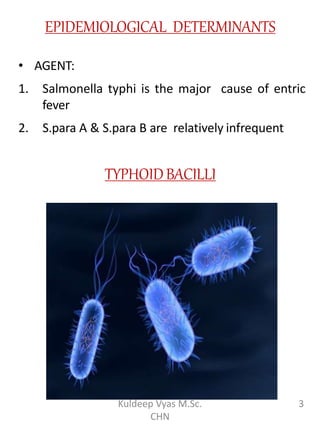
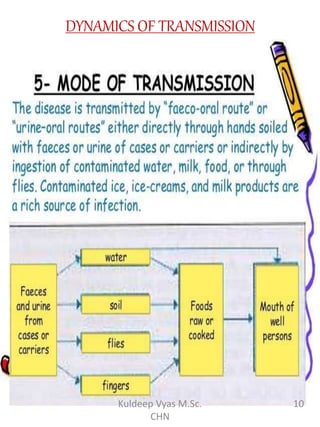
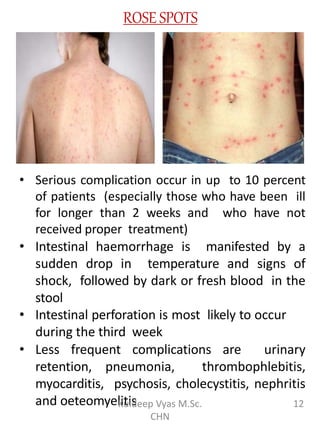
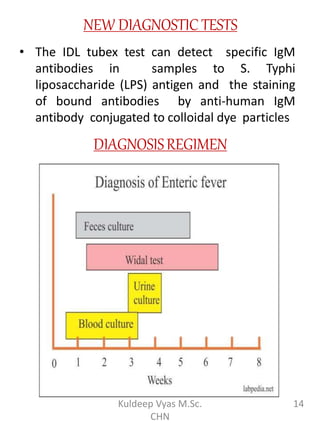
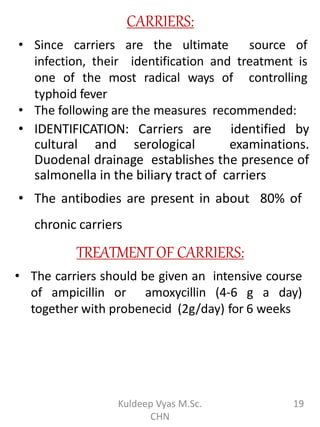
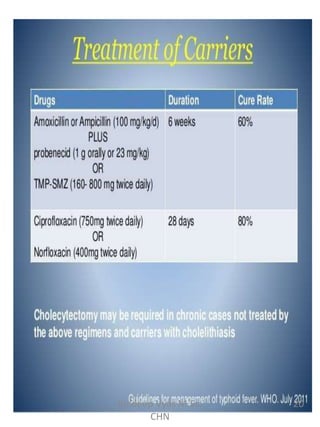
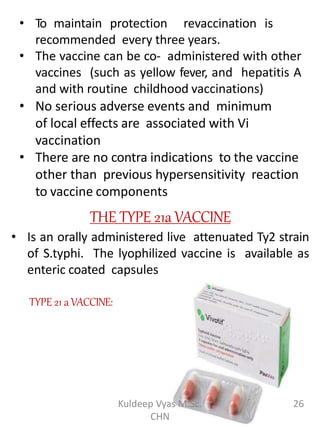
This document summarizes typhoid fever, caused by Salmonella typhi bacteria. It discusses the epidemiology, transmission, clinical features, diagnosis and control of the disease. Typhoid fever is transmitted through contaminated food, water or contact with carriers. It causes sustained fever for 2-3 weeks and can lead to serious complications without treatment. Diagnosis involves blood and stool cultures. Control relies on identifying carriers, improving sanitation, safe food/water handling, and immunization with Vi polysaccharide or live attenuated Ty21a vaccines.