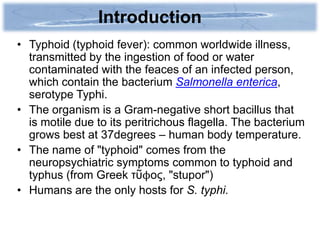
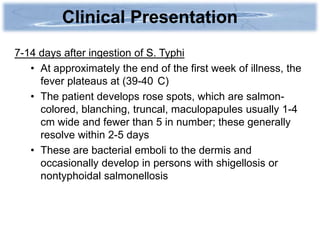
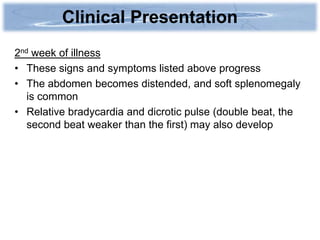
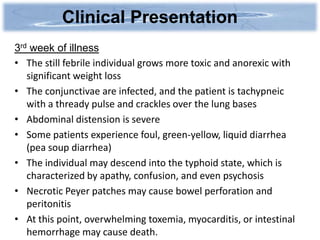
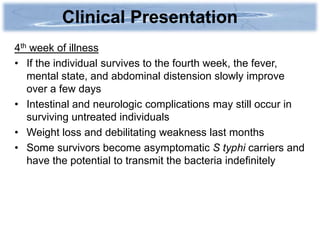
Typhoid fever is caused by the bacterium Salmonella enterica serotype Typhi and is transmitted through contaminated food or water. It has a variable incubation period of 1-2 weeks. Clinical presentation includes a stepwise fever pattern, gastrointestinal symptoms like abdominal pain, and occasionally a rose-colored rash. Without treatment, typhoid fever can last 3-4 weeks and be life threatening, but with antibiotics mortality is low. It remains common in areas with poor sanitation.