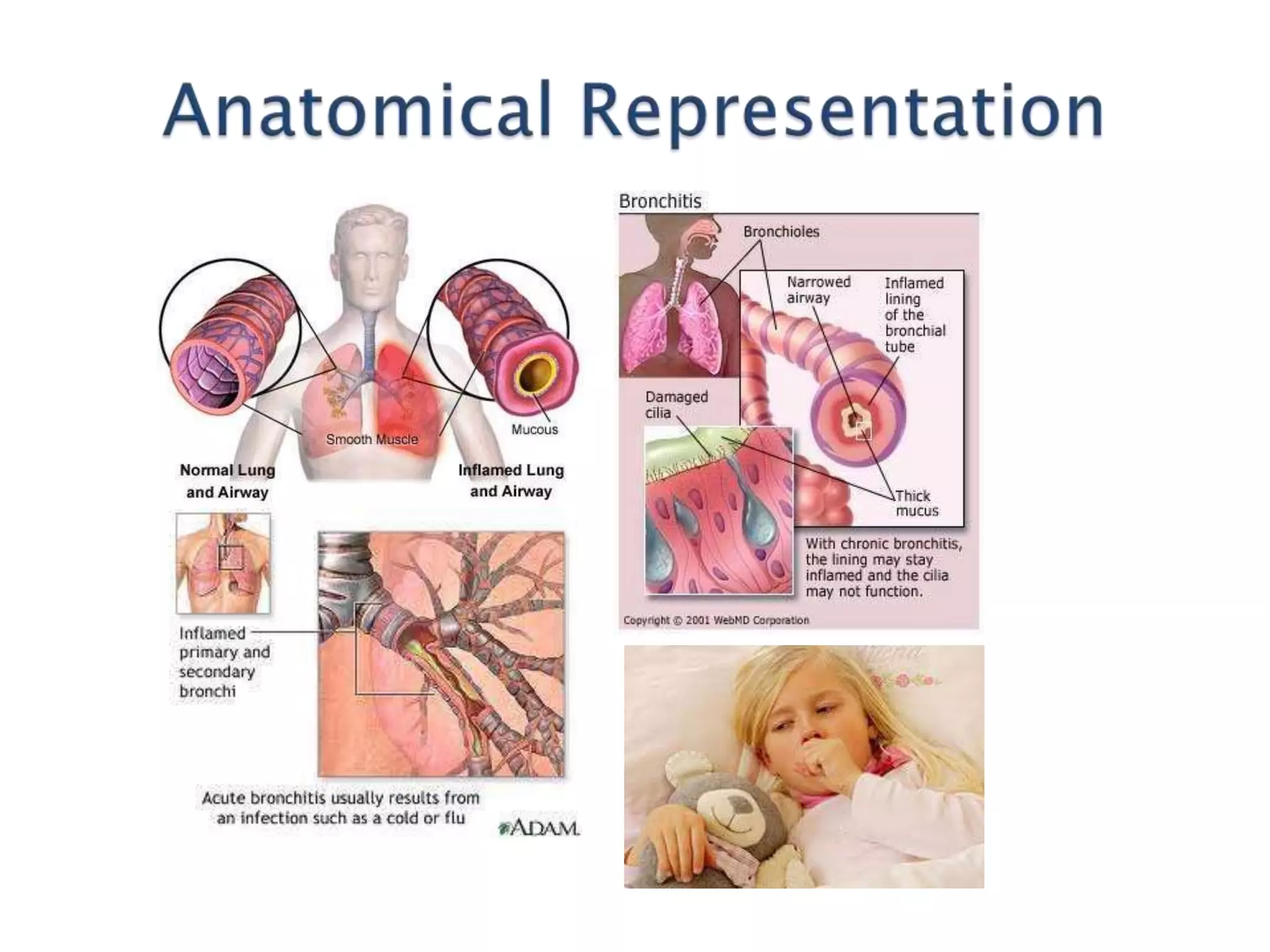
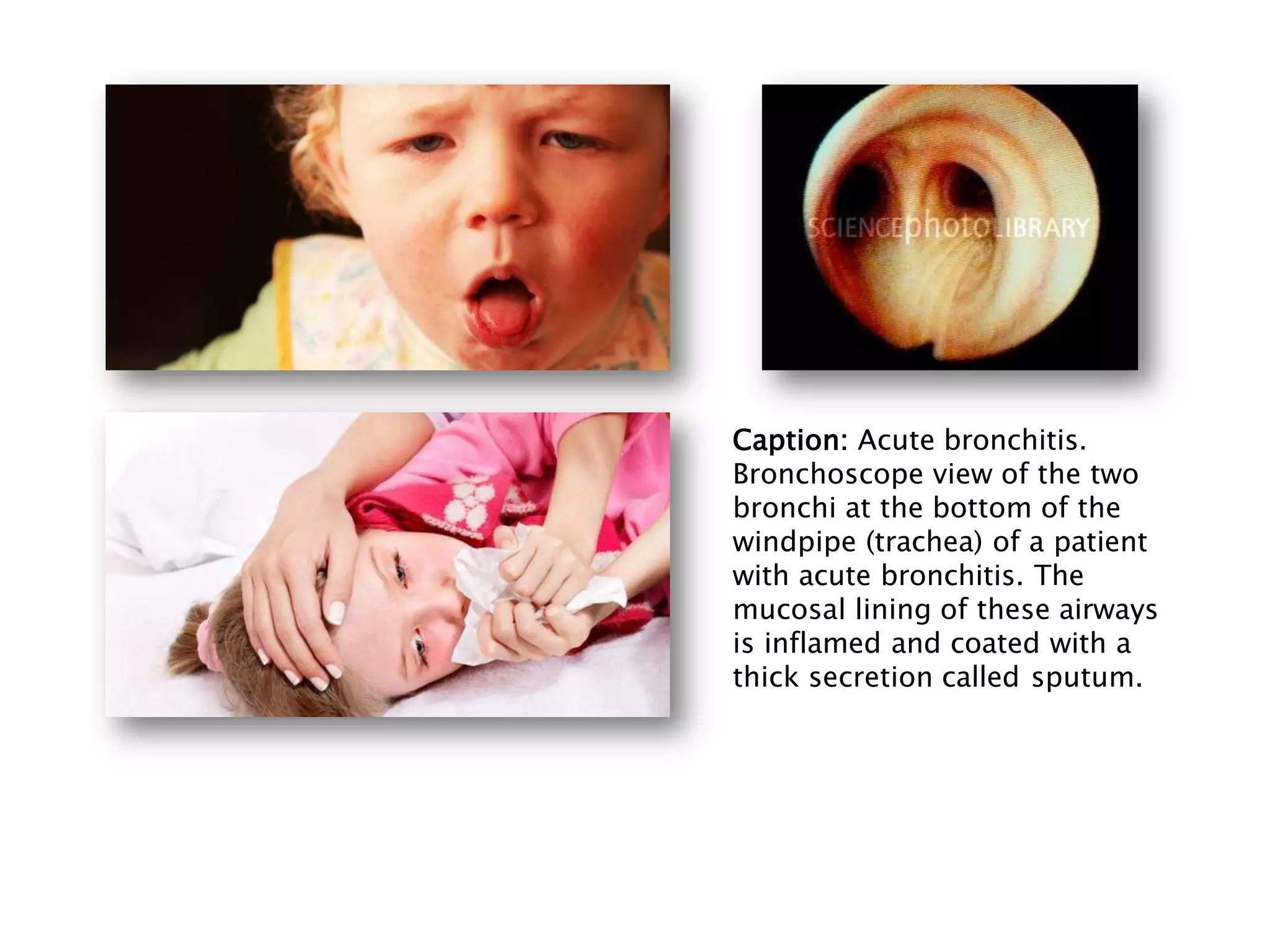
Acute bronchitis is an inflammation of the air passages within the lungs that causes coughing or other breathing problems. It usually starts as a cold or flu that has spread from the nose and throat to the windpipe and airways. Viruses are the most common cause. The illness typically lasts around 2 weeks and is generally not serious, resolving on its own as mucociliary clearance works to remove debris. Damage to the airway lining from recurrent infections can contribute to chronic bronchitis in childhood.