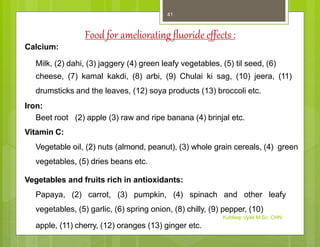
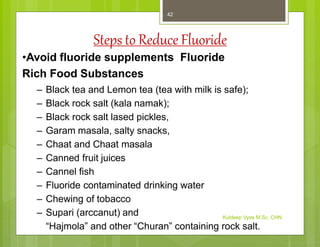
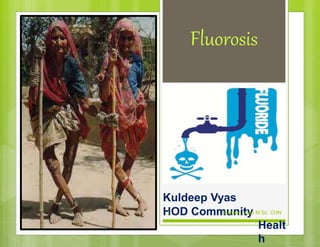
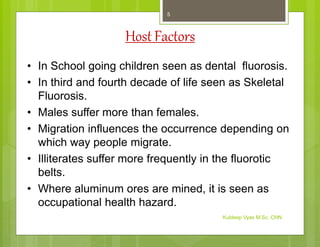
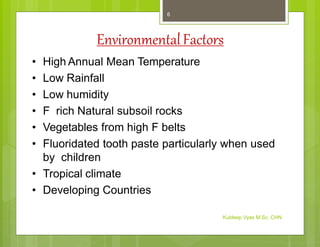
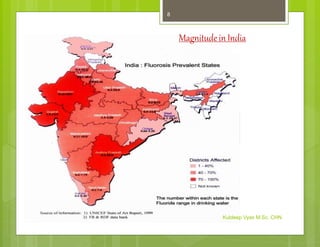
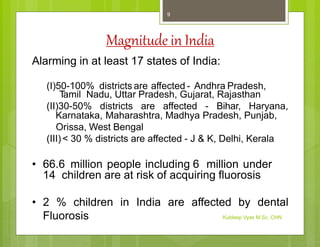
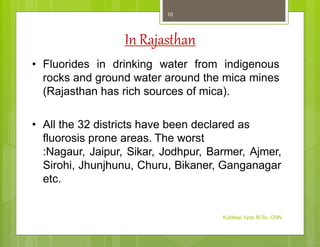
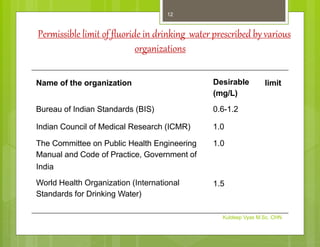
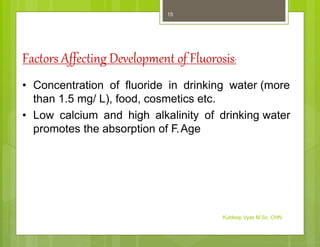
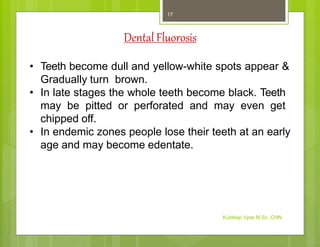
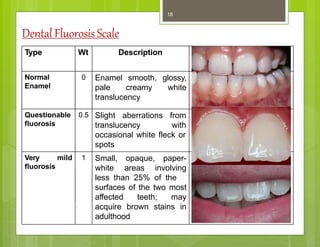
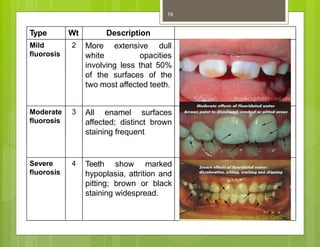
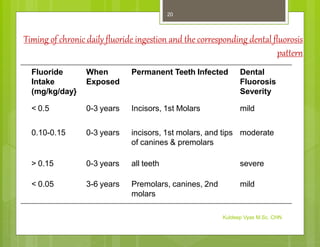
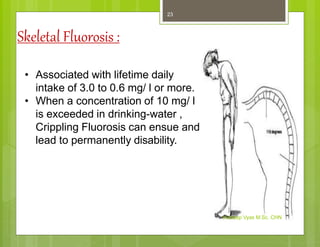
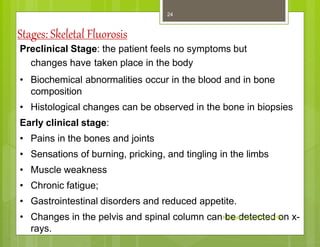
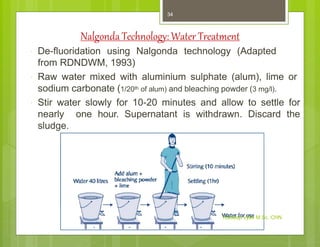
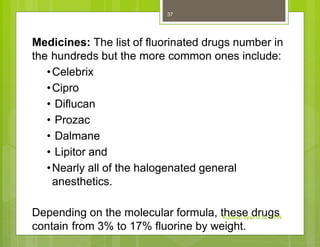
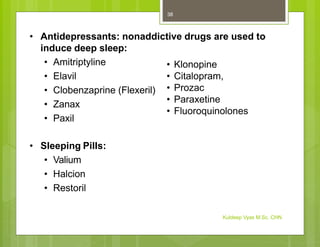
Fluorosis, or fluoride toxicity, is caused by elevated levels of fluoride intake. It is a worldwide problem, endemic in over 22 countries, with India and China being the worst affected in Asia. In India, Rajasthan and Gujarat have the highest prevalence, while other states like Punjab, Haryana, and Maharashtra are moderately affected. The document discusses the agent factors, host factors, and environmental factors that influence fluorosis prevalence. It also describes the clinical manifestations of dental fluorosis in children and skeletal fluorosis in adults. Various methods for defluoridating drinking water at the household level are presented. Commonly fluorinated drugs and food supplements are also listed.
![• Corticosteroids: Prescribed for severe pain
• Prednisone
• Cortisone
• Acetaminophen (nonsteroidal anti-inflammatory plus
antipyretic [lowers fever])
• Tylenol
• Liquiprin
• Datril
• NSAIDs (Nonsteroidal anti-inflammatory)
• Motrin
• Advil
• Aspirin
• Indocin
• Ibuprofen
• Excedrin
• Midol
• Nuprin
Kuldeep Vyas M.Sc. CHN
39](https://image.slidesharecdn.com/fluorosis-kdv-220305134054/85/Fluorosis-39-320.jpg)