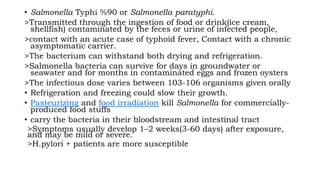
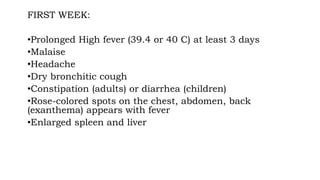
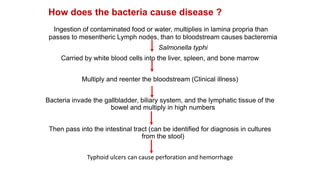
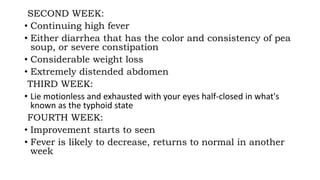
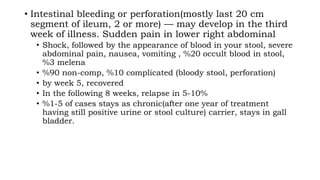
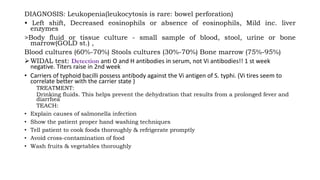
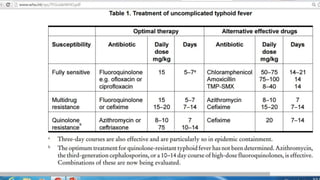
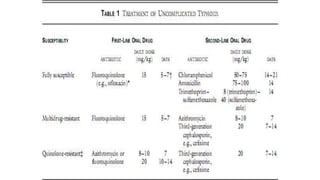
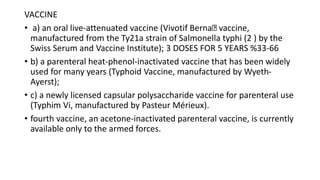
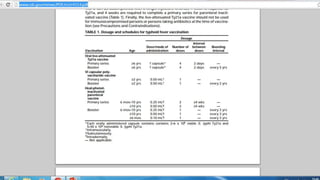
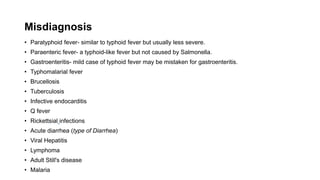
This document provides information about typhoid fever, also known as enteric fever. It is caused by the bacteria Salmonella Typhi or Paratyphi and is transmitted through contaminated food or water. Symptoms develop 1-3 weeks after exposure and include sustained high fever, headache, malaise and abdominal discomfort. Complications can include intestinal bleeding or perforation. Treatment involves antibiotics such as ciprofloxacin. Prevention focuses on proper hygiene, food handling and water treatment. Vaccines are also available but not completely protective.