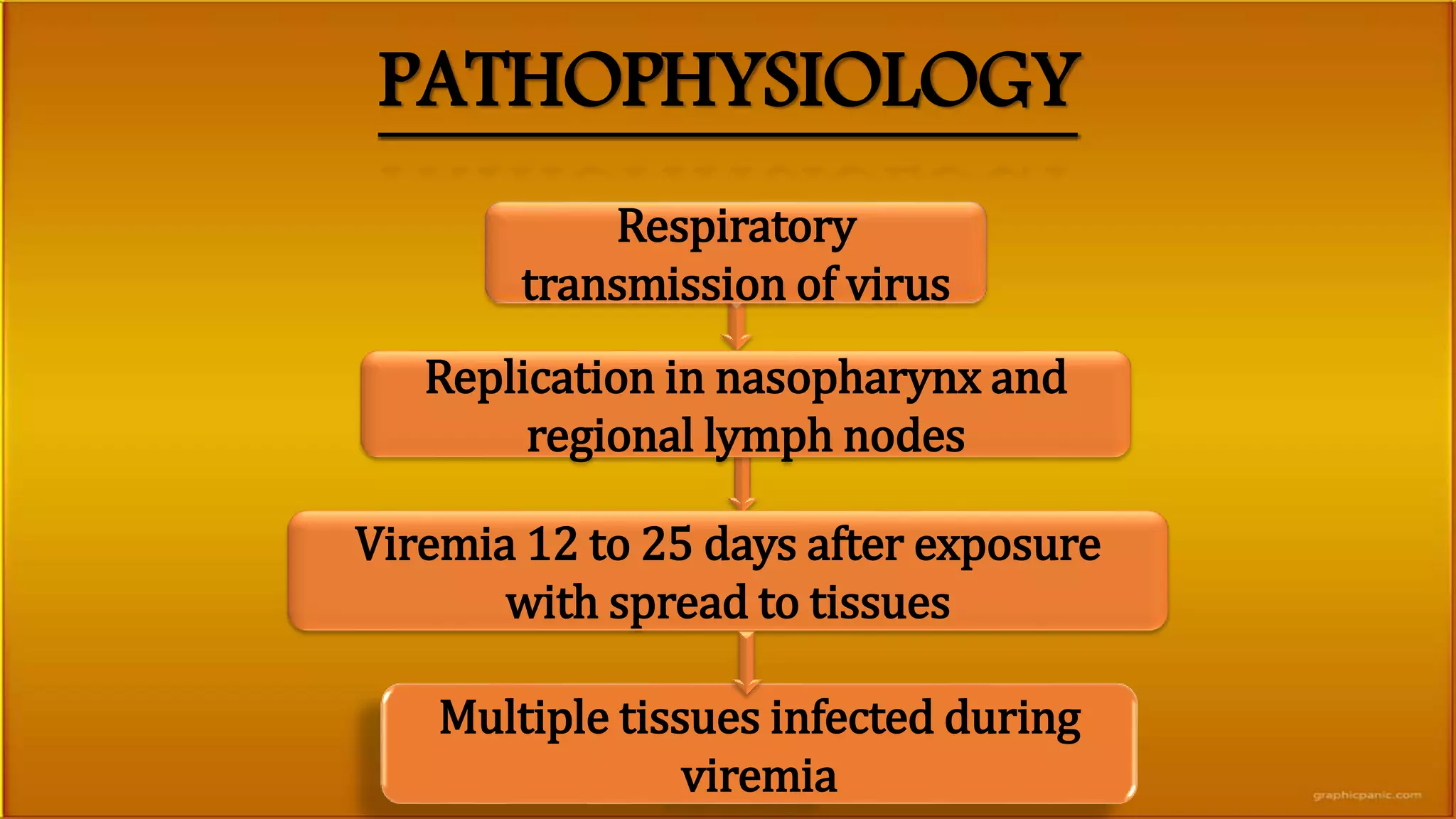
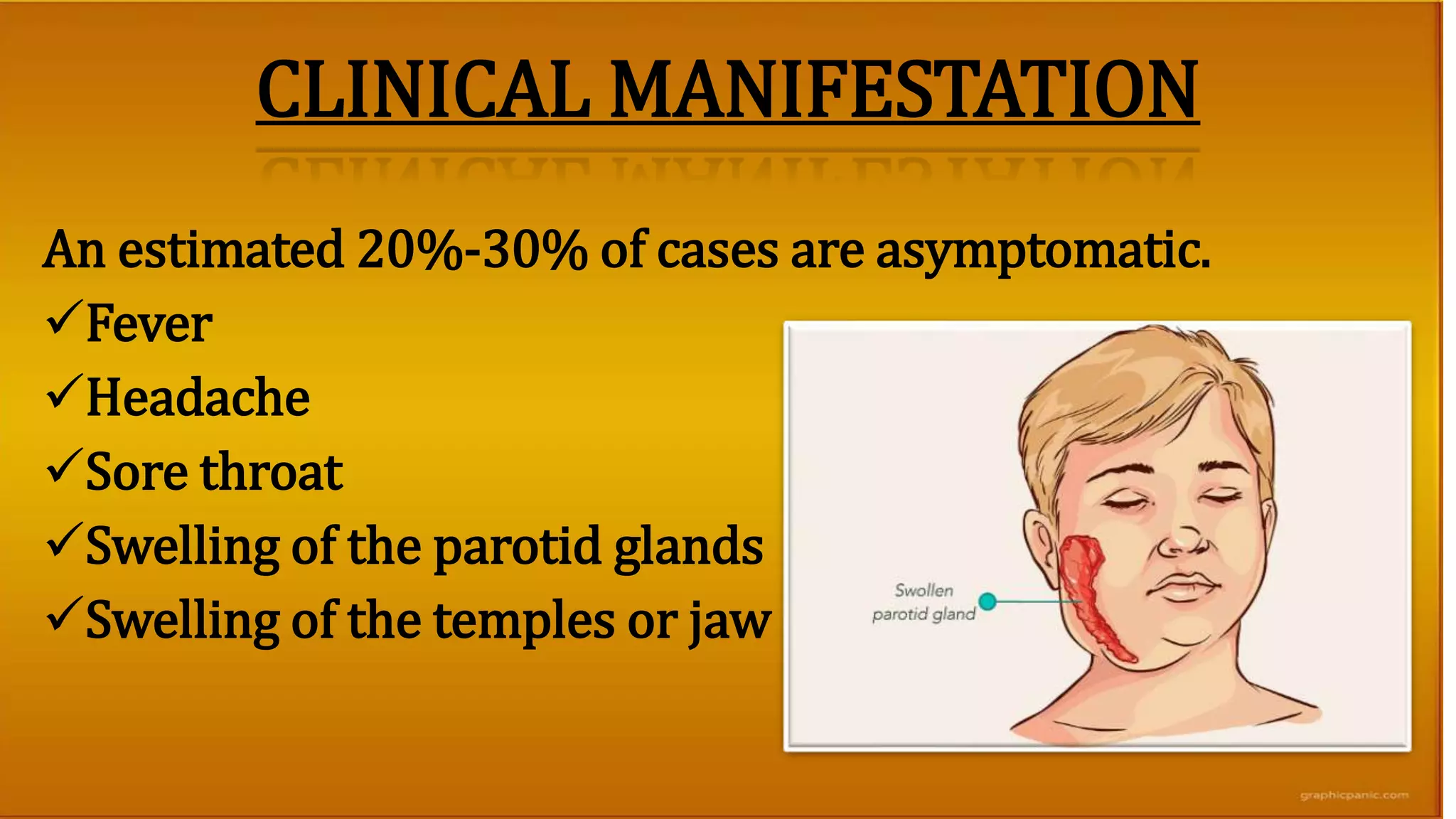
Mumps is a viral infection caused by a paramyxovirus that typically causes swelling of the parotid glands. It has an incubation period of 12-25 days and is transmitted through respiratory droplets. While many cases are asymptomatic, common symptoms include fever, headache, sore throat, and swelling of the parotid glands. Diagnosis is usually made clinically through physical examination. Treatment focuses on relieving symptoms through rest, fluids, fever medication, and application of warm or cold compresses. Vaccination with the MMR or MMRV vaccines can help prevent mumps.